— Ben Griffith’s dad chose a method to end his life that was controversial — but protected by a Supreme Court ruling
By John Rosengren
1990: The right to refuse medical treatment
Ben Griffith rose before the sun the morning of March 18, 2022, packed his car and began the long drive from his house in Frankfort, Ky., to suburban Kansas City, Mo. The time had come to help his father die.
Months earlier, when John Griffith made clear to his three sons that he would end his life by denying himself food and drink rather than go into an assisted-living facility, his two older sons objected. Only Ben, the youngest at 67, agreed to keep vigil with his 99-year-old father. Now that John’s quality of life had deteriorated to the point where he would rather die than have his misery prolonged with unwanted treatment in assisted living, Ben was heading to his father’s house.
From their many conversations on the subject over the previous decade, Ben knew his father would have chosen the route of assisted suicide if it were legal in Missouri, as it is in 10 states and the District of Columbia. But it wasn’t. In September 2021, in a power-of-attorney directive, John had given his sons the authority, in the event that he was incapacitated, “to direct a health care provider to withhold or withdraw artificially supplied nutrition and hydration (including tube feeding of food and water).” Now, instead of assisted suicide, John had opted to voluntarily stop eating and drinking, a process known in right-to-die circles by the acronym VSED. The process generally takes between seven and 15 days. Because it can be painful, many who opt for it also seek palliative care through hospice services — which is what John Griffith did.
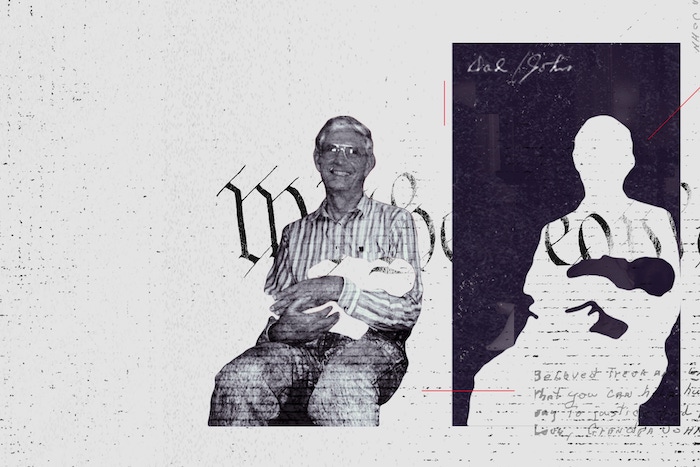
Seated at the kitchen table of his Frankfort home and surrounded by family photos, Ben recounts his father’s experience with life and death. (Ben participated fully in this article; his eldest brother, Tim, did not comment; his elder brother, Jon, offered this comment: “I just know that Ben did a great job representing the family and our experience of going through VSED with Dad. I don’t need to add anything more.”)
There’s a frost threatening that evening, so Ben and his wife, Patricia, have moved inside a dozen or so plants now safely perched along the kitchen counter. Ben, a piano tuner with short gray hair, is tall and lanky like his father, who was 6-foot-4. His words occasionally give way to emotion. His soft blue eyes, also like his father’s, are warm and kind.
John Griffith — born Dec. 12, 1922, in South Carolina, the son of a Methodist minister — was a man of such strong principles and resolve, he bordered on obstinate. Despite widespread public support for the United States’ involvement in World War II, Griffith at 19 opposed war “for any cause whatever” and refused to register for the draft, which he considered a “contradiction of Christian teachings, democratic liberty and individual freedom.” Instead, as he wrote in an essay for the book “A Few Small Candles: War Resisters of World War II Tell Their Stories,” he served 24 months in federal prison.
The influence of a Quaker attorney willing to defend him pro bono sparked John’s conversion to the Religious Society of Friends. After his release from prison, he attended William Penn College, a Quaker institution in Oskaloosa, Iowa, where he met and married Reva Standing. They raised four sons. Griffith spent his working career managing a farmers cooperative. When their oldest son, Chris, was murdered in 1986, Griffith stuck to his pacifist convictions and opposed the death penalty imposed on his son’s killer.
Reva suffered a stroke in 2003 and showed early signs of dementia in the hospital. Despite his belief that it was wrong to end another’s life in war or by capital punishment, John made the decision to honor her wishes and remove his wife of 56 years from life support in what he considered an act of compassion. “It was clear if she came home, there would be a loss of brain function,” Ben says. “He knew one of her biggest fears was living with dementia.”
