Given hypothetical, anything-goes permission to choose from a creepy, unlimited vending machine of endings, what would you select? Should you have the right to choose?

BY ROBYN K. COGGINS
After a particularly gruesome news story — ISIS beheadings, a multicar pileup, a family burnt in their beds during a house fire — I usually get to wondering whether that particular tragic end would be the worst way to go. The surprise, the pain, the fear of impending darkness.
But lately, I’ve been thinking that it’s the opposite question that begs to be asked: what’s the best way to die? Given hypothetical, anything-goes permission to choose from a creepy, unlimited vending machine of endings, what would you select?
If it helps, put yourself in that mindset that comes after a few glasses of wine with friends — your pal asks something dreamy, like where in the whole world you’d love to travel, or, if you could sleep with any celebrity, who would it be? Except this answer is even more personal.
There are lots of ways to look at the query. Would I want to know when I’m going to die, or be taken by surprise? (I mean, as surprising as such an inevitable event can be.) Would I want to be cognizant, so I can really experience dying as a process? Or might it be better to drowse my way through it?
Many surveys suggest that about three-quarters of Americans want to die at home, though the reality is that most Americans, upwards of 68 percent, will die in a hospital or other medicalized environment. Many also say they want to die in bed, but consider what that actually means: just lying there while your heart ticks away, your lungs heave to a stop. Lying around for too long also gets rather uncomfortable — as anyone who’s spent a lazy weekend in bed can tell you — and this raises a further question: should we expect comfort as we exit this life?
Sometimes I think getting sniped while walking down the street is the best way to go. Short, sweet, surprising; no worries, no time for pain. Sure, it’d be traumatic as hell for the people nearby, but who knows — your death might spark a social movement, a yearlong news story that launches media, legal, and criminal justice careers. What a death! It might mean something. Does that matter to you — that your death helps or otherwise changes other people’s lives? If there’s not a point to your death, you might wonder, was there a point to your life?
These are heavy questions — ahem, vital, ones — that don’t seem to come up very often.
I got curious about how other people would answer this question, so I started asking colleagues and friends for their ideal death scenarios (yes, I’m a blast at parties). I heard a wide variety of answers. Skydiving while high on heroin for the second time (because you want to have fun the first time, according to a colleague). Drowning, because he’d heard it was fairly peaceful once the panic clears. Storming a castle and felling enemies with a sword to save a woman, who he then has appreciative sex with, just as he’s taking his dying breaths. (That poor gal!) An ex-boyfriend of mine used to say that the first time he lost bowel control, he’d drive to the Grand Canyon and jump off.
My own non-serious answer is to be tickled to death, sheerly for the punniness of it.
Anecdotally, young men were more fancy-free about their answers, while the older folks and women I spoke with gave more measured answers or sat quietly. Wait, what did you ask? I’d repeat the question. A pause. Hmm.
One old standby came up quite a lot: dying of old age in my bed, surrounded by family. The hospital nurses I asked had a twist on that trope: in bed, surrounded by family, and dying of kidney failure. Among nurses, there was consensus that this is the best way to go if you’re near death and in intensive care — you just fade out and pass, one ICU nurse told me. In the medical community, there’s debate about how calm death by kidney failure actually is, but really, who can you ask?
These answers are all interesting, but my nurse friend got me wondering about people who deal with death on the regular — what do they think about the best death? Do they think about it? Surely hospice workers, physicians, oncologists, “right-to-die” advocates, cancer-cell biologists, bioethicists, and the like have a special view on dying. What might their more-informed criteria be for my “best death” query?
I started with a concept that I think most can agree with — an ideal death should be painless.
***
Turns out, a painless death is a pretty American way to think about dying.
Jim Cleary, a physician in Madison, Wisconsin, specializes in palliative care, cancer-related pain relief, and discussing difficult diagnoses with patients. “Eighty percent of the world’s population lacks access to opioids,” he tells me. That includes morphine, fentanyl, oxycodone, and many of the other drugs used to soothe patients in the United States. Cleary is director of the World Health Organization’s pain and policy studies group, which is working to get these relief drugs to other nations to help those in need — burn and trauma victims, cancer patients, and women giving birth.
