The critical role of talking with a doctor about values and priorities in life—at any age
At 30 years old, a person’s brain weighs about three pounds. In its capaciousness it wears the skull like a well-tailored suit. So notes Harvard professor and surgeon Atul Gawande in his most recent book Being Mortal—only to contrast that with the fact that by age 70, there is usually about an inch of space between the brain and the skull. And that’s not because the skull is expanding. From just a glance at a CT scan of a person’s brain, a radiologist could venture a pretty good approximation of the person’s age.
 That’s not to say that loss of brain volume means that most people don’t retain enough grey matter to remain brilliant in old age. (Over the last 20,000 years, the average human brain has gotten smaller by about the size of a tennis ball, which doesn’t mean we’ve gotten dumber.) Instead it’s—like the recession of gums from teeth and the exhaustion of the stem cells that give hair its pigment—a vivid example of the normal aging of the human body.
That’s not to say that loss of brain volume means that most people don’t retain enough grey matter to remain brilliant in old age. (Over the last 20,000 years, the average human brain has gotten smaller by about the size of a tennis ball, which doesn’t mean we’ve gotten dumber.) Instead it’s—like the recession of gums from teeth and the exhaustion of the stem cells that give hair its pigment—a vivid example of the normal aging of the human body.
Together these changes illustrate, Gawande writes, that the end process is often really not the body wearing down so much as gradually shutting down. It’s a process that doctors are trained to resist and “fight,” leading a patient into “battle” with disease. Though, the analogy falls apart in that a battle with death can’t be won; Philip Roth once said that old age is less a battle than a massacre. And, as Gawande notes, a good general is not one who leads an army to the point of total annihilation.
Being Mortal, which was published in October, is ostensibly about the struggle to cope with the constraints imposed by flesh-and-bone biology—and the failure of medical science to acknowledge that any ability to push back is finite. Gawande’s ultimate message, that death in America is not often enough discussed, and that patients suffer at the hands of well-meaning doctors because of it, has been generally celebrated, though not for breaking particularly new ground. His is the basic message for which the late surgeon Sherwin Nuland’s How We Die won a National Book Award 20 years ago; and it’s the message of another book released last week, The Conversation, by another Harvard physician, Angelo Volandes. It’s a message that has grown extremely loud inside of the health-professional echo chamber, but is somehow still only faintly reverberating into broader culture.
“I think too many people don’t know what’s going on behind those closed doors in  hospitals,” Volandes told me. “But if they did, they’d be outraged. So many people are getting—not costly care—I’m talking about unwanted care.”
hospitals,” Volandes told me. “But if they did, they’d be outraged. So many people are getting—not costly care—I’m talking about unwanted care.”
It’s a point that Volandes himself has made many times in the past decade (ever since he was a medical student under Nuland at Yale), which may account in part for his bursts of highly polished, nightly-news-style phrasing: “If people were more informed about their options, they wouldn’t want a lot of the ‘medical care’ that they end up getting in our hospital system today.”
Now Volandes sees his work as a sort of “part two” to Gawande’s book, in that he goes an extra step to tell people exactly how to raise the subject of death—in the context of personal values and life priorities—with their doctors. Because if a patient does not start the conversation, and insist on a quality understanding, it is unlikely to happen.
In order to become a board-certified physician in his residency training at the University of Pennsylvania, Volandes writes, “I was required to prove my competence with inserting central line catheters, leading Code Blues, performing lumbar punctures, drawing blood, and obtaining arterial blood-gas samples. But not a single senior physician needed to certify that I could actually speak to patients about medical care.”
 Now a hospital-medicine specialist at Massachusetts General Hospital, Volandes has very rarely inserted central lines or performed many of these procedures since his residency. But, of course, he speaks with patients and families daily. He notes that while medical students and resident physicians today are being trained in end-of-life counseling, most doctors currently in practice graduated medical school before palliative care was ubiquitous, and before The Conversation (he capitalizes the term throughout the book, capturing the importance of talking about death, but also making it seem daunting) was a part of curricula.
