I’m leaning into death to see if I can change how I feel about it.
By
[I] imagine I’m not the only person who’s written their own obituary, but maybe I’m the first one to see it in print. Writing my obit was the first task in an exercise that came to an end yesterday.
“Brown, Laurie Jane. (October 7, 1957 – March 4, 2018). Laurie died suddenly yesterday in Toronto at age 60.”
I feel like Scrooge seeing his own gravestone.
I am in perfect health, but having recently turned 60 years old, I am feeling an increasing urgency about, well, everything. Why not give myself the deadline to end all deadlines? On Dec. 4, 2017, I decided I had three months to live. Three months to make more of whatever time I have left.
So for the past three months I have been thinking about death everyday. “Is this the last time I hand wash this sweater? Is this the last time I talk with my son?” It was jarring, but I kept going. I wanted to get to a less anxious feeling about my own mortality. By trying to live as if I was dying, would I live each day differently? Might that take some of the sting out of my impending death? Is that even possible?
The first thing anyone with three months to live is told to do is “get your affairs in order.” I updated my will and my living will. Next, I collected all my banking and legal information and printed it. (Kids – it’s in a bankers box on the floor of my closet, along with the full obituary.)
I started my death exercise without telling anyone. Good thing – I could have ruined a few dinner parties. I did let one girlfriend in on it and her response was “March is still too cold to stand by your grave. Can you make it May?”
With two months left on the calendar, I flipped between two very different states of mind. On a good day? I believe I’ve had a full life, a lucky life and I’m good to go right now. But on a bad day, it’s a different story: I want to be a grandmother, I want to create more, I want to grow old. My children need me and my new partner needs me. I couldn’t bear to contemplate the end of a love I had barely begun.
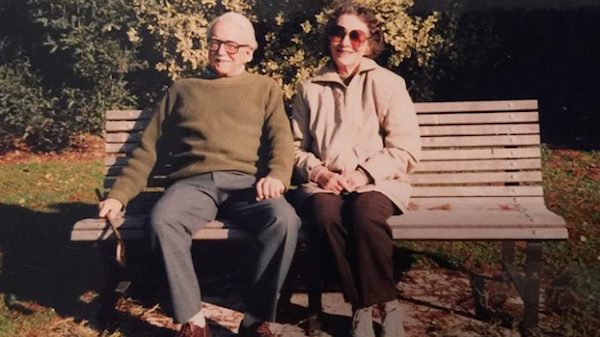
I never used to think about death until my mother died at 58 of ovarian cancer. I was terrified that would happen to me. Now, I scroll through my Facebook feed reading chemo updates and news of departed friends. I feel like death is hunting me and my senses are working overtime to hear the approach. I don’t want to live in fear – so I’m leaning into death to see if I can change that.
Each morning, I opened my eyes and thought of the day in front of me. I paid attention to the morning light through my window, the luxurious feel of my bed sheets, the realization that I had no pain, and I felt great. My feet hit the floor and I jumped into my day joyously. My mantra became ‘say yes until it breaks you.’ I was sounding like an inspirational poster, with kittens. And yet, I didn’t feel as if I was truly living each day like it was my last.
Too embarrassed to talk to people about what I was up to, I turned to books. Die Wise by Stephen Jenkinson struck a huge nerve.
Stephen has been witnessing death for decades, both as head of a palliative-care unit in Toronto and as a “grief whisperer,” helping the dying and their families navigate death. Stephen has no 10-step plan to a wise death but talking about it with him on Pondercast, my podcast, was such a relief.
When my mother lay sick and dying, I felt frozen and mute, and she was keeping what she felt to herself. Probably because I didn’t ask. I have terrible regret about that. I know I’m not alone in these feelings after a parent dies.
We live in a death-phobic culture. We don’t acknowledge dying people, we keep turning the conversation in the other direction, toward life and “keeping up the fight.” We institutionalize our terminally ill and our aged and we outsource the task of dealing with our dead. Illness and death are kept as far from the living as possible – it’s no wonder we are at a loss to find anyone to talk about it with.
In the same way that women have fought to take back the birth experience – bringing it home, surrounding birth with family and siblings, making it a human experience instead of a medical one – might we do the same thing with death?
I began to question my motives in taking on this three-month death exercise. It became clear that I was anxious to learn how to handle death. I wanted to bring order to the chaos of feelings I had. I thought I could learn to embrace death just enough to think I had it pegged.
My experiment is a pale shadow to the real thing. It doesn’t compare to the anxiety and fear felt by those who are truly ill. Nor what I once felt waiting for a biopsy report.
I can’t embrace death, death will embrace me. It will have its way with me. It will be messy and confusing. Death will ask everything of me. Will I be able to accept that? Is it too much to ask that that I might I leave my life loving it?
Perhaps the strangest outcome of this morbid exercise is realizing I have a moral obligation in my final days. Dying will be my last and perhaps most important act of parenting. I need to show my children how it’s done. That death carries with it a responsibility is helpful to me, it gives my death some purpose.
I have started awkward and halting conversations about death with my father, and have asked him to let me in. I want him to share his coming death with me. It will help me when my time comes.
Keeping death in the forefront of my mind is informing everything I’m doing. It’s a funny liminal place to be – but the balance of it feels right.
Laurie Brown lives in Toronto.
Complete Article ↪HERE↩!