By BETH SLEPIAN
A recent analysis published by the New England Journal of Medicine revealed that for the first time since the early 20th century, more Americans are dying at home than in the hospital.
According to the report, in 2017, 30.7% of Americans died at home, while slightly fewer (29.8%) died in hospitals. Another notable statistic from the study is that between 2003 and 2017 the number of Americans who died in hospice-specific facilities grew by 41%, from 0.2% of deaths in 2003 to 8.3% in 2017. According to the National Hospice and Palliative Care Organization (NHPCO), 47.5% of New Hampshire residents on Medicare who died in 2017 were receiving hospice care benefits.
This data does not come as a surprise to those of us who work in hospice care and have the honor of helping families navigate the end-of-life experience.
Up until the mid-1900s, it was routine for people to die in their homes, cared for and surrounded by loved ones, but by the 1950s, more Americans died in hospitals. The concept of “death with dignity” was introduced in the United States in the early 1960s, sparking the movement toward hospice care.
The hospice movement gathered steam in the late 1970s with the formation of the National Hospice Organization, and by the mid-1980s, the federal government formalized the hospice benefit for people on Medicare.
Concord Regional VNA has been caring for people in their homes for 120 years, providing nursing, therapy, personal care, homemaking and other services to people of all ages. For more than 30 of those years, we have provided specialized end-of-life care, guidance, and support to patients and families. In 1994 we expanded our hospice service by opening the first Hospice House in New Hampshire on Pleasant Street in Concord. We have served thousands of hospice patients and their families over the years, including nearly 1,000 patients in 2019.
While it is true that hospice care comes into play toward the end of a person’s life, there are many common misconceptions, such as:
■ Hospice care is only for the last few days or weeks of a person’s life;
■ It is only for people with cancer, people in severe pain or those who have a “do not resuscitate” order;
■ People on hospice do not receive treatment, they’re just kept comfortable with medication;
■ Hospice is a “place” where a person goes to die;
■ Hospice hastens death;
■ People on hospice must give up seeing their primary care providers;
■ Hospice care is focused on the patient and ends when the patient dies.
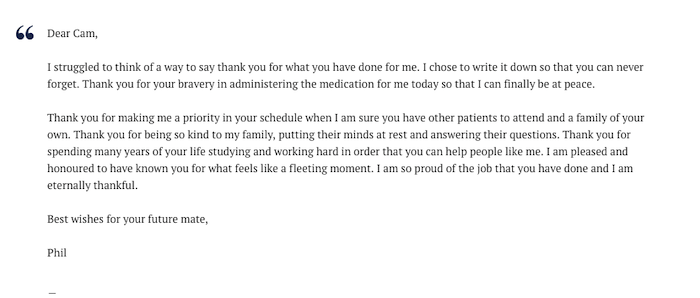
Hospice care is much more than meeting patients’ medical needs. Hospice care empowers patients to have a voice in their end-of-life experience, and to help them through it with as much comfort, grace and dignity as possible. It is about compassion – for them and their loved ones.
Some people choose to begin receiving hospice care in the final weeks or days of a terminal illness, but it is not unusual for patients to begin hospice care many months before they eventually pass.
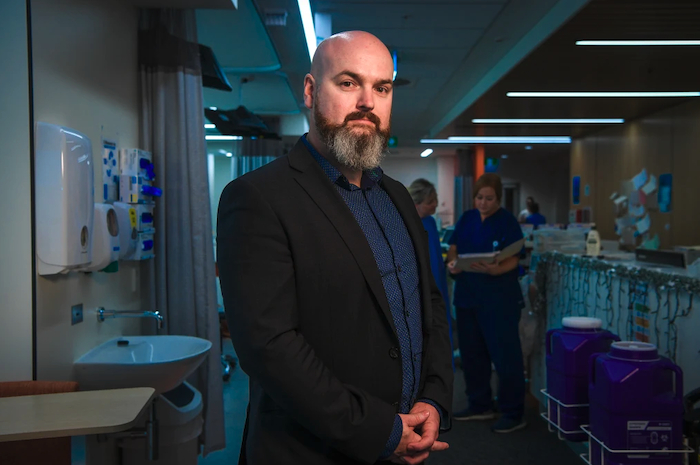
People who receive hospice care through Concord Regional VNA benefit from individualized care coordinated with their care team, which may include their primary care provider and other clinicians. They may receive nursing care, physical and/or occupational therapy, pain management, spiritual care, social work , including emotional support and companionship – all in the place they call home, which could be a private residence, an independent living or assisted-living community, or a skilled nursing facility. Those who need more intensive care may opt to receive care at Hospice House.
Equally as important in this journey are the caregivers, who are most often the patients’ loved ones. Hospice care is about them, too. In addition to day-to-day assistance with patient care, loved ones may receive emotional and spiritual guidance and support from our counselors and spiritual care providers; help with end-of-life planning; much-needed respite care; and myriad other services. And it is important to note that hospice care does not end when a patient dies – our bereavement counselors and support groups help loved ones as they learn to cope with their loss for as long as they need us.
Hospice care is also about volunteers. The hospice movement was started by volunteers and they remain a crucial component to this day. In fact, Medicare requires that volunteers provide at least 5% of total patient care hours, which can take the form of direct support, spending time with patients and families, or performing tasks that support hospice care services. Concord Regional VNA is incredibly fortunate to have nearly 100 volunteers from the communities we serve who give their time and energy to our hospice patients and their loved ones.
So what does this mean and why does it matter? The recently released data suggests that more people have come to understand that receiving care in the comfort of home – in familiar surroundings, in proximity to loved ones and friends – is a preferable and realistic option. From a clinical standpoint, studies show that patients who receive hospice care live longer than those with similar diagnoses who do not receive hospice care. Receiving care at home also has a significant positive impact on overall health care costs.
Death is a fact of life. Patients often tell us that choosing hospice allows them to feel in control, and managing their symptoms helps them feel more at peace. Choosing hospice is not giving up, rather, it is choosing to live fully until you die.
It is not meant to be scary; it is meant to help people live each moment to the fullest and to pass with dignity and respect surrounded by love.
We at Concord Regional VNA are privileged to help patients and their loved ones navigate this journey, and proud to have been providing hospice service to the people of Concord and the 43 other New Hampshire communities we serve for more than 30 years.
Complete Article ↪HERE↩!