Now a hospital-medicine specialist at Massachusetts General Hospital, Volandes has very rarely inserted central lines or performed many of these procedures since his residency. But, of course, he speaks with patients and families daily. He notes that while medical students and resident physicians today are being trained in end-of-life counseling, most doctors currently in practice graduated medical school before palliative care was ubiquitous, and before The Conversation (he capitalizes the term throughout the book, capturing the importance of talking about death, but also making it seem daunting) was a part of curricula.
“Practicing doctors are a tough group to try and train,” he told me. “That’s what we’ve been trying to do for the past 10 years, and we’ve barely moved the needle. I have much more faith in patients bringing this conversation to doctors than waiting for doctors.”
And so he makes it straightforward, telling people exactly what a good Conversation should involve: How important is it to you to live as long as possible, even if it means that you would experience pain and suffering? Would you want to avoid pain at all costs, even if you might not be able to interact with others? How important is it to you to be at home when you die?
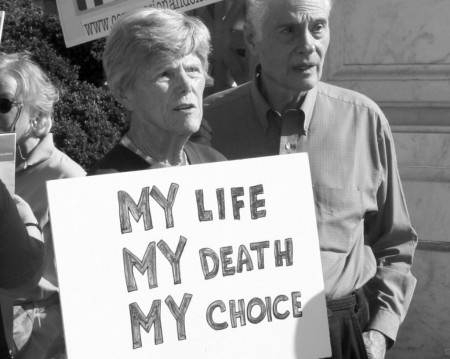
“When you ask most people where they want to die,” Volandes said—referring, of course, to people who have some context for the nature of the question—”most people say, I want to die outside of the hospital, in my home, in comfort.”
Nearly 80 percent of Americans, in fact, say that. And yet, close to 55 percent of older adults die in a hospital or nursing home. Fewer than one in four manage to die at home. Why does this discrepancy persist?
* * *
 The American approach to death in the past century has followed an arc not unlike our approach to food. One of the most common pieces of advice given by nutrition experts today was coined by Michael Pollan: “Eat food. Not too much. Mostly plants.” But amid war and scarcity in the early and mid nineteenth century, producers flaunted triumphs science in food processing and preservation—in their capacity for synthetic tastes, bright colors, and infinite shelf lives. Wonder Bread, Tang, Spam, Velveeta, perfection salad, and Twinkies were created not because they should have been created, but because they could be created. They were cheap and delicious; God bless the land of plenty.
The American approach to death in the past century has followed an arc not unlike our approach to food. One of the most common pieces of advice given by nutrition experts today was coined by Michael Pollan: “Eat food. Not too much. Mostly plants.” But amid war and scarcity in the early and mid nineteenth century, producers flaunted triumphs science in food processing and preservation—in their capacity for synthetic tastes, bright colors, and infinite shelf lives. Wonder Bread, Tang, Spam, Velveeta, perfection salad, and Twinkies were created not because they should have been created, but because they could be created. They were cheap and delicious; God bless the land of plenty.
It was decades later that the the “real food” movement supplanted the virtue of processed foods, favoring anything natural (or at least appearing to be of nature). Part of that shift was due to advances in agriculture and transportation making natural-food access possible, but an even larger part was consciousness of nutrition and health. For many people, the central questions of consuming food shifted away from “Can we?” and toward “Should we?” Nearly in step, those were the questions facing doctors in a culture that tended to pursue aggressive medical therapies for people near the end of their natural lives by default.
As Gawande tells the story, in the 1940s, almost everyone died at home. But by the late 1980s, a mere 17 percent of people did. That shift was partly due to tremendous scientific advances that transformed the hospital from a place of very few effective treatments, to a place that had intravenous antibiotics, heart surgery, and kidney transplantation. By the latter part of the century, a doctor could do something for almost anyone (or rather, almost any medical condition), and hospitals became places not of resignation, but of hope. In 1946, the Hill-Burton Act provided government funding for widespread hospital construction. For the moderately and seriously ill, going to a hospital became the default.