In his work with American cancer patients, he’s careful not to suggest that dying will be comfortable. “I can’t promise ‘pain-free,’” he says. What he can promise is that he’ll try his best to help patients end their lives as they wish. “Listen to your patients,” he tells his colleagues, “they have the answers.”
Cleary says you can lump the different ways we die into categories. The first is the sudden death. “That’s not going to be a reality for most of us,” he’s quick to point out. The other category is the long death, which is what most of us will likely experience. “The reality is death from cancer,” says Cleary, “where you actually know it’s going to happen, and you can say goodbye.”
According to the American Cancer Society, a man’s risk of dying from cancer is 1 in 4, and a woman’s 1 in 5. (It’s important to note that those numbers are just for dying from one of the many types of cancer, from bladder to brain, prostate to ovaries. The odds that a man will develop cancer are 1 in 2; for women, 1 in 3. Reality, indeed.) In long-death cases, most care does not extend life so much as extend the dying process, a fact noted by many end-of-life experts, from surgeon and author Atul Gawande to hospice patients.
Cleary thinks the idea of a “best” death or even a “good” death is a little misleading, as if it’s a competition or something one can fail at. He prefers the term “healthy dying,” which isn’t as oxymoronic as it sounds. To him, healthy dying means that death is “well-prepared for, it’s expected, and other people know about it.”
“We as a society have to do much, much more on accepting death as a normal part of living,” he says. “So rather than even talking about what’s ‘the best way to die,’ how do we normalize dying?” In a country where funeral parlors handle our dead and corpses no longer rest for days in our own parlors at home, we’re rather removed from the whole ordeal.
Still, I press Dr. Cleary to answer the question at hand: How would he choose to die? “Would it be sudden death walking along a beach in Florida?” he ventures, then quickly reconsiders. “But if your family doesn’t know you’re dead — dad goes for a walk or run and doesn’t come back — is that good for them? It may be good for me, but it may not be good for them.”
***
In many American hospitals, you’ll find representatives from No One Dies Alone (NODA), a nonprofit volunteer organization formed in 2002 by a nurse named Sandra Clark. NODA’s founding principle is that no one is born alone, and no one should die alone, either.
NODA volunteers work in groups of nine. Each carries a pager 24 hours a day during their assigned shifts, so that one of them is always available to attend a death. Usually, a nurse makes the phone call summoning NODA volunteers. The vast majority of people who NODA visits are comatose. But that makes no difference, the principle abides; comatose or not, it’s still important for someone — anyone — to be present.
Anne Gordon, NODA’s current program director, has helped hospitals around the country start the program in their facilities. She has a worldly perspective similar to Cleary’s, and different from the expectations that most Americans have on the topic of death.
“Dying is a process, not [just] the last breath,” says Gordon. If you’re a hospital patient in the process of dying, there’s a specific protocol to qualify for NODA services. You need to be actively dying — estimated to pass in the next day or so. (“Seasoned nurses can tell,” Gordon says, which is why they’re often the ones to page the NODA volunteers.) You must have reached a point where you will not receive any further interventions — that means comfort care only, with a required “do not resuscitate” order. And you must be without family or friends who can keep you company as you pass away.
Nobody? How does it happen that a person has nobody to visit when they die?
“Sometimes a person’s outlived everyone, or they’re estranged,” Gordon explains. Maybe they do have family, but for whatever reason, the loved ones needed to leave, or live far away, or just cannot bear to be present. Some of the patients are homeless and, just as in their healthier days, have no one to comfort them. Whatever the reason, NODA will be there.
As Gordon sees it, death is an act of meaning, and the process — what she calls “the human family coming together” — is an act of intentionality and love. “I find the whole process to be so compelling,” she says. “It’s our shared experience — a key transition we all share.”
Gordon, a Baby Boomer, sees her work and the recent public interest in end-of-life issues as a byproduct of her generation aging — an extension of the consciousness-raising of the 1960s and “one of the good echoes” from that era, she quips. “As we get closer to death, we like to talk about these things.”
