— The emotional difficulties of hospice care have made it underutilized and, to some, taboo — medical professionals are trying to change that

Carla Thompson has worked in hospice care for more than two decades, and she knows first-hand just how difficult it can be to make end-of-life decisions.
“You can’t always see the future,” says Thompson, a registered nurse and administrative director for Bon Secours Home Health & Hospice. “When you’re given a diagnosis, you have all these treatment options in front of you. You have to make decisions to keep trying to cure the disease or choose to live with it, focusing on comfort and spending time with family.”
Thompson’s daughter Jessica died last year in hospice services at the age of 31. She fought fiercely for years, but when her breast cancer came back despite aggressive treatment, the family knew it was time to enlist hospice care.
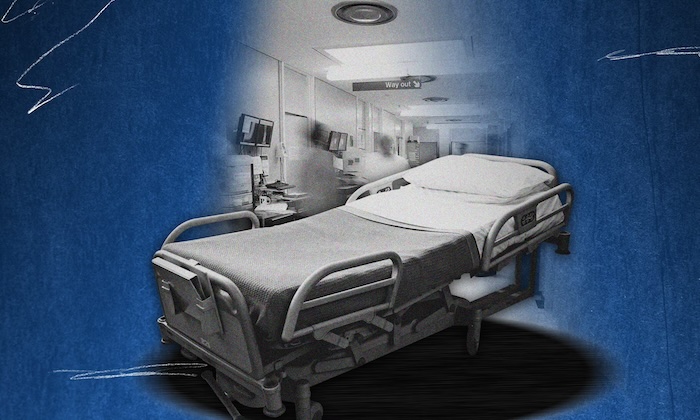
“Jess wasn’t laying in the bed waiting to die,” Thompson says. “She was able to stay home for three months, get the support she needed, and spend time with her four children. She was given medications to help her be comfortable and functional for as long as she possibly could. She was at peace.”
Her hospice team managed her pain and symptoms, brought in a hospital bed and other equipment and provided frequent medical care, services that Thompson says are a blessing for patients as well as their caregivers.
Bon Secours is one of about two dozen hospice providers in Central Virginia. On any given day, hundreds of Richmond-area nurses, chaplains, social workers, home health aides, volunteers and physicians are paying home visits to terminally ill patients, providing them with critical and compassionate support.
Destigmatizing Hospice
While the concept of hospice care dates to medieval times, the first hospice practice in the United States was founded just 50 years ago by a nurse, two doctors and a chaplain who believed patients should pass in their own comfortable environment. Since then, it’s expanded to many providers in all states with two major directions: palliative care and hospice care. In most cases, patients in palliative care are still seeking active treatment, while patients in hospice have a terminal diagnosis and have forgone or exhausted treatment options.
Zach Holt, CEO of Crater Community Hospice in Petersburg, says after 15 years in the business he’s still surprised how many people have misconceptions about hospice. His company is part of a statewide coalition of hospice services working to raise awareness of its benefits. According to a recent report by American Health Rankings, Virginia is 30th in the nation for hospice use, with less than half of Virginians who are eligible for hospice choosing services.
“There’s a big stigma,” Holt says. “People think it’s designed for your last days of life when, in reality, it’s designed for your last six months of life. Studies have shown people across all disease states typically live longer on hospice than they do not on hospice. Our specialized teams are equipped to give patients a higher level of comfort.”
Trish Evans, a registered nurse and director of VCU Health Hospice, admits that hospice is a scary word and fear is a contributing factor for low utilization. “People don’t want to think about death and dying,” she says. “But it’s not about giving up, it’s about your quality of life. It’s a choice on how you want to spend your time with a terminal diagnosis if those are the cards that have been dealt to you.”
Holt encourages Virginians who qualify for hospice to sign up earlier, before they are actively dying, to receive the full benefit. According to the National Hospice and Palliative Care Organization, the median stay for patients in hospice care is 18 days, while Medicare approves stays that are 10 times longer.
Another misconception that leads people to avoid hospice is the possible high cost; in most cases, it’s financially reasonable. According to Debt.org, more than 90 percent of hospice care is covered by Medicare, and patients may be covered through private insurance and charity care.
On the personal end, Evans points out that some believe hospice patients are permanently bedridden at home. “Life can go on,” she says. “There are hair appointments and vacations and family events. We want to give patients the support they need and the comfort they need to continue to do those things before the end stage of their disease.”
Pediatric Hospice Care
When the unimaginable happens and a child is given a life-limiting diagnosis, Noah’s Children provides palliative and hospice services at no cost to families. While run by Bon Secours Richmond, Noah’s Children partners with all health systems in Central Virginia to help families navigate the most harrowing times.
In addition to nurses, physicians, social workers and chaplains, Noah’s Children employs a music therapist, an art therapist and bereavement counselors who visit the patient’s home. They also offer programming for parents and siblings. Nurses are available to attend doctor’s visits, helping parents manage complex treatment plans from multiple sub-specialists.
“We want to debunk the myth that we’re focused on death,” says Dr. Kelly Lastrapes, Noah’s Children medical director. “We’re focused on the best life children can live for as long as they can.”
Planning Ahead
Holt recommends that everyone of all ages have an advanced directive, a legal document that indicates an individual’s health care wishes. “As a society, we don’t like to talk about death, but you have to get uncomfortable and have those conversations,” he says. “I see close-knit families get ripped apart when they haven’t discussed end-of-life care. One sister thinks one way, one sister thinks another, but Mom never told them what she wanted.”
Holt advises families to discuss financials and set realistic expectations. “You hear parents all the time joke about not putting them in a nursing home, so discuss the alternatives,” he says.
As a society, we don’t like to talk about death, but you have to get uncomfortable and have those conversations.
—Zach Holt, CEO of Crater Community Hospice
Some states with high hospice use, like Oregon and Maine, have also passed legislation allowing patients with terminal diseases to self-administer life-ending medication. The Death with Dignity National Center reports that legislation not only eases suffering but brings important conversations about death and dying out of the shadows and into the spotlight. The Virginia Senate passed a “Death with Dignity” bill in February, but members of the House of Delegates chose to table the bill until 2025.
Richmond-area hospice experts recommend that any time a family member has been diagnosed with a terminal illness, they should work with their medical team to prepare a treatment plan as well as an end-of-life plan.
Lastrapes adds that it’s helpful to keep a 10,000-foot view of the patient’s care, understand the trajectory of the prognosis, and set goals early on. While life is filled with unknowns, surrounding yourself with the right people can help ease the pain.
“When you’re born, you have a room full of people to support that baby,” Evans says. “It should be very similar when your life is over. It’s the one thing we’re all going to experience. You should have the ability to surround yourself with your family and your pets and those people who can support you and keep you comfortable.”
Choosing a Hospice Provider
- Start your hospice conversation with your health care team and ask about preferred partners.
- Medicare patients can enter their ZIP code at medicare.gov to find certified providers in the Richmond area.
- Talk to friends, family and neighbors about their experiences with hospice.
- Once you narrow down several hospice providers, interview them about specific services, additional resources, areas of specialty, organizational culture, religious affiliation and other differentiating factors that are important to you or your family.
Complete Article ↪HERE↩!