By Erica Curless

Bob Faller died after a day of fighting and struggling. Naked and fierce, gripped by death’s delirium, he rolled on the floor tearing paper into tiny shreds. He tried to flush his pants down the toilet.
Jane, his wife of 58 years, was alone in their rural Republic house, terrified. Helpless.
When a new day dawned, she called a hospice nurse, who told Jane to increase her husband’s morphine dose to every two hours. Bob eventually settled, slept, and slowly let his body shut down.
Longtime friend Steve Anthes was with Jane as Bob, 79, took his final breath. It was Oct. 19, nearly 18 months after Bob was diagnosed with throat cancer, 18 months of dying slowly in the forests far away from hospitals, tubes and machines. It was the ending he chose.
Now a new struggle begins for Jane. Can this 77-year-old woman live alone in the winter in remote Ferry County with little money and medical bills arriving daily?
Relief brings feelings of guilt
“It’s quiet now,” Jane said shortly after her husband’s death. Her voice was strong but soft over the phone, the relief evident.
Yet within an hour, her house filled with people and the chaos of dying’s aftermath. The coroner, friends bearing containers of food, phone calls, decisions.
By 9 p.m., Jane sat in near-darkness on her couch, alone. Murphy the dog slept on the floor near her feet. Bob’s hospital bed was around the corner, empty.
“I feel guilty at feeling so relieved,” she said. “I’m really going to sleep tonight.”
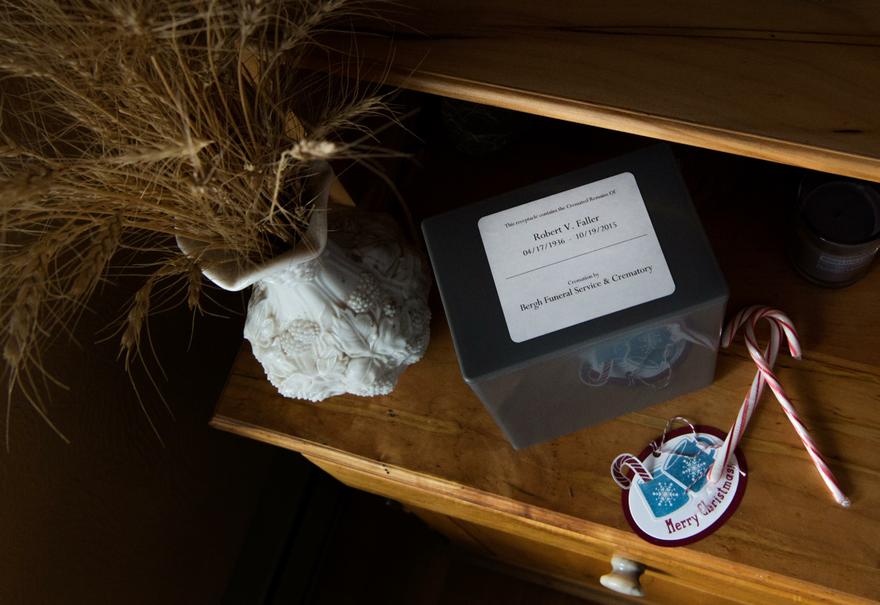
Three months later, Bob’s ashes are in a gray plastic box on a beautiful wooden shelf that he crafted with his own hands years ago. Jane carefully removed the lid, exposing a plastic bag of ash. She put her nose near the bag and took a big sniff. She shrugged. At first she talked to him a lot, lit candles. Not so much now.
Jane’s unsure what she will do with the ashes, other than eventually spread them somewhere in nature. It doesn’t matter right now as snow falls outside the window and each day presents more pressing problems and challenges.
Two weeks ago the weather warmed and snow slid from the roof, burying the deck so she couldn’t open the door. She called for help.
A few weeks before that, the ancient hot water heater leaked at least 25 gallons onto the floor and into the crawl space under the house. She called the local hardware store for the name of a plumber, who inspected the damage and asked for a $400 check to buy a new heater and supplies. The man was gone several hours, long into the evening; Jane panicked. At one point she held her cramping stomach, wrought with stress. But he eventually returned and by 9:30 p.m. had the tank installed and working. She paid another $125 in labor costs and then had to buy a new faucet for the sink. Her hand shook as she wrote the check.
After visiting her daughter in Issaquah, Washington, for Thanksgiving, she returned home and turned on the kitchen light. It crashed from the ceiling.

