I have this great opportunity to cross post, here, a posting I made this morning on my sex advice site, Dr Dick’s Sex Advice.
Name: LD
Gender: Male
Age: 38
Location: Atlanta
How do you jump back into the game when your partner passed away suddenly? Getting really horny but its still awkward to actually do it.
Good question, LD. You say you’re feeling awkward. Why exactly? Is it because you’re out of practice with the whole dating thing? Are you concerned that people might think you’re jumping the gun, trying to get back into the game before your partner is cold in the grave? People can be pretty heartless about this. Or, is your awkwardness associated with your grief?
Grief has a profound effect on every aspect of our lives. Yet there is hardly any literature on the effects grief has on our sexuality. To my mind, grief is the leading causes of sexual dysfunction for those who have experienced the death of a partner.
Allow me a bit of time here for one of my pet spiels. Healing and helping professionals often misdiagnose grief. I want to make one thing clear, grief is not depression. Treating grief with an antidepressant is counterproductive. It can actually take away the impetus to resolve the grief and get on the rest of one’s life.
Making sure that you have processed your grief may eliminate some of your awkwardness you are currently experiencing. This is something I’m pretty familiar with. A good portion of my private practice is with sick, elder and dying people and their friends and family who survive them. I know the impact a terminal illness and dying process can have on the surviving spouse or partner. We often go into survival mode, shutting down so much of ourselves in an effort to have the strength to cope with this life-altering experience. Of course, trying to kick-start our life afterwards is often a monumental effort. Without the support and guidance of a professional or a group of similarly challenged people, some of us just sink to the lowest common denominator.
I believe in the resilience of the human spirit. I believe that we can honor our dead and continue to live and love. It sounds to me like you have a desire to get on with your life, LD, to fill the void, to make new connections, but you simply don’t know how. Acknowledging that fact is a real good place to begin.
 Perhaps you could start by reawakening your sexuality through self-pleasuring. Reconnect with your body and the joy it can bring you. Reestablishing a social life will no doubt follow, slowly at first. But the inevitable tug of the need for human-to-human contact will draw you, if you let it. Remember the best testament to those who have died is to continue to celebrate life itself.
Perhaps you could start by reawakening your sexuality through self-pleasuring. Reconnect with your body and the joy it can bring you. Reestablishing a social life will no doubt follow, slowly at first. But the inevitable tug of the need for human-to-human contact will draw you, if you let it. Remember the best testament to those who have died is to continue to celebrate life itself.
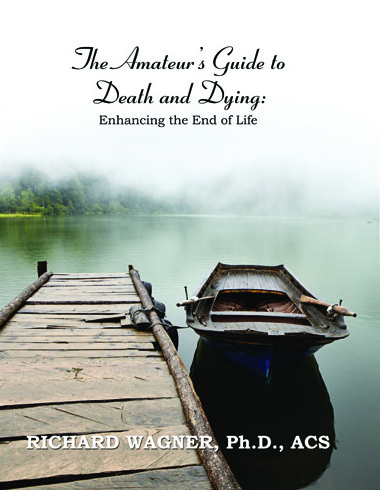
Allow me to draw your attention to my latest book, The Amateur’s Guide To Death And Dying; Enhancing The End Of Life. Actually it’s more of a workbook then a text and while its primarily target are those currently facing their mortality it’s not exclusively for them. Concerned family and friends, healing and helping professionals, lawyers, clergy, teachers, students, and those grieving a death will all benefit from participating in the interactive environment the book provides.
Of special interest to you will be Chapter 6, Don’t Stop. My good friend and colleague, Dr Cheryl Cohen Greene, joins me in presenting this chapter on sex and intimacy concerns. Like I said above, there is a dearth of information about this timely topic for sick, elder and dying people as well as those who are grieving. So I am delighted that my book helps break this deafening silence.
I hope you take the time to write back, LD. I’d very much like to keep tabs on how you are doing.
Good luck