‘The Good Death’: Hard to find, and religion’s role may be to blame
There is no such thing as a “good death.” There is only a “good enough death.”
So writes Ann Neumann in “The Good Death: An Exploration of Dying in America.” A visiting scholar at the Center for Religion and Media at New York University and a hospice volunteer, Neumann takes a close-up look at end-of-life issues and how they are both helped and hindered by faith.
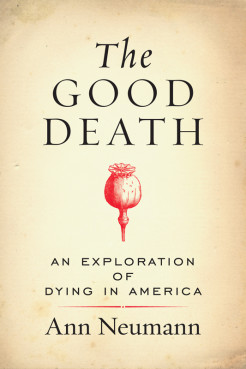
“Religion is most prevalent around the deathbed in our country,” Neumann, 47, said in a phone interview from her home in Brooklyn, N.Y. “That is where it is resoundingly proven that we are not a secular nation.”
“The laws, medical practices and corporate regulations that surround death and dying continue to be strongly influenced by religion, whether it is in the delivery of health care through Catholic hospitals, whether it is in the rituals that medical practice is infused with, or whether it is simply in the language that we find acceptable around the dying.”
If “The Good Death” is anything, it is a call for people to examine their own wishes around end-of-life issues and decide what role religion — either theirs or that of their caregivers — will play. Religion, she holds, influences our ideas of quality of life and how far we are willing to go to preserve it.
Neumann has spent time around the dying. Her first up-close experience as a caregiver was with her father’s difficult, drawn-out death from cancer that left her worn-out and overwrought.
In the aftermath, unmoored by her own grief and seeking a way to cope with the death she knew would someday come for her and her loved ones, she decided in 2007 to become a hospice volunteer. Her descriptions of her visits with her patients are among the most moving in the book.
In between she weaves in the history of death in America, from the front parlor to the back room of the nursing home. She chronicles the harrowing right-to-die cases of Karen Ann Quinlan, Nancy Cruzan, Terri Schiavo and Jahi McMath, who remains in a coma in New Jersey, the only state that does not consider her legally brain dead, Bible verses hanging over her bed.
Newmann, reared a Mennonite and now a Catholic, looks at how quality of life is often sacrificed for sanctity of life, often for religious reasons, by health care providers, families and religious leaders.
“We must examine the inequality and the discrimination that the church has built into its position on health care,” she said. “The Catholic Church is so good at managing hospitals, at addressing patient care that we cannot say it is bad on the whole and yet the discrimination against women, the lack of autonomy provided to elders or to individuals like to Terry Schiavo — these families that are put in these difficult positions should be supported by their church. They should be able to make their own decisions.”

But what about hope? In the book, Neumann echoes the writing of Adrienne Martin, a professor at the University of Pennsylvania, who writes that hope is not always a good thing. It can lead to pain and suffering, both physical and emotional, and result in stretching out an illness in the hope for an unlikely positive outcome.
“It was an area of research that fascinated me because it did question the hands-down understanding we have that hope is always good,” Neumann said. “Hope can be sustaining. It can get us out of bed. But it can also result in the very painful treatment of patients and lead to denial.”
What’s a country with a rapidly aging population to do? The U.S. Census Bureau predicts that by 2050, one in five Americans will be 65 or older and have diverse ideas about end-of-life issues. A Pew Forum survey in 2013 found two-thirds of Americans believe there are some situations in which patients should have a right to end their own lives, while 31 percent say doctors should do everything they can to prolong life.
Start conversations with your loved ones, make your end-of-life wishes clear and know your rights, Neumann said.
“A good death is whatever a patient wants,” Neumann said. “It is not up to me, to their legislators, to their priests, to their families. That is true informed consent. A good enough death is as close as we can get because humans are not perfect. We can get so much closer, but we will never have a perfect death.”
Complete Article HERE!
At my father’s bedside, I learned what death looks like
NHS end-of-life and palliative care must focus more on the dying person’s needs and wishes – but for that we need to have proper conversations
By Jon Henley

My father spent 10 days dying.
He was 84 and he had lost his wife – my mother, whom he adored, and without whom he felt life was a lot less worth living – three years earlier. He died of old age, and it was entirely natural.
The process, though, did not feel that way at all, at least not to me. Dad had been bedridden for months and was in a nursing home. He stopped eating one day, then started slipping in and out of consciousness. Soon he stopped drinking.
