by
Mindfulness assists people with their end of life process by giving them and their caregivers a tool they can use in order to be fully aware of the present moment and their own physical and mental states
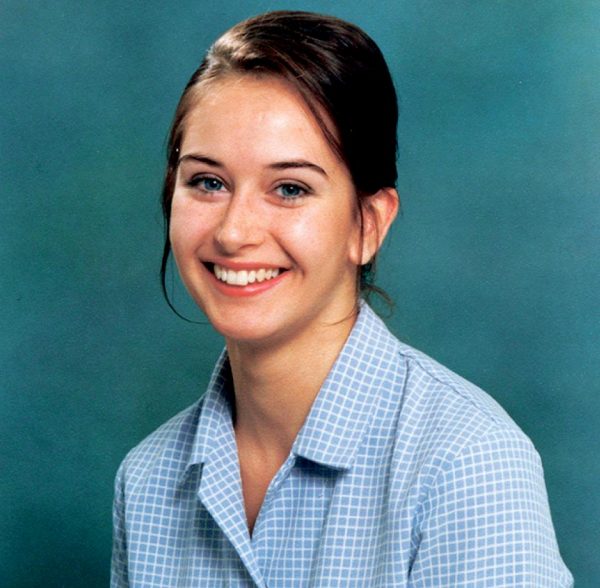
[T]he Venerable Yin Kit (pictured above) has spent decades in hospitals, hospices, and homes, assisting people through their death. Through these experiences, her understanding of how to compassionately and wisely care for those dying and their families has changed as a result of constantly reflecting on what she experiences and what she learns as a Buddhist nun living in the West in the 21st century.
The end of life is a transformation from one physical existence to another existence. Similarly, mindfulness is a transformation of one mental existence into another mental existence.
Emphasis on mindfulness
Buddhist teachings have always emphasized the contemplation of death; a subject that engenders so much fear and worry for many. Mindfulness can take on a role that compliments advanced medical technology in end of life (EOL) care.
Mindfulness assists people with their end of life process by giving them and their caregivers a tool they can use in order to be fully aware of the present moment and their own physical and mental states. This allows them to settle into each moment and open up to a wider vision of the future.
With mindfulness, a dying person not only sees their physical changes, but also how their mind influences the perception and experience of their waning body. With an aware and balanced mind, a person is more able to cope with the vicissitudes and challenges that come with this stage of life and be at peace with these experiences. This in turns greatly helps to console the family, friends and care-givers.
Mindfulness also assists in opening pathways for healing relationships and positive life reviews. One can be more receptive and capable of planning for, dealing with and understanding the constantly changing physical and mental experiences and in the end, one’s own death.
The role of mindfulness in end of life care

Venerable Yin Kit spoke about the role of mindfulness in end-of-life care at Simon Fraser University’s Vancouver campus on November 3, 2016. She was also a participant in a “praxis panel” that included Rabbi Laura D. Kaplan, veterinarian Dr. Jeff Berkshire, and counselor Hilda Fernandez.
Venerable Yin Kit, also known as “Sister Jessie”, has been a Buddhist nun since 1992 and is the spiritual leader of Po Lam Buddhist Association in Chilliwack, B.C. She is involved in leading numerous workshops teaching hospice care and hospital spiritual care in Hong Kong and in Canada. The Venerable is also the advisor to the Hong Kong SPGA Hospice program.
In 2005, Venerable Yin Kit established the Compassionate Centre for Health, a service for the Chinese-speaking community in the Greater-Vancouver area. This group has grown to over fifty active volunteers who visit senior homes and palliative care units at several sites. The Venerable has spent decades in hospitals, hospices, and homes, assisting people through their death. Through these experiences, her understanding of how to compassionately and wisely care for those dying and their families has changed as a result of constantly reflecting on what she experiences and what she learns as a Buddhist nun living in the West in the 21st century.

on the Praxis Panel at The End of Life: Dying, Suicide, Death (November 2016)
The End of Life: Dying, Suicide, Death
Simon Fraser University’s Institute for the Humanities hosted a conference in November 2016 called The End of Life: Dying, Suicide, Death. The conference was intended to provide space for pondering the complex and agonizing decisions regarding the end of life. Space for such conversations is especially needed given the 2015 decision of the Supreme Court of Canada declaring that the prohibition on physician-assisted dying infringes upon Section 7 of the Canadian Charter of Rights and Freedoms, and the introduction of Bill C-14 which has resulted in debate about who, when and in what circumstances an individual may make such a decision.
Speakers included academics, graduate students and practitioners who spoke from their own particular perspectives: legal, ethical, medical, and spiritual or religious. The presentations also drew upon insights from literature and art, some of humanity’s most treasured resources.
Complete Article HERE!