“I cannot escape death, but at least I can escape the fear of it.”
– Epictetus
I wish more people knew that quote during the pandemic. I write this on November 1st, celebrated as Dia de Muertos or “Day of the Dead.” Epictetus and the other Stoics knew that death is inevitable, that life can change in an instant, and viewed it as a reminder to live each day purposefully and virtuously. In a world where meaningless death is a daily fact, only the individual can define meaning in their own lives.
This introduction is not meant to be morose but rather meant to explore the dilemmas in health care at the end of life. One of my colleagues took a phone call that I overheard. It was from the nursing home where his 88-year-old demented mother was housed, calling to say they were taking her to the emergency room due to a change in mental status. “Stop,” he shouted. “My mother has a do not resuscitate health care directive.” The conversation became an argument between the facility’s risk-averse nurse manager and him. The paramedics arrived, the nursing home protocol directed them to take her to the ER, and that was that. The ER soon called; my colleague’s mother was in septic shock, in renal failure due to a kidney infection, and they were starting her on IV antibiotics, and planning dialysis. The doctors were following their script, one based on best evidence-based care. The son anguished in his reminding them of his mom’s end-of-life directive, particularly because his sister, now in the loop, wanted to do “everything we can” if death was not a certainty.
But it is, as reluctant as we all are to acknowledge. Most frontline doctors won’t argue with a family member who reverses the directive in a moment of grief, panic, or guilt. Given their training, these acute care specialists are not willing participants in a “death panel.” The doctors’ skill set and enthusiasm also influence the approach. Highly skilled physicians – expertly trained and confident in their technical talents – are enthusiastic and passionate about what they do and want to do it. This is why advanced hospitals, like ours, have a palliative care team led by a physician, a trained social worker, with an ethics panel to help families and doctors in the throes of such life-wrenching decisions.
Economics plays a role. The amount of health care dollars spent in the U.S., 4.3 trillion dollars or 19 percet of GDP, includes 1.2 trillion spent in the last months of life. That 1.2 trillion is over four times as much as England spends for all health care annually (on a per-patient basis, England spends less than half as much as the US). In England, many procedures, including dialysis, are restricted by the National Health Service, based on utilitarian principles that consider quality of life versus cost. In the US, a fee-for-service payment system financially rewards physicians for each procedure: Hospitals are paid a per diem fee based on the admission diagnosis. This “per click” payment model influences decisions by both parties, consciously or not. Yet many providers and most families do not consider health care expenses when the moment comes to do “everything we can” in the last stages of life. Switching an in-patient to hospice care can improve a hospital’s “pay for performance” mortality scorecard.
The American College of Physicians previously issued guidelines that emphasize each physician’s duty to provide “parsimonious care”; that is, to “practice effective and efficient health care, and to use health care resources responsibly.” Their president at the time stated: “We also have to realize that [we must think] about how resources are used in an overall sense [or] there won’t be enough health care dollars for our individual patients. So while concentrating on our individual patients and what they need, we also need to think on this bigger level both for their benefit and for the well-being of the community at large.” My italicized emphasis brings to mind F. Scott Fitzgerald’s oft-quoted definition of a first-rate intelligence: The ability to hold two opposed ideas in the mind at the same time and still retain the ability to function.
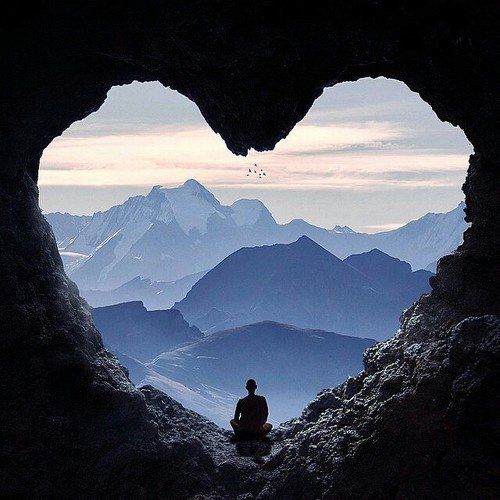
Death is not an entity but a rumination: a tornado of thoughts, fears, visions, and emotions. Only humans see what can and – in the case of death – will be. Not all embrace the introduction, yet it is that sad certainty that introduces order, purpose, and increasing urgency into the human contract. The intensity of a loved one’s passing, or a pandemic, brings it to the forefront of the mind.
Or, as Camus put it in his famous book The Plague: “Plagues are infrequent but constant and they do not alter the conditions of mankind (everybody dies) but rather concentrate our misfortunes into moments where everyone thinks for a change that mortality is afoot.” The Stoics remind us daily that “mortality is afoot” to start each morning with a renewed passion for life.
Complete Article ↪HERE↩!