For 10 days my sister and I sat by his bedside, holding his hand, moistening his lips. Slowly his breathing changed, became more ragged. During the last few days, the tips of his fingers turned blue. His skin smelled different. His breath gradually became a rasp, then a rattle.
It sounded awful. We were sure he was in pain. The doctor reassured us he wasn’t; this was a human body dying naturally, shutting down, one bit at a time. We had not, of course, talked about any of this with Dad beforehand; we had no plans for this, no idea of what he might have wanted. It would have been a very difficult conversation.
The doctor said he could give him something that would make him at least sound better, but it would really be more for us than for my father. “My job,” the doctor said, “is about prolonging people’s lives. Anything I give to your father now would simply be prolonging his death.”
So we waited. When it finally came, death was quite sudden, and absolutely unmistakable. But those 10 days were hard.
Death is foreign to us now; most of us do not know what it looks, sounds and smells like. We certainly don’t like talking about it. In the early years of the 20th century, says Simon Chapman, director of policy and external affairs at the National Council for Palliative Care, 85% of people still died in their home, with their family.
By the early years of this century, fewer than 20% did. A big majority, 60%, died in hospital; 20% in care homes, like my father; 6% in hospices, like my mother. “Death became medicalised; a whole lot of taboos grew up around it,” Chapman says. “We’re trying now to break them down.”
There has been no shortage of reports on the question. From the government’sEnd of Life Care Strategy of 2008 through Julia Neuberger’s 2013 review of the widely criticised Liverpool Care Pathway to One Chance to Get it Right, published in 2014, and last year’s What’s Important to Me [pdf] – the picture is, gradually, beginning to change.
The reports all, in fact, conclude pretty much the same thing: the need for end-of-life care that is coordinated among all the services, focused on the dying person’s needs and wishes, and delivered by competent, specially trained staff in (where possible) the place chosen by the patient – which for most people is, generally, home.
“It’s not just about the place, though that’s important and things are moving,” says Chapman: the number of people dying in hospital has now dropped below 50%.
“The quality of individual care has to be right, every time, because we only have one chance. It’s about recognising that every patient and situation is different; that communication is crucial; that both the patient and their family have to be involved. It can’t become a box-ticking exercise.”
Dying, death and bereavement need to be seen not as purely medical events, Chapman says: “It’s a truism, obviously, but the one certainty in life is that we’ll die. Everything else about our death, though, is uncertain. So we have to identify what’s important to people, and make sure it happens. Have proper conversations, and make proper plans.”
All this, he recognises, will require “a shift of resources, into the community” – and funding. Key will be the government’s response to What’s Important to Me, published last February by a seven-charity coalition and outlining exactly what was needed to provide full national choice in end-of-life care by 2020. It came with a price tag of £130m; the government is expected to respond before summer.
In the meantime, though, a lot of people – about half the roughly 480,000 who die in Britain each year – still die in hospital. And as an organisation that has long focused on curing patients, the NHS does not always have a framework for caring for the dying, Chapman says.
But in NHS hospitals too, much is changing. There has been a specialist palliative care service – as distinct from end-of-life care, which is in a sense “everyone’s business”, involving GPs, district nurses and other primary care services – at Southampton general hospital and its NHS-run hospice, Countess Mountbatten House, since 1995, says Carol Davis, lead consultant in palliative medicine and clinical end-of-life care lead.
People die in hospital essentially in five wards: emergency, respiratory, cancer, care of elderly people and intensive care, she says: “Our job is about alleviating patients’ suffering, while enabling patients and their families to make the right choices for them – working out what’s really important.”
Palliative care entails not just controlling symptoms, but looking after patients and their families and, often, difficult decisions: how likely is this patient get better? Is another operation appropriate? What would the patient want to happen now (assuming they can’t express themselves)? Has there been any kind of end-of-life planning?
Of course many patients in acute hospital care will not be able to go home to die, and some will not want to, Davis says: “Some simply can’t be cared for at home. If you need two care workers 24/7, it’s going to be hard. Others have been ill for so long, or in and out of hospital so often, they feel hospital is almost their second home. So yes, choice is good – but informed choice. The care has to be feasible.”