There are “death cafes,” informal coffee hours where friends and strangers get together, eat cake, and talk about dying. There are high-demand conferences where people share their personal experiences of loss and grief. There are bestselling books about coming to terms with your own mortality and how to prepare for death — spiritually, familially, and financially. Even Costco, the bulk-retail giant, sells coffins alongside its low-price tire changes and discount cruises. It’s mostly just static noise, though. Death is never fully discussed, only hinted at from the margins.
Gordon believes that now — with Baby Boomers entering retirement, many losing their parents, and many more coming to grips with their own mortality — is the moment to talk through these issues as a culture, to discuss the process of death in specific terms, beyond the anecdotal and platitudinal. “When death is a daily concept,” as it might be in Bhutan, she offers, “it’s not as terrifying. What matters is quality of life.”
When I ask Gordon how she’d like to die, she demurs. “I have no answer. I figure it’ll be what’s appropriate for me.”
***
Pamela Edgar is an end-of-life doula and drama therapist in Brooklyn, New York. Similar to how birth doulas help pregnant women bring new life to the world, end-of-life doulas help people on their way out.
Edgar grew up with a mom who worked in nursing homes, and young Pamela sometimes tagged along, visiting people at different stages in their lives, including the final ones. As she grew older, Edgar got especially interested in those last months: “What is the kind of relationship that you can have with someone when it might be one of their last new relationships? What can that be like?” she wondered.
Edgar has worked in nursing home dementia units and other late-life facilities for the past eight years. After working in a Veterans Administration hospital during an internship as a creative arts therapist, she requested to go to the hospice unit. (“Nobody ever asks to do that!” she remembers her supervisor replying.) For the past three years, she’s been an end-of-life counselor with Compassion & Choices. The organization is primarily known for advocating right-to-die legislation at the state level, but it also helps anybody seeking assistance to “plan for and achieve a good death.”
“As a drama therapist,” Edgar says softly, “I look a lot at roles that people play in their life, and one of the things that I really see — and this is a little bit related to a good way to die — I see that for a lot of us, a lot of our lives are spent doing. What can we do for other people, how we define ourselves by these roles that are really about what we can do, or what we have. And as people get older, of course, that role system gets smaller, and often people can’t do all the things they used to do. I think it’s really an interesting moment for people then: What is their identity, and who are they now?”
For many, dying becomes about control and autonomy, she says. “Here are the things I still can do and what I can still control are really important for some people.”
Others get spiritual. Edgar shares the example of a patient in his 70s who’d been diagnosed with ALS and lost the ability to do many of the things he loved. “He decided that he was ready, and he and his wife kind of describe it that ‘his spirit had outgrown his body.’ He was on hospice care and he chose to stop eating and drinking, and the wife had a lot of support, and hospice was really excellent and supportive of them. It was a very peaceful passing for him.”
Peaceful. Especially given the circumstances of a degenerative illness, “peaceful” seems like an indispensable criterion for the “best” death.
Edgar has been particularly affected by seeing choice taken away from patients. Many of the people she worked with early in her career wanted to go home but, because of what she calls the country’s “medical model” of dying, never were able to. After helping hundreds of people with their deaths — filing wills, deciding on final treatments, aiding loved ones with the transition — she’s developed an idea of a good death that’s based on her background in psychology. You’ve heard it before: letting go.
“Ultimately, we are going into an unknown,” Edgar says. “Even when people think or have ideas about what’s next, truth is, we don’t have proof. So there is that sense of going into an unknown and do people feel ready — body, mind, and spirit? Are they really ready to go?”
Sometimes, Edgar says, the body and mind are ready, but the person isn’t emotionally there yet. Or vice versa — the person feels spiritually ready, but their body’s still holding on.
“My personal answer for the best way to die is being ready, like being physically, emotionally, spiritually ready to go.”
Before we end our conversation, she stresses a point to me: “Life and death are not opposites,” she says. “We haven’t figured out how to stop either. They’re partners.”
