— My friends came to a silent supper with their dead friends and relatives so that we could grieve our loved ones together

I don’t normally feel worried about having my friends over for dinner. Usually, I’ll be covered in splashes of soup and partially dressed when they arrive, but tonight I feel nervous.
Figuring out who to invite was complicated. Not only did they have to be available at short notice, but they had to be up for it, open to something different. Because this evening everyone has been asked to bring a plus-one … someone who has died.
As my living guests begin to arrive, bringing in the dark and subtle nip of the October air, I have the strong sense that they are not alone. I take their coats and ask them for the photo of their guest. Out of their pockets come snapshots. Smiling portraits, a moment of laughter on the stairs, a child on the beach, the ruffled ears of a French bulldog, a matriarch blurred by clouds of cigarette smoke.
In the other room, it’s quiet. The table is laid with candles, autumn leaves from the park and bright flowers, and there are twice as many plates laid at the table as there will be people in the room. I put each photo in its place. Because this is where we will serve food to the dead. We will eat, sometimes in silence, but we’ll talk and remember and, probably, cry. This is a silent supper. A feast for the dead.
It isn’t something I’d even have thought to do if I hadn’t been hanging out with witches for the series Witch for BBC Sounds and Radio 4. I’ve rarely felt comfortable or at ease talking about the dead or talking to someone who’s grieving, but for witches this seems to be different. Over the past year I’ve taken part in seances, been to an ancestor ritual and made an ancestor bottle for the spirit of a loved one. Most witches have regular rituals and altars for their ancestors and, of course, they have a dedicated season for remembrance. Witches believe that on 31 October, or Samhain, the “veil” is thin. It’s a skin between life and death that becomes more porous throughout October until, on this night, life and death can pour into each other – a lot like the world we see around us.
There are twice as many plates at the table as people in the room
This is the idea we play with at Halloween when ghouls and night terrors come knocking at our door. There’s a playfulness and joy at the idea of the afterlife being present, but in reality it’s so far out of reach. This year, I’ve decided to search for meaningful ways to remember the dead.
I decided that hosting a silent supper – historically known as a “dumb supper” – could be a good start. Eating in silence and feasting for the dead has been part of life for centuries. In England, there used to be a tradition called “chesting”.
Prof Diane Purkiss, author of English Food: A People’s History, explains: “This was even more of an Irish wake than an Irish wake. It involved having a feast that was laid out on the coffin of the deceased person. A massive blowout meal with huge treats and sugary goo. It’s honouring the dead, but it’s also quite visceral because you’re doing it on the coffin and it almost brings them physically into the feast.”
A silent supper is one step further. “What you’re describing is a ritual around the scariest and most taboo thing, which is the dead,” she says, “and this is because witches have a very special relationship with them. I define a witch as someone who doesn’t see the dead the way other people do.”
That’s certainly true. Last year my friend, colleague and witch Tatum Swithenbank reached the age at which a much loved and needed auntie had died. So their coven held a silent supper