In 2014, the report One Chance to Get it Right [pdf] identified five priorities in end-of-life care: recognise, communicate, involve, support, and plan and do. (“Which could pretty much,” says Davis, “serve as a blueprint for all healthcare.”) The first – recognise, or diagnose – is rarely easy. How does a doctor know when a patient is starting to die?
“There are physical signs, of course,” says Davis. “Once the patient can’t move their limbs, or can no longer swallow.” But, she says, “we have patients who look well but are very ill, and others who look sick but are not. In frail elderly people – or frail young people – it can be hard to predict. Likewise, in patients with conditions like congenital heart disease, where something could happen almost at any moment.”
Quite often, Davis and her team face real doubts. “Right now,” she says, “I have a patient in intensive care, really very ill. They probably won’t pull through, but they might. I have another doing well, making excellent progress – but they’ve been in hospital for three months now. They’re very, very weak, and any sudden infection … You just can’t predict.”
Which is why communication, and planning, and involving the family – all those difficult and painful conversations that we naturally shy away from – are so very important.
It could well be, for example, that my father would actually have wanted his death to be prolonged: he certainly clung on to life with a tenacity that startled my sister and me. We will never know, though, because we didn’t talk about any of it.
“It is our responsibility – all of our responsibility – to find the person behind the patient in the bed,” Davis says. “One way or another, we have to have those conversations.”
Complete Article HERE!
Families smuggling lethal drugs into hospitals so loved ones can die: Nitschke
By Julia Medew

Three people smuggled lethal drugs into Australian hospitals last year so their loved ones could secretly take their own lives when nobody was watching, euthanasia campaigner Philip Nitschke claims.
The head of Exit International said all three patients were elderly people with serious illnesses when they took a lethal drug in their hospital beds. They were being cared for at the Royal Prince Alfred and Concord hospitals in Sydney and the Austin hospital in Melbourne.
In each case, a partner or adult child took the lethal drug to them in hospital, Mr Nitschke said. The patients had previously acquired the drug in case they wanted to take their own lives one day.
Mr Nitschke, a former medical practitioner, said the three people took their drug overnight while no hospital staff were watching. The next morning, their deaths were recorded with no suspicion about how they died.
“In each one of those three cases, there have been no questions asked. It’s not surprising because they were very sick. The assumption was that they just died,” he said.
The cases are now being used by Mr Nitschke in his workshops on assisted death. He said while many people fear they will not be able to take their own lives in hospitals or other institutions such as nursing homes, these recent stories show it can be done.
However, he warned that if the relatives were caught smuggling a lethal drug into a hospital, they could be charged with criminal offences including assisting a suicide.

Mr Nitschke recently tore up his medical licence after the Medical Board of Australia demanded he stop discussing suicide if he wanted to keep his medical registration. He has since continued his work with Exit International.
Dr Rodney Syme, of Dying with Dignity Victoria, said he had never heard of families assisting people to die in hospitals in such a fashion. However, he said the reports added to the case for assisted dying laws in Australia. If there were more options for people to end their lives when the time was right for them, he said clandestine suicides in hospitals would not happen.
Margaret Tighe, of Right to Life Australia, said it was appalling that Mr Nitschke was promoting these deaths. She said the hospitals should investigate them and boost their security.
While spokespeople for the hospitals said they did not know anything about the deaths, a spokesman for NSW Health Minister Jillian Skinner said: “Any matter of this nature should be referred to the appropriate agency, the police, and accompanied by details and evidence of the illegal activity.”
A spokesperson for federal Health Minister Sussan Ley said she was “disturbed by any serious breach of accepted or ethical medical standards and this certainly falls into that category”.
“Obviously our department will need to obtain more information from the relevant health offices in both states before we could comment in any detail,” her spokesperson said.
A spokeswoman for Victorian Health Minister Jill Hennessy would not comment on the reported deaths, but said the Victorian government was introducing laws this year to give people more choice about the kind of medical care they want or do not want in the event of future illnesses such as cancer or dementia.
The Australian Medical Association would not comment on the report, but Secretary of the Australian Nursing and Midwifery Federation, Lee Thomas, said: “It is unfortunate that any person needs to resort to drastic measures to relieve their pain.”
“Overwhelmingly ANMF members support the right to die with dignity and many have been engaged in the dying with dignity movement,” her statement said.
Complete Article HERE!