***
In the autumn of 2014, the story of Brittany Maynard incited conversations on this topic in average American living rooms. Maynard, a 29-year-old newlywed, was diagnosed with an incurable brain cancer that gave her seizures, double vision, headaches, and other terrible symptoms that inevitably would intensify until her almost surely agonizing death.
As she looked at that future, Maynard decided that she wanted to end her life on her own terms with the help of legal medication. Unfortunately, she lived in California, which didn’t allow doctors to write life-ending prescriptions. So Maynard, her husband, and her mother packed up and moved to Oregon, where the right to die is legally recognized.
Through the ordeal, Maynard partnered with Compassion & Choices to spread the word about her journey for a good death. Her story appeared on the cover of People magazine, was featured on CNN, the Meredith Vieira Show, in USA Today, in the op-ed pages of the New York Times — you name it. Such a young woman facing such a terrible fate: it’s compelling, even wrenching, and hard to turn away from.
Disregard your personal beliefs on the morality of this situation for a moment, and think about what you would do in the face of an agonizing terminal diagnosis. Would you seek medical care until the very last breath, demanding chemo from your deathbed? Or would you prefer to go without, letting the disease take its natural course? Which path do you fear the most?

David Grube is an Oregon family doctor who, in his own words, has “delivered babies and sung at people’s funerals.” He wants to die “feeling perfectly well, and just not wake up.” Over his 35-year career, he has prescribed life-ending drugs to about 30 patients (though “aid in dying,” as it’s often called, only became legal in Oregon — and for the first in time the United States — in 1994). He did not prescribe Maynard’s medication, but he did talk to me about the process of aiding in a patient’s death.
Grube, who is the medical director for Compassion & Choices, says that though many people ask for the drugs, few end up using them. The prescriptions require a psychological evaluation, sign-off from two different physicians, and a 15-day waiting period before they’re available. The fatal dose will be a barbiturate like pentobarbital, a sedative that’s also used in animal euthanasia — it’s the same drug as the “sleeping pill” that killed Marilyn Monroe, Grube notes — or secobarbital, a bitter anesthetic and sleep aid. Someone like Brittany Maynard would likely stir the drug into a glass of juice, drink it, then await its effects.
In her final message to the public, Maynard wrote, “The world is a beautiful place, travel has been my greatest teacher, my close friends and folks are the greatest givers. I even have a ring of support around my bed as I type. … Goodbye world. Spread good energy. Pay it forward!” Her husband, Dan Diaz, said that as she took the medication, “The mood in the house was very peaceful, very loving.” Within five minutes, she fell asleep. Then she died.
Grube says that’s usually how it goes with these cases: within an hour or two, the person stops breathing and experiences “a peaceful, simple death.” On the rare occasion when the patient takes the medication with a glass of milk or with a large dose of anticonstipation medication (vanity doesn’t automatically disappear with terminal illness), they will sometimes wake up. But when taken as prescribed, most people who choose to end their life this way will, like Maynard, pass with tranquility. It is, in a word, peaceful.
Another term for Maynard’s act is “physician-assisted suicide,” but Grube rejects that concept wholeheartedly. “They don’t want to die!” he says. “‘Suicide’ is such a harmful word … and words are scalpels; they can be healing, kind, or destructive.” Some of Grube’s allies prefer the term “physician-assisted dying,” while others talk about the “right to die.” Compassion & Choices has settled on its own values-based language to discuss cases like Brittany Maynard: “death with dignity.” Partly due to Maynard’s activism, the California legislature and Governor Jerry Brown passed the “End of Life Option Act” this October, just before the one-year anniversary of her death.
Grube says most people who ask for these prescriptions are educated, motivated, and confident. What they want, he explains, is to determine the timing of their imminent death.
Control. When a disease is controlling your body and mind, when you’ve lost pleasure in the things you once loved, when you’re in pain, when you’re suffering and you fear burdening those around you, when there’s nothing more to do but wait for death, having the power to take — or not take — life-ending drugs can be a supreme comfort. But it’s a fine line of morality.