Neither father nor son could bear watching a loved one suffer unnecessarily — a point driven home by the experience of Ben’s mother-in-law. In 2016, when Patricia’s 93-year-old mother began losing her sight, she moved into an assisted-living facility and eventually a nursing home after going completely blind. “She fell gradually into a shell,” Ben says. “Her existence was getting not very good.”
It was so painful for Ben to watch that he started searching online for ways he could end her life to put her out of her misery and not get arrested. But his father urged him not to do anything that would have negative consequences for his wife and their two adult children. Ben tears up at the telling. “I could have ended her life,” he says. “She suffered — but he said, ‘Don’t do it, Ben.’ ”
Her ordeal seemed to spark something in John. Already into his 90s by then, he began contemplating the end of his own life, which he discussed openly with his sons. Patricia’s mother’s situation “cemented the idea for him: If you go into assisted living, you lose a lot of choices,” Ben says. “If something happens, they call for help. You go to the hospital and they treat you. Same thing if you are in a nursing home. If you’re unresponsive, they are going to treat you.” John made it very clear that he did not want to go into assisted living or a nursing home.
A man as spiritual as he was stubborn, John had meditated daily for years, an hour or so at a time, an essential part of his religious faith and practice. He also swam a mile most every day at the local YMCA. At 90, he set eight state swimming records for nonagenarians on his daily swim, according to Ben. He had decided that once he could no longer swim, life would no longer be worth living and he would begin VSED. “He had identified the red line,” Ben says.
More from The Unwritten Rights Issue
John “had his last swim at 98,” Ben recalls. His “will to live” did continue, but he was losing physical strength. He was having trouble walking and would soon have to use a wheelchair. And he felt himself slipping cognitively. So that’s how he came to fill out his health-care directive in September 2021. With the help of Compassion & Choices, a nonprofit organization that advocates for access to aid in dying, he also filled out an advance directive addendum indicating his desire throughout various stages of dementia that others “keep me comfortable while stopping all treatments and withholding food and water so that I can die peacefully.”
That fall John discussed his VSED intentions with his primary care physician, who did not approve. The doctor tried to talk John out of the idea over the course of several visits. But John would not be dissuaded.
He informed his sons of his plans in a Zoom call. The two older sons protested. Tim, who had been his father’s primary caregiver, taking him to appointments and helping him at home, tried to persuade his father to move into assisted living instead, according to Ben. But their father refused. He would stay in the two-bedroom townhouse he and his wife had lived in for years and die by his own design. There was no talking him out of it. “If he was going to do something, he was going to do it,” Ben says.

Though Tim and Jon would visit, they did not want to be accomplices to VSED; Ben alone agreed to be with their father continuously throughout the process. “I felt it was an act of love,” Ben says.
In January 2022, John developed a cough. The prescribed medication he took for it made him confused, even after he stopped taking it. He had trouble focusing during his meditation. He began to notice “a sharp decline, both in memory and in my ability to make decisions,” he wrote in a letter to family, friends, neighbors and his spiritual community. In February, he was diagnosed with dementia.
Physically, he was also failing fast. He could no longer stand on his own. He needed the help of home health-care attendants using a lift device to get from his bed to his wheelchair and back again. He was outfitted with a catheter. By late February, his quality of life had sunk to the point of no return. “It’s exhausting to get through every day,” he explained in his letter. “I’ve had a good life. I think the time for VSED is now.” In another Zoom call with his sons, he told them the same. He eventually set March 19 as the date to begin his life-ending fast.
Ben and his brothers hired a hospice service to provide palliative care. But the assigned chaplain, a Catholic priest, said he could not in good conscience minister to someone committed to dying by their own doing. Another chaplain, who was not Catholic, took his place.
“While I agree with the Court’s analysis today, and therefore join in its opinion, I would have preferred that we announce, clearly and promptly, that the federal courts have no business in this field. … This Court need not, and has no authority to, inject itself into every field of human activity where irrationality and oppression may theoretically occur, and if it tries to do so it will destroy itself.”— Justice Antonin Scalia, concurring, Cruzan v. Director, Missouri Department of Health
Others objected, too. Some covertly, some overtly. His next-door neighbor did not disagree with his decision explicitly, though she did come over to read the Bible with John. “She wanted to make sure he was right with Jesus,” Ben says. Once John began the VSED process, Ben says, she stopped visiting.