How to Talk to Your Grown Kids About Your Mortality
Do these three things and your children will thank you
By Elizabeth Fishel and Jeffrey Arnett

During a car ride, Peter brought up to his two twentysomethings what his end-of-life wishes would be: No heroic measures, because he wouldn’t want to suffer and wouldn’t want his family to endure it. One of the boys took this in stride, but the other became very upset, asking: “Why are you talking about this? It’s horrible that you’re so calm about death.”
Death comes to us all, but in the 21st century, it comes later than ever for most people. Because of medical advances, life expectancy has stretched to record highs, and in the United States and other countries most people can expect to live into their 70s or 80s. Perhaps for this reason, we generally prefer to ignore death and avoid talking about it, even when we’re in our 60s or older. And our young-adult children, certain of their own immortality, may also prefer to think of their parents as living forever. Bringing up our mortality may provide a rude awakening to grown children of any age.
But we ignore it at our peril, or rather, at the peril of those we love. They may not want to hear us talk about the inevitable visit from the Grim Reaper, but if we neglect the responsibility to prepare for our death — and to prepare them for it — we do them a disservice and leave them with a stressful mess when the time comes. That’s a legacy few of us would wish.
So, here are three crucial issues to make sure you address and discuss:
1. Make a Will
You need to have a will, and once you do you need to make sure your loved ones know about it. Because we tend to prefer to think of death as many years away no matter what age we are, many of us fail to fulfill the basic responsibility of making a will. Various surveys indicate that about 50 percent of American adults have not had one drafted. The percent who have made a will rises with age, but even among 55- to 64-year-olds, 40 percent have no will.
Here’s the problem with that: If you die without a will, the state takes over your estate and makes the decisions about who gets what. Who would want that?
So, no excuses: If you haven’t prepared a will yet, do it as soon as you’re done reading this post! There are many inexpensive online options or you can hire anestate planning attorney if your estate is complex or you’d like the assurance that all the legal steps have been taken correctly.
2. Make Funeral Plans
Figure out plans for your funeral and burial or cremation and make sure family members know what ,and where, the plans are. We’re not crazy about talking about this aspect of death, either, but again, wouldn’t you rather decide on this now, rather than leaving it to your grieving family members to handle hastily after your death? You may find consolation, too, in the thought that the post-death commemoration will be done as you would have wished, even though it is a party you will not be able to attend.
3. Make Your End-of-Life Plan
You also should come up with your end-of-life plan and make sure your loved ones know about it. Medical interventions are extremely effective at keeping us alive at the end of life, even after any prospect of restoring us to consciousness, much less good health, has passed. People vary in how they view this issue, from those who want all possible steps to be taken to those who would prefer not to prolong the inevitable.
Ask your doctor how to make an “advance directive” that will contain your instructions or look up the instructions online from a reputable source like AARP or state government websites (each state has its own laws concerning end-of-life care).
Don’t assume your loved ones will know what to do; they probably won’t, and you don’t want them to have to make those decisions amid the stress and sadness of losing you.
Difficult as these conversations and plans may be, for your children’s sake and for your own peace of mind, discuss them now, while you are lucid and healthy. Your children may not thank you today, but they will appreciate the guidance when the time comes. That’s one last gift of love you can give them after you’re gone.
Complete Article HERE!
New website will give people ‘greater control over their death’
By JAMIE BULLEN

A website which allows people to declare how they wish to be treated in the final weeks of their lives is set to launch this week.
Compassion in Dying, a charity that supports people to exercise their rights over end-of-life treatment, said MyDecisions.org.uk will give people greater control over their death.
The group said the website was created in response to fears not enough people were planning for how they want to be treated in the advanced stages of their life.
A statement on the MyDecisions.org.uk homepage reads: “You might not like to think about it but there might come a time when you’re too unwell to tell those caring for you – like your family or a doctor – what you do and don’t want to happen.”
Anyone visiting the site can fill out an “advance decision” where users can refuse any drugs or medical treatments that may be given to them at some time in the future.
The document, also known as a living will, is legally binding meaning any healthcare professional that ignores it risks going to court.
The website also allows people to make an “advance statement” to declare preferences, wishes and beliefs for those who might have to make choices for them should they lose the capacity to make their own decisions.
According to research commissioned by the charity, only 4 per cent of Britons made a record of their preferences last year.
The website is set to go live on Thursday.
Complete Article HERE!