 And so people died fighting. They died fighting even when the fight was futile. They died on sterile wards with electrodes taped to their chests and tubes in orifices both natural and manmade. They died deprived of sleep and good food and all things familiar. They died in uniform gowns, whose singular purpose is accommodation of gastrointestinal processes. And worst, they died the way they most likely wouldn’t have wanted to die. Most of those cases could have been, and could now be avoided, Volandes argues, if doctors and patients would just have The Conversation.
And so people died fighting. They died fighting even when the fight was futile. They died on sterile wards with electrodes taped to their chests and tubes in orifices both natural and manmade. They died deprived of sleep and good food and all things familiar. They died in uniform gowns, whose singular purpose is accommodation of gastrointestinal processes. And worst, they died the way they most likely wouldn’t have wanted to die. Most of those cases could have been, and could now be avoided, Volandes argues, if doctors and patients would just have The Conversation.
The dilemma of modern medicine, in the era of tremendous medical capabilities—when almost any person can be kept alive well past the point when they would have otherwise died (and, in some cases, after they did die)—is, when are health professionals missing the point? When does care become, to use the word Volandes and Gawande do in their lived stories, torture? Because it is a very rare case now, when there is nothing more that doctors can do.
In recent years, the trend has slowly begun to reverse. Since 1990, more and more Americans have died the way they wanted. By 2010, 45 percent of Americans died in hospice care—most of them at home. The rates, among the highest in the world, are what Gawande calls a “monumental transformation” away from a “miserable” system perpetuated by tradition and familiarity. But this remains, he believes “an unsettled time.” In our 21st-century approach to dying, “We have begun rejecting the institutionalized version of aging and death, but we have not yet established our new norm.”
Both of these authors invoke a balance of ominous warnings and messages of empowerment—taking control of your medical care, flipping the patient-doctor power dynamic, living life on your own terms, et cetera. Any discussion of finances, of the prudence of pouring limited resources into the marginal life-prolonging of terminally ill people, has become so politicized that it is no longer grounds for productive discussion.
Both authors focus instead on optimizing communication between doctors and patients. Patients can drive change with knowledge of their options, and doctors by communicating those choices—and guiding the decision with insight from experience. Both authors take a familiar narrative tack, following the stories of seriously ill patients for whom they’ve cared, and the vastly different courses that those people’s lives take according to whether they had discussed life priorities. Both authors contrast things they’ve done to their patients with what they would want done for themselves or their loved ones—a point of too-frequent discrepancy. Both authors depict, too, the vast discrepancy between the medical care that most people say they want and the care they actually receive.
Once patients understand the realistic odds that they will benefit from aggressive medical therapies in dire circumstances—and just how painful and debilitating it can be to go through some of the things that can be done to keep a person’s heart beating in a modern intensive care unit—research shows that most people become less likely to pursue the same course. And in one large study Gawande cites, patients even ended up living just as long when they went into hospice care as did their aggressively medicalized counterparts. Of 4,493 people studied, the researchers concluded, mean survival after three years was actually 29 days longer for hospice patients than for non-hospice patients.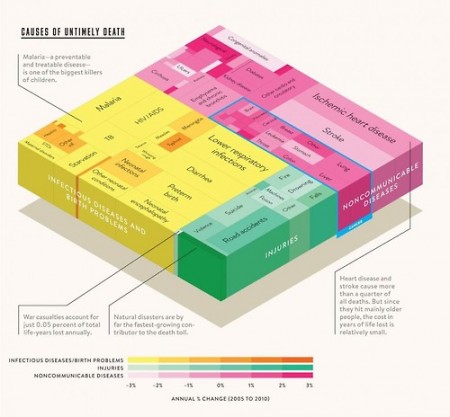
If every patient knew those numbers—that care aimed at prolonging life is often so far from a guarantee of anything but discomfort—would so many people still end up dying they way they didn’t want?