A key word in the 14th Amendment’s due process clause is “liberty,” a concept that runs deep in the American psyche. “We think of it in terms of: Each individual person controls their own body, especially if you’re an adult and competent,” explains Rob Gatter, a professor at Saint Louis University’s law school and director of its Center for Health Law Studies. “It’s the same reason motorcyclists get mad when states say you have to wear a helmet: … I’m a competent adult and I don’t need the state to be my parent. I make choices for myself understanding if I’m wrong I suffer the consequences. My body does not belong to the state. My body belongs to me.”
Ben arrived at his father’s townhouse in Gladstone, Mo., about 3 o’clock the afternoon of March 18, having driven the better part of 11 hours. He had braced himself for the ordeal, knowing it could become more difficult if his father wavered and requested food or water. Ben could not deny him that. “It’s voluntary,” Ben says. “If a person wants food or water, you give it to him. I had done my homework with Compassion & Choices and read their list of guidance. It says remind the person, ‘Dad, you know you’re doing VSED. If you take ice chips or water, it’s going to delay the process.’ I prepared before I left for that.”
Ben found his father in good spirits. “I am convinced that there is something more: that human consciousness is independent of the body and that the death of the body is not an ending of consciousness — it is rather a passing,” John had written a couple of weeks earlier. “Into what? I confess that I do not know, but I have a deep, abiding trust in the Divine Ground of all existence that the major world religions have variously called God, Mind, Allah, Tao, etc. My parting wish for my friends is that they nurture compassion and walk humbly in the presence of Unfathomable Mystery.”
In addition to the hospice staff coming and going and a home-health caretaker on duty 24/7 beginning March 19, there was a stream of visitors to John’s house the first several days. Neighbors, fellow Quakers and other friends stopped by to spend time with him. John made small jokes at times and laughed with them. Tim and his family also visited. Tuesday, March 22, John was happy to see his son Jon, who arrived from Vermont. He had energy to send some emails. He spent half an hour being interviewed over the phone by someone from Compassion & Choices, which tired him out. The hospice team gave him a bath. Several times a day, Ben gave him the medications prescribed by the hospice nurse — Haldol to ease anxiety and hydromorphone to soothe pain — by squirting them into his mouth with a syringe.
By Wednesday, the fifth day of his fast, John was weakening. It was more difficult for him to get in and out of his wheelchair, even with the power lift. The hospice nurse added lorazepam to John’s list of medications to help him relax. The next day, Thursday, he was talking less, and when he did speak, he didn’t make much sense. He insisted on getting out of bed at one point, then drove his wheelchair into the kitchen but did not seem to know what to do once he got there.

By Friday, March 25, John’s face had lost its color, and his eyes had dulled. One of the nurses tended to his feet and lower legs, which had swollen with fluid. Ben began to sense his father’s life would soon be over.
The process was difficult to watch. Some couldn’t. Matt, married to Tim’s daughter, found it too upsetting to interact with John when he visited. But Ben stayed the course. “I was trying to keep in the role of making sure it happened,” Ben says. “I was the protector of the process.”
At one point during the week, someone informed Ben that a caregiver was swabbing his father’s mouth with a sponge soaked in juice — despite being given clear instructions that they were not to give him any food or liquid. Ben had to go into his father’s bedroom and stop her. “It’s really hard for some people to hear that someone isn’t going to eat or drink anything until they die,” he says.
So hard that others want to intervene. But the law is clear. “A physician who treats a patient against their will — even to save their lives — would be guilty of battery,” Gatter says.
Ben worries the Supreme Court’s recent ruling overturning the right to abortion could cloud the right to refuse treatment. “How can you tell a person you cannot make your own decision?” he says. “It’s their legal right. Who’s going to take that away?”
By Saturday, March 26, eight days into his fast, it was clear John had neared the end. He lay on his side in the fetal position, clutching the rails of his hospital bed and moaning. Ben had been sleeping at his brother Tim’s house, a 15-minute drive away, but he decided to spend that night at his father’s townhouse.
A little after 1 a.m. on the 27th, the nighttime caregiver woke Ben and told him death was at hand. Ben found his father still in the fetal position, breathing very slowly. He laid his hand on his father’s shoulder and leaned over him so that his lips nearly brushed his father’s ear. “It’s okay,” he said. “Let your body go. We love you.” And within a few minutes, John Griffith was gone.
Complete Article ↪HERE↩!
