Herman Feifel, pioneering figure in the modern death movement
American psychologist Herman Feifel was born in Brooklyn, New York, on November 4, 1915. He is internationally recognized as a pioneering figure in the modern death movement. His personal and research efforts helped break the prevailing taboo that discouraged scientific study of death and dying. His work transformed the way people think about death, treat the dying and bereaved, and view their own lives.
Feifel was educated in the New York City school system. His interest in psychology was stimulated during his undergraduate years at the City College of New York by John Gray Peatman, and later by Irving Lorge at Columbia University, where he received his master of art’s degree in 1939. World War II became a reality before Feifel could finish his doctorate. He enlisted in the Army Air Corps (now, the Air Force) in 1942, where he worked first as an aviation psychologist and later as a clinical psychologist treating combat soldiers overseas. While assigned to the Island of Tinian in 1945 he watched the Enola Gay take off to bomb the Japanese city of Hiroshima, an event that ushered in the age of atomic warfare. Feifel later reflected that this event and the death of his mother in 1952 were the two most important influences that catalyzed his interest in thanatology.
When the war ended Feifel resumed his studies at Columbia University, and finished his doctorate in 1948. He joined the Winter General Veterans Administration (VA) Hospital/Menninger School of Psychiatry group in Topeka, Kansas, in 1950, an event that marked the beginning of a long and illustrious association with the VA.
In 1954 Feifel accepted an invitation to join the Los Angeles VA Mental Hygiene Clinic. In 1960 he assumed the position of chief psychologist, an office he held until his retirement in 1992. Since 1958 he has additionally held an appointment at the University of Southern California School of Medicine, where he is emeritus clinical professor of psychiatry and the behavioral sciences.
Feifel’s dissatisfaction with psychology’s neglect of the existential richness of life, including the everyday matters of death and dying, coalesced in the 1950s. A major consequence was his focus on what has since become known as the field of thanatology. In 1959 he edited the book The Meaning of Death, which authorities agree was the single most important work that galvanized the scholarly community concerning dying, death, and bereavement. In this and related areas (e.g., gerontology, personality, psychotherapy, religious experience) his publications encompass more than 125 articles and chapters, as well as two books. Many of his literary contributions are focused on dispelling myths held by scientists and practitioners about death, the most injurious of which is a denial of its importance for human behavior.
Feifel’s empirical contributions are most influential in the areas of death attitudes, death anxiety, and coping with life-threatening illness. By the late 1990s scholars identified over 1,000 published studies in these areas, and recognized Feifel as being the only person to contribute seminal papers in five consecutive decades. He shaped the direction of this research by arguing for reliable and valid measures that acknowledge the multidimensional, multifaceted nature of death attitudes and fears, the importance of death attitudes in shaping a wide variety of behaviors, and the need to study death issues among those actually facing life-threatening circumstances. His research demonstrated that fear of death can exist differently on conscious and nonconscious levels, and helped establish that people may use different coping strategies when faced with life-threatening versus non-life-threatening situations.
For his work in thanatology, Feifel has received numerous accolades, including an honorary doctorate from the University of Judaism (1984), a Distinguished Death Educator Award (1990), the Distinguished Professional Contributions to Knowledge Award by the American Psychological Association (1988), and a Gold Medal for Life Achievement in the Practice of Psychology by the American Psychological Foundation (2001).
Complete Article HERE!
A world too big, a time too brief
Embracing Death for Ourselves and Our Patients
I have the honor of having an essay of mine published on NurseTogether today.
“I want to celebrate my belief that living well and dying well are one and the same thing. I’m not talking about adjusting deathbed pillows so that the dying people can strike heroic poses for the edification of onlookers. I’m talking about achieving a good death in the context of real dying – with all its unpredictability, disfigurement, pain, and sorrow.”
My name is Richard. I’m the founder of PARADIGM/Enhancing Life Near Death, a nonprofit organization with an outreach to terminally ill, seriously ill, elder, and dying people. I’m also the author of the newly published The Amateur’s Guide To Death And Dying. I’ve been invited to share some thoughts with you about my personal journey on patient deaths.
Although I’ve been working in this field for 30 years, I should probably say from the onset that witnessing patient deaths is not something I chose to do. It was more like this work chose me. Let me explain.
I finished my doctorate in San Francisco in 1981. That same year a mysterious thing began to happen. Gay men all across the country began to sicken and die from an unknown disease. Was this a diabolic plot of some kind? Perhaps it was divine retribution. Or was this simply a very serious medical emergency? The AIDS crisis had begun in earnest.
Because of my background in religion and psychology, friends turned to me for guidance, but I’m afraid that I had nothing to offer them. Nothing, in all my years of schooling, had prepared me for what was happening to the people I loved. I was petrified. All my greatest fears were being realized. What did it all mean? It was a desperate time and I was powerless. I could do nothing but sit and watch the nightmare unfold.