As a philosopher and bioethicist at Vanderbilt University, John Lachs considers these situations all the time. His mother, Magda, lived to 103, but given her ever-increasing collection of age-related illnesses, he wrote in Contemporary Debates in Bioethics, “living longer seemed to her utterly pointless: the pain, the indignity and the growing communicative isolation overshadowed her native optimism and the joy she had always taken in being alive. She decided that she had had enough and she was ready to die.”
Magda stockpiled prescriptions, ready to overdose on them, but lost them in a move, according to her son. She tried to die by abstaining from food and drink, but, as Lachs put it, “there was enough love of life left in her to make this a regimen she could not sustain.”
Is it okay to help someone else die? Lachs argues that “doctors should help us through every stage of life,” including the final one. Furthermore, exercising freedom — in this case, the freedom of choice to end one’s life — is not the same as following moral rules. “We have the right to terminate our lives even if it is wrong to do so,” Lachs says — with an important caveat. “Healthy young adults who propose to kill themselves cannot demand aid from others. … The situation is altogether different with suicide that is justifiable.”
To Lachs, context is of the utmost importance. “We don’t want people to choose death over life,” he tells me. But when the end is near anyway, and the person is suffering, what’s the argument against it?
- The philosopher has developed a set of five standards for the ideal death:
- It must be after a person has exhausted his purpose; there’s got to be nothing more for him to truly do.
- Corresponding to the loss of purpose is a lessening of energy — mental and physical.
- The person’s affairs should be in order — paperwork, wills, goodbyes, all of it.
- The person should feel he’s leaving something good behind — “I didn’t live for naught.”
- The death should be quick and painless.
Lachs has seen and heard of people who are near death but linger on. “It’s so much better when the other conditions are met and they just pass on,” Lachs says. “Ideally, life is such that it gives you a chance to get ready for death.
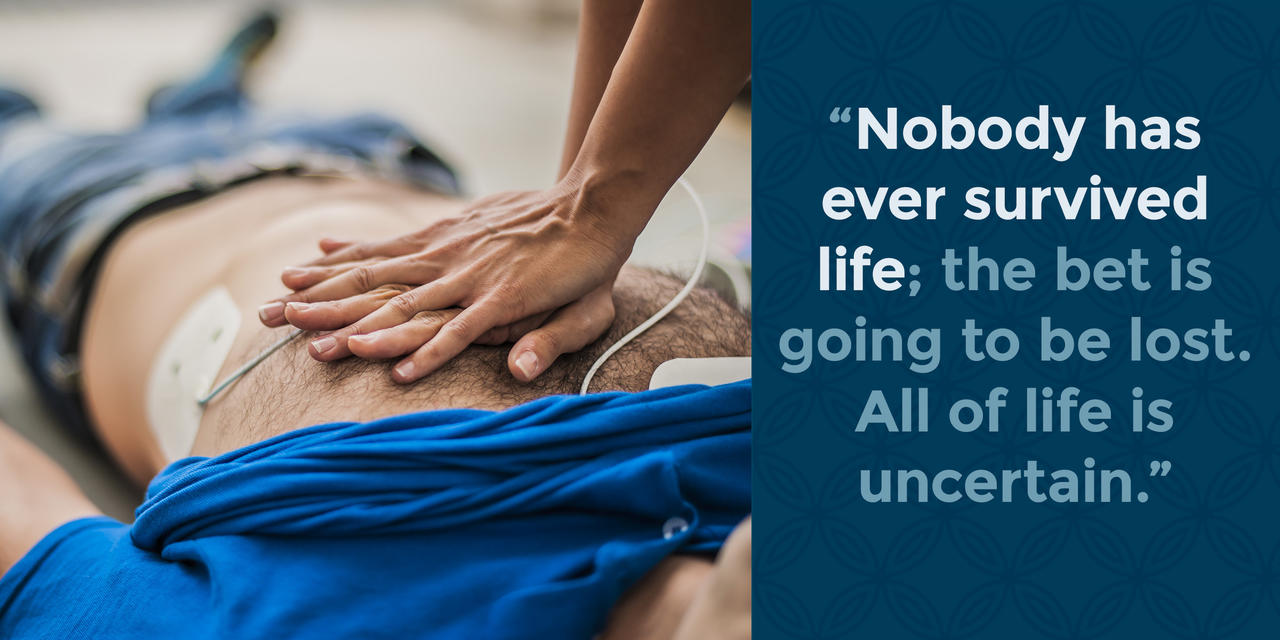
“Nobody has ever survived life. The bet is going to be lost. All of life is uncertain. We think it’s not, and contingency is the name of the game. But ultimately, we’re going to have to come to terms with the end of it.”