Cumulative stress taking its toll
Jane knew living alone would be challenging, but she wasn’t prepared for the reality of it.
A year of stresses have snowballed: Bob’s illness and mental highs and lows. The nasty fall while walking her dog that turned into a three-hour ambulance ride and a weeklong stay in a Spokane hospital. The missed time with her dying husband because of her hospitalization. The nearby forests that erupted in wildfires this summer, the same week Bob started hospice care, forcing them to prepare to evacuate.
Now there’s snow and ice and long, dreary days. After spending months with her arm immobilized in a brace and then in physical therapy, Jane’s arm and hand still hurt. The scars are purple and angry. Her fingers ache.
Jane is timid about walking, although she used to hike miles a day in all weather. She hasn’t resumed her yoga practice. Her legs and feet are achy.
“She’s keeping a good face on it,” said Cherie Gorton of Rural Resources, who checks on Jane at least weekly and recently sat with Jane as she opened piles of medical bills. “I think it’s to the point where she probably needs to get out more. Accept invitations. But I know that is really hard to do.”
Gorton called Jane’s daughter in Issaquah, Cat Kelley, to see if she could help her mother make sense of the mounting medical bills from the hospital stay and ambulance ride. Jane has Medicare, but that only covers a percentage of the bills. She has a few too many dollars in her savings account to qualify for Medicaid. Jane and Bob took out a reverse mortgage that covers their mortgage payment, and she receives Social Security. Her son in North Carolina recently created a GoFundMe account to ask people for donations.
The financial woes weigh heavy on Jane. She doesn’t like owing people. Her kids want her to wait for all the bills to arrive so she knows how much she owes. Then they will figure out a plan.
“It makes me really upset,” Jane said, after a recent trip to the mailbox, which most always contains a bill. “It’s horrible.”

Once estranged, the kids have visited their mom
Jane and Bob chose an adventurous, nomadic life at the cost of not having more than a few thousand dollars in savings. They never thought about getting old, getting sick or having medical expenses.
Yet Jane doesn’t regret their independent lifestyle and her husband’s dreamy, back-to-the-land mentality.
Kelley, Jane’s daughter, said her mom recently told her that’s she’s trying to remember only the good things about her life with Bob.
“That will be stuck in my mind forever,” Kelley said. “I like it.”
The Fallers’ romance with nature, however, hasn’t been embraced by their four living children.
“That’s how she wants to live,” Kelley said recently. “She has something in her that thrives on that.”
All the children have rebelled against their parents’ hippie lifestyle. In subtle ways, they have all alluded to the fact that having Bob as their father wasn’t easy. He was gruff, demanding.
Today all the Faller children are financially conservative, have stable, traditional jobs and live in large houses in the suburbs. They drive nice cars and buy material things.
Kelley, an attorney who no longer practices, proudly has three bathrooms in a big house. It has a generator so she is never without electricity. She said she will never again live like a squatter, as she believes the family did when they homesteaded in Canada and lived in a shack without running water or a toilet and where her mom cooked over an open fire.
The result was something of an estrangement between the children and Bob, and by association, Jane.
Since Bob’s death, three of the children have reconnected, however, jointly visiting their mom in November to help her prepare for winter and sort through Bob’s possessions. Kelley said it’s relieved a lot of family tension.
Before Bob died, one of his grandsons, Bobby, came for a rare visit, to say goodbye and make peace. Afterward, Bob would talk about the visit until his voice gave out. He reiterated the importance of family, even when people don’t agree and view the world differently. Afterward, Bob felt energized, somehow released from his burdens. Perhaps it was that connection he needed, proof that the Faller tenacity lives on.
With that same tenacity, Jane is reaching deep into her adventurous soul and said she intends to stay put on her beloved land. She looks through seed catalogs by the wood stove. Friends are plenty, checking on her, plowing the driveway, helping in any way she needs. This is home.
“I’m staying as long as I can,” she said with her girlish giggle. “We’ll see what happens.”

Complete Article HERE!











