by Richard C. Gross
[W]hen I once conveyed concern to my father about his eventual death, his matter-of-fact response was, “We all die.”
And he did. At 89, of complications of pneumonia. Some say it was the best way to greet the hereafter: He went to sleep, into a coma, helped by doctor-administered doses of morphine. Yet when the ambulance initially came for him at the assisted living facility, his light brown eyes widened with fear.
I’m deathly afraid of dying. The idea of no more Richard weighs on me the older I get, and I’m getting up there. There’s so much more to do, so many more people to meet, so much to see, so much to live for, so much more to know. But there is no cure for aging.
I learned my fear of dying is not irrational; I have lots of company.
“Death is still a fearful, frightening happening, and the fear of death is a universal fear even if we think we have mastered it on many levels,” wrote Swiss-American psychiatrist Elisabeth Kübler-Ross in her seminal 1969 book, “On Death and Dying.”
Cultural anthropologist Ernest Becker, in his Pulitzer Prize-winning 1973 book, “The Denial of Death,” writes that “anxiety about death is a constant fact of life for everyone and that it is the underlying cause of the many other fears and phobias people experience.” Fears of being alone or stuck in a confined space, for example, are substitutes for fear of death.
Maybe singer Neil Diamond, now 76, expressed those very fears in the lyrics of his 1971 song about loneliness, “I Am … I Said:”
“But I got an emptiness deep inside/And I’ve tried/But it won’t let me go/And I’m not a man who likes to swear/But I never cared/For the sound of being alone.”
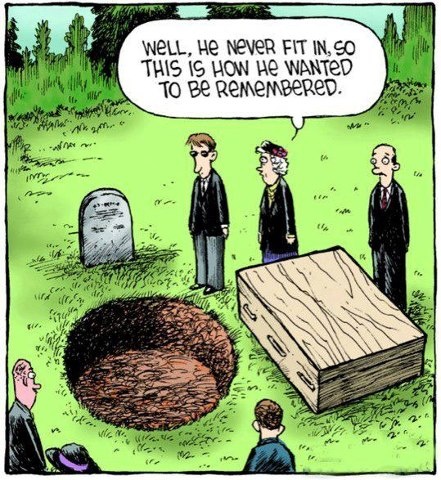
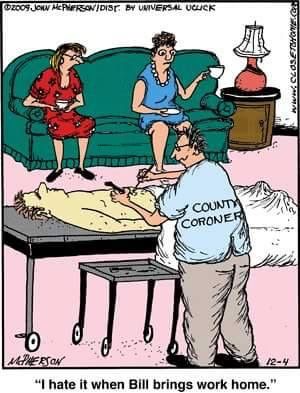
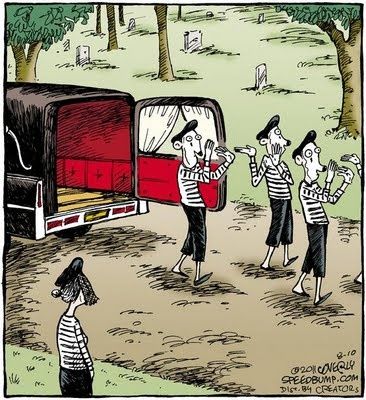
Alone or not, one’s mortality and the inevitability of death becomes more real the older we get, especially as relatives, friends and onetime coworkers — people with whom we’ve spent many years — die, shrinking our world, reminding us with a jolt that one day we will join them. Attending funerals becomes commonplace.
Seeking others for opinions about the fear of death, I attended a 90-minute seminar, called “Santa Fe Doorways,” hosted by Denys Cope, a registered nurse for nearly 50 years, including about 30 of them in hospice care. About 30 elderly people attended, all but three of them women; we sat in a wide circle in a windowless room in a retirement home.
Ms. Cope said, “We are all hard-wired to fear death,” and threw out a question: “When you think about death, what matters to you most?”
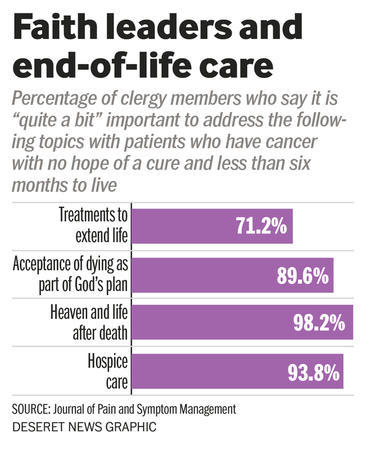
“To be able to die resting in God’s mercy,” replied one woman, acknowledging she is Christian.
Deep faith in one’s religion must be potently comforting, providing virtually certain assurance of peace as death approaches, perhaps, as another woman said, because of an abiding belief in an afterlife. Enviable. And for the secular among us?
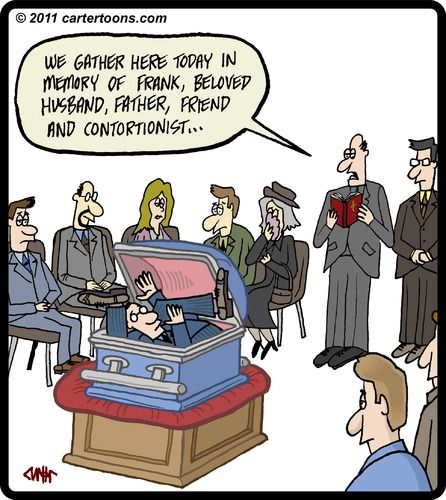
One white-haired man, who experienced a near-death episode, approached the subject lightheartedly, maybe because he appeared so organized. He said he since has written his own obituary, letters to his loved ones and has paid for his cremation. This is a man who will meet his maker head-on.
Another woman took an amazingly positive approach toward death, reveling in its opposite: life.
“What I love about death is thinking how I’m going to live,” she responded to Ms. Cope’s question.
I’m not as sanguine and stubbornly turned back to Becker’s “Denial of Death” to reinforce my feelings about dying. For me, he hit a bull’s eye:
“This is the terror: to have emerged from nothing, to have a name, consciousness of self, deep inner feelings, and excruciating inner yearning for life and self-expression — and with all this yet to die. It seems like a hoax.”
Ms. Cope has another way of looking at death.
“When first faced with the fact they are dying, many people experience a tremendous amount of fear,” she wrote in her 2008 book, “Dying: A Natural Passage.” “Often, I am told, it is not death but the process of dying that is frightening. … As long as we remain attached to this world and to our life, it is a struggle to die. … When we surrender to the process of dying, there is an incredible inward flow of peace and grace.”
I hope I can surrender.
Complete Article HERE!