Magda, Lachs’ mother, finally did pass in the “subterfuge” way that hospice workers sometimes quietly administer: a nurse offered a morphine solution that depressed Magda’s lung function and finally accelerated her death.
What’s the best way to die? It’s a question that Lachs has spent time considering. His favorite answer comes from a medical colleague of his, but it’s an old yarn: being shot to death at 90 years old by an irate husband while biking away from sleeping with the gun-toting man’s wife.
Barring that, Lachs says, he’d like to die having met his own criteria — quickly, of a heart attack.
***
One of the last people I posed my question to was Doris Benbrook, director of research in gynecologic oncology at the University of Oklahoma. Her specialty is much different from the health care staff I’d spoken to previously — she studies cancer on the cellular level, particularly apoptosis, or programmed cell death. Does the microscopic level of dying give us any other ways to think about the best way to go?
In its most basic sense, a cancer cell over-multiplies and begins causing bodily trouble. “At the organ and tissue level, it eats away at vital organs. It grows, duplicates, divides.” That clogs up organs, cascades into other systems, and makes its body croak. How utterly unfair of something so tiny. Some cancers you barely feel, like the notoriously silent ovarian cancer, while others, like bone cancer, cause immense, deep pain.
Benbrook’s work with apoptosis aims to switch off that growth, to figure out how to flip the cell’s existing kill-switch so it can’t wreak such havoc. Years from now, she hopes, doctors could even use this mechanism as a cancer-prevention method.
Interestingly enough, CPR and other familiar cardiovascular attempts to keep people alive take the opposite tack: “They want to prevent cell death,” Benbrook notes. So there are many different ways to think about what the end of a cell means for the end of the human. But cells die constantly, and a few cells dying here and there don’t kill a person. Even though our cells die with us, she stressed that the microscopic level isn’t the right place to look when considering dying.
Her personal answer to the best way to die, however, was my favorite, if only for its imagery.
“I would like to die by freezing to death,” she says. “Because from what I understand of the process, it’s that you eventually just go numb and don’t feel anything. I have experienced extreme pain. I don’t ever want to do it again. I would like to go peacefully.”
Interesting. But it’s where she’d like to freeze to death that moved me.
“I would think that if I were to just sit on an iceberg floating up in the Arctic Ocean, that it would be a peaceful death. I could look up at the stars, I could think about life, and it could be a good experience.”
The frozen night air blowing over your body. The dead quiet of nature interrupted only by laps of the ocean and the occasional fish flopping out of the water. The icy sensation of your tears freezing as you look up at the Great Bear constellation for the last time. That really doesn’t seem like such a bad way to go.
But Benbrook and I come quickly back to land. “Of course I would like to have my family surrounding me, and the chances that I’m going to go sit up on an iceberg in the Arctic Ocean to die — that is not likely.” She laughs. “I’d probably be laying in a bed surrounded by loved ones. My goal would be to go peacefully.” Back to the beginning.
***
So I turn to you, brave and patient reader: from the absurd to the probable, how would you like to die? Allow yourself to think about it, in as far as you’re ready to do so. Do you want a breathing tube snaked down your throat if it becomes necessary? Do you want to be fed if you can’t do it yourself? Would you mind dying in a hospital? You can even get down to ambient details — do you want punk music blasting, a warm room, someone rubbing your swollen feet?
Whatever you wish, however deeply you’re willing to think about it, the key is to share your ideas about a good death. Talk to your family, write down what you want, and keep it somewhere they know about. Ask people about it at parties. As anyone who’s made a “pull the plug” decision can tell you, any guidance you leave will be helpful if you can’t speak for yourself on your last day.
This is your last possible decision, after all — better make it a good one.
Complete Article HERE!