“I think eventually we have to accept the fact that talking about end-of-life care is a fundamental part of what it means to be a good clinician,” Volandes told me, if only to ensure that patients are aware of the limitations and drawbacks of invasive life-prolonging measures. To that end, he has also created a series of free videos (which were the subjects of a 2013 story in this magazine) to help patients understand exactly what certain medical routes entail, to supplement discussions among family and with doctors.
In one attempt at forcible change in culture, Massachusetts recently passed a law requiring hospitals to present advanced-care planning materials and discussion to patients. Volandes is cautiously optimistic, believing it remains to be seen how well this sort of regulation will work. A requirement for conversation does not guarantee a quality conversation.
 When I was a medical intern in Boston in 2010, our hospital had orange “code sheets” that we had to put on the very first page of every patient’s chart (we were still using handwritten paper charts for all medical records in 2010, in a Harvard hospital). The orange sheet had to specify whether the patient, should they die in our hospital, wanted to undergo cardiopulmonary resuscitation or not. My job as the lowest doctor on the totem pole was to make sure one of the two boxes was checked, for every patient at all times. Which meant some kind of conversation. But it was rarely good and meaningful. These were people I just met, and I constantly had a million people paging (paging) me with more urgent (if less important) concerns. Unless I foresaw that someone might quite likely die during their stay, and their stated wishes seemed at odds with my medical prerogative on a conscionable course of action, then what should have been a proper conversation was much more often, regrettably, a hurried checking of a box.
When I was a medical intern in Boston in 2010, our hospital had orange “code sheets” that we had to put on the very first page of every patient’s chart (we were still using handwritten paper charts for all medical records in 2010, in a Harvard hospital). The orange sheet had to specify whether the patient, should they die in our hospital, wanted to undergo cardiopulmonary resuscitation or not. My job as the lowest doctor on the totem pole was to make sure one of the two boxes was checked, for every patient at all times. Which meant some kind of conversation. But it was rarely good and meaningful. These were people I just met, and I constantly had a million people paging (paging) me with more urgent (if less important) concerns. Unless I foresaw that someone might quite likely die during their stay, and their stated wishes seemed at odds with my medical prerogative on a conscionable course of action, then what should have been a proper conversation was much more often, regrettably, a hurried checking of a box.
Even when there is time for an extensive conversation with a familiar physician, there will always be nuances and circumstances that cannot be predicted—which is fine. The point is not to deliberately lay out everything you might want done in every possible scenario. It’s to consider the basics of what is important to you in life, so that your family and medical team can make sure you get the care that aligns with those goals.
As Gawande writes in his epilogue, “[Doctors] think our job is to ensure health and survival. But really, it is larger than that. It is to enable well-being. And well-being is about the reasons one wishes to be alive.”
Complete Article HERE!











/cdn0.vox-cdn.com/uploads/chorus_asset/file/2400318/sidebar-image__1_.0.jpg)
/cdn0.vox-cdn.com/uploads/chorus_asset/file/2919162/gawande_chart_1.0.png) (Metropolitan Books)
(Metropolitan Books)/cdn0.vox-cdn.com/uploads/chorus_asset/file/2919212/gawande_chart_2.0.png) (Metropolitan Books)
(Metropolitan Books)/cdn0.vox-cdn.com/uploads/chorus_asset/file/2919148/vox-share__43_.0.png)
/cdn0.vox-cdn.com/uploads/chorus_asset/file/2919326/Screen_Shot_2015-01-09_at_10.43.30_AM.0.png)
/cdn0.vox-cdn.com/uploads/chorus_asset/file/2920092/vox-share__51_.0.png)