10 Excuses You Tell Yourself Why You Don’t Need To Have The Conversation & 10 Reasons Why Those Excuses Don’t Hold Up
We did a survey in 2013 which found that “90 percent of people say that talking with their loved ones about end-of-life care is important yet only 30 percent of people actually have done so.” Clearly, knowing the importance of a conversation or behavior doesn’t always mean we’ll do it. How many diets and half-marathon training programs have begun in this vein? We know all the excuses a person is likely to tell themselves to avoid the conversation. Any of these look familiar?
“I know my loved one well enough to make the right call.”
There are plenty of reasons to have the conversation with your loved one beyond your belief that you know what they would want. Having a specific conversation about they would prefer could bolster your confidence, strengthen their trust and reward you with a new sense of intimacy. The conversation could really surprise you. You might discover something about your loved one that you never expected.
“I don’t need to have the conversation. I’m healthy and young.”
The Conversation Project is an initiative to encourage people to have these conversations before they are sick or terminal. If you’re healthy and well, it’s the perfect time to have the conversation. As we say, it’s always too soon, until it’s too late.
“If my loved one wants to have a conversation, they can come to me.”
This excuse is extremely powerful. It allows you to believe you’re up for the conversation while simultaneously avoiding it.. Don’t fall victim to this one. Your loved one might be thinking the same thing, trapping you both in a game of chicken, in which neither of you have important conversations about your health, your finances and your future because you’re waiting for the other to initiate it.
“I’ll just decide based off what I would want.”
This excuse provides false comfort. No need to have the conversation because you know what you would do for yourself. Right? But this method of avoidance leads to an improbable and unrealistic scenario. Even if you are the designated health care proxy that doesn’t mean you’ll be the only one who cares about the outcome. You might find yourself having to explain your choices to other family members, friends and caretakers. This might open up a disagreement between family and loved ones who believe the person in question wouldn’t want that. And you’d be surprised how many decisions you might have to make. Imagine what happens when you need to make a decision and you don’t know what you would want.
“It makes me uncomfortable.”
The thought of having The Conversation can make a lot of people uncomfortable. Understandably. You do have the right to live your life with minimal discomfort, but consider this: we’ve heard from a lot of people who wished they’d had the conversation, rarely those who wished they hadn’t. Knowing what a loved one prefers can give you A LOT of comfort during a time when you most desperately need it.
“I don’t want to encourage my death by talking about it.”
We work with many diverse communities of various beliefs, cultures, and faiths. Each has their own history, experience and theological lens through which they view death. Our mission is to ensure that your fears aren’t holding you back from a very real and human experience.
“I don’t want to offend my loved one.”
Death doesn’t have to be an offensive topic, and if your loved one perceives it to be so, maybe you can start the conversation there. Ask them why they find death so offensive. A simple question can lead into a complex and profound conversation.
“I don’t need that kind of negativity in my life right now.”
Having the conversation doesn’t have to lead to a negative experience. Many people who had the conversation describe it as a positive, freeing experience rather than a negative one.
“I don’t even know what my career path will be let alone what I prefer about my end-of-life care.”
If you’re in your twenties or thirties, it can be particularly difficult to focus on your end-of-life care. You’re focusing on surviving the hardship of life post-college. We know the #TheStruggleIsReal. But while it’s hard to relinquish the coziness of childhood irresponsibility, you must. Get your affairs together: start that 401K, use sunscreen, stop eating take-out every night, and have the conversation with your loved ones.
“Why do we need to have a conversation? Can’t my loved one just write everything down?”
Modern medicine is helping individuals live longer than ever before, and with that extended time on earth comes increased medical complications and a lot more decisions to be made at the end-of-life. People will often say, ‘if I am ever like that – pull the plug,’ but there is often no proverbial plug to pull. Instead, there is a number of cascading decisions left for your loved ones to make. Talking through your values with your family can give them the guidance to navigate the health care options presented to them. Questions like: “What matters most to them at the end of life?” “Do they want to be at home or in the hospital?” “Do they mind visitors?” “Who do they want to make sure is there?” “Is there a book they might want read to them?” “Do they want music playing or a ball game on in the room?” These are the questions you might find yourself considering. Conversations are organic; they are interactive. This conversation isn’t just about answering a set of medical questions, but exploring all the avenues you didn’t think were possible.
So really, what are you waiting for? Check out our Conversation Starter Kit and have the conversation today.
Complete Article HERE!