As it turned out, sitting and watching was the best thing I could have done, because as fate would have it, this time I was to be the student, not the teacher. In time, I became less anxious. The monstrous thing I feared for so long was being transformed. I was able to sit with death and not be afraid. Death was no longer the enemy, she had become what St. Francis called her, ‘sister death.’
Years of going from one death scene to another with hardly a break in between was exhausting but also rewarding. I began to see patterns develop. Despite the uniqueness of each death, I noticed there were two things all these deaths had in common. They were difficult and lonely affairs.
Difficult because in this culture we have a hard time recognizing when things are over, especially the things we enjoy – summer vacation, relationships, our youth and even life itself. This is a problem because being unable to acknowledge the end of something makes saying goodbye and thank you impossible.
And they were also lonely affairs, because the wisdom people come as they approached the end of their life often died with them. There simply wasn’t a medium for collecting this abundant wisdom and thus it was frequently lost.
Most people face their mortality in a vacuum of information and support. It is as if each of will have to learn to die from scratch, as if no one had died before us.
I figured there had to be a better way to deal with this fundamental fact of life. That’s why I’m here. I want to take a fresh look at my mortality, and do so in an interactive and positive way.
I look forward to other opportunities to address the topic of patient deaths and even dying as a personal issue in the weeks to come. Thank you for this opportunity to join you.
Complete Article HERE!
Hump Day Humor
Was your week as grueling as mine? Well I have the antidote.
HAPPY THANKSGIVING!
Beyond “The Sessions”: Intimacy at end of life
I did a little follow-up interview with the wonderful people at Life Matters Media.
November 16, 2012
Beyond “The Sessions”: Intimacy at end of life
Dr. Richard Wagner
Dr. Richard Wagner, a Seattle based clinical sexologist, spoke with Life Matters Media this week about the many positive effects physical intimacy may have on the terminally ill. As the critically acclaimed film The Sessions has brought this topic to the forefront, it has left in its wake many issues in which to delve deeper. Wagner, a former Roman Catholic priest, is the author of “The Amateur’s Guide to Death and Dying: Enhancing the End of Life.” He has practiced sex therapy and relationship counseling for more than three decades.
You have a degree in theology from the Jesuit School at Berkeley, and you’re a former priest. How did you get involved with end of life and intimacy?
I was a Catholic priest for 20 years. While that wasn’t a particularly happy association, I’m the only Catholic priest in the world with a doctorate in clinical sexology. I wrote my doctoral thesis on the sexual attitudes and behaviors of gay priests in the active ministry in 1981. That was long before the Church was willing to acknowledge there was even such a thing as a gay priest. The fallout from this research blew my ministry out of the water.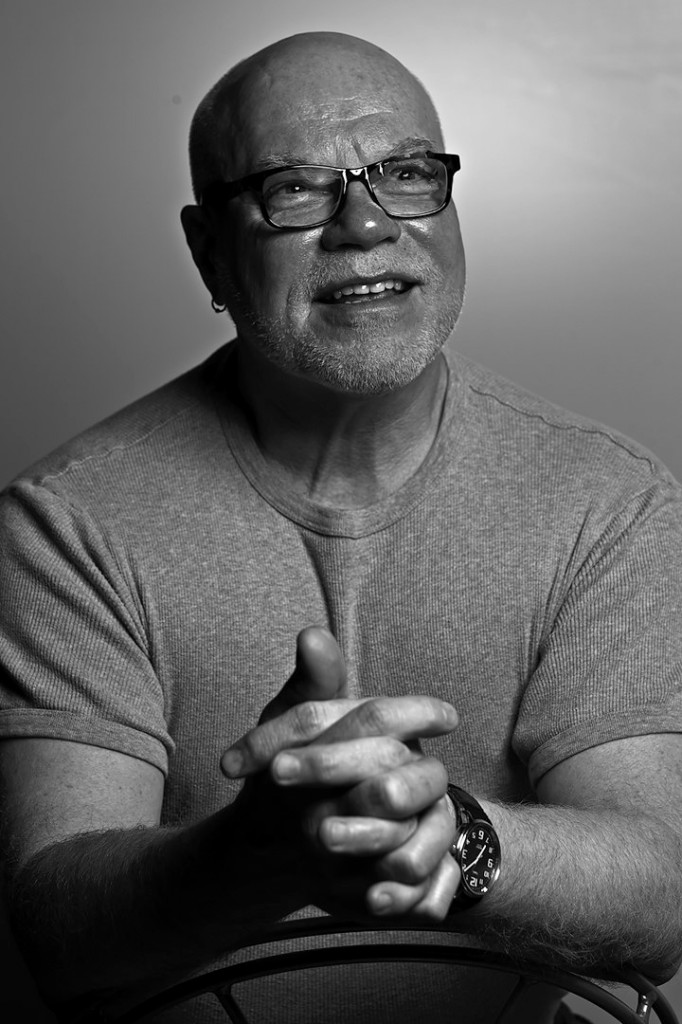
In 1981, the same year I finished my doctorate, a remarkable thing was happening to gay men in San Francisco and elsewhere. They were dying of some mysterious disease. Some speculated that this was God’s retribution for the gay lifestyle. How quickly we leap to that conclusion when we are ashamed and frightened. Most of my friends died in the first wave, between 1981-85. None of us knew what to do. My friends looked to me for guidance, since I had a background in psychotherapy and religion. But, to tell you the truth, I was just as lost as anyone.
I found myself sitting with all these men as they were dying. It was ghastly. But sitting with death was precisely what I needed to do. It helped me to desensitize death and prepared me for what was to come. I realized early on that dying in America is often a very lonely and very passive affair.
I wrote “The Amateur’s Guide” because of the work I was doing with sick, elder and dying people – not just AIDS patients. I saw this pattern develop; the end of life is more difficult than it needed to be. In response I founded Paradigm, a nonprofit organization with an outreach to enhance life near death for sick, elder, and dying people. It provided an opportunity for participants to discuss end of life concerns and get the support they needed to fully live the end of their life. The program was so successful; I decided to put the program in book form.
Let’s talk about intimacy and end of life care.
Just because someone is dying doesn’t mean that they have stopped being human. One of the things that humans need in their life is intimacy. And sometimes that intimacy involves genital sexuality. But this concern is hardly ever talked about in terms of the end of life, nor is it included in disease-based discussions. I mean, when is the last time you heard someone talk about the sexual concerns of people with cancer or heart disease? Our culture is uncomfortable with the concept of sick, elder, and dying people having such desires. But if you listen to these folks they’ll tell you what they need and ho difficult it is to live without.
Could sexual intimacy be considered a form of palliative care?
I would think, yes. If you’ve had an active intimate/sex life up until the point you were diagnosed and then all that suddenly disappears, there will be problems. I’m not just talking about genital sexuality; I’m talking about all intimacy needs we humans have — being present to, touching, as well as pleasure. It’s all about what is possible, on a personal level, with one’s intimate partner(s). So many people, even people who love sick, elder, and dying people don’t know how to touch them. And sick, elder, and dying people often report that the only touch they receive is very clinical touch. And that’s not all the life affirming, if you ask me.
Complete Article HERE!
End-of-Life Care Should Be Universally Provided and Need-Based
By James Hamblin, MD
Dr. Ezekiel Emanuel, oncologist and chair of the Department of Bioethics at the National Institutes of Health (and, entirely incidentally, brother to Rahm and Ari Emanuel) has long been a champion of end-of-life care. He spoke today with Corby Kummer at The Atlantic’s Washington Ideas Forum, where he made succinct points about strategies for systematic improvements in our approach to caring for those nearest to death.
 First, all doctors and nurses should be formally trained in end-of-life care and discussions. Walking into a room with a patient and their family to discuss a terminal diagnosis or prognosis is — especially at first — overwhelming, and impossible to just know how to do. Emanuel admits that facing those situations remains “scary,” even as a veteran clinician. He and most of his generation of physicians never received formal training in how to best discuss terminal illness with patients and offer palliative options, and some in training today still do not. Considering the large number of people who eventually face death, it is unreasonable that not all doctors and nurses are thoroughly prepared to help them as they do.
First, all doctors and nurses should be formally trained in end-of-life care and discussions. Walking into a room with a patient and their family to discuss a terminal diagnosis or prognosis is — especially at first — overwhelming, and impossible to just know how to do. Emanuel admits that facing those situations remains “scary,” even as a veteran clinician. He and most of his generation of physicians never received formal training in how to best discuss terminal illness with patients and offer palliative options, and some in training today still do not. Considering the large number of people who eventually face death, it is unreasonable that not all doctors and nurses are thoroughly prepared to help them as they do.
Emanuel also cited that more than 40 percent of hospitals in the U.S. do not offer access to palliative care, either within the hospital or after a patient has been discharged home. He believes that hospitals should be required to at least offer the option.
And finally, at present, eligibility for hospice care is predicated on having six months to live. Emanuel sees access to hospice as more aptly need-based, not calendar-based. Patients with symptoms warranting palliation, regardless of the estimated length of their remaining life, should be standardly offered care in that vein.
All of these changes would come as part of an ongoing shift in psychology and broader openness about death. Emanuel is quick to add the caveat that he is not talking about euthanasia or [shudder] … “death panels.” His inclination toward explicit clarification on that point stems from accusations that he and other leaders in the realm of end-of-life care have endured in the past. The fact that he still needs to make that clarification speaks to the persistent widespread misunderstanding surrounding quality end-of-life care. That mindset is and will remain the primary barrier to seeing these improvements out.
Complete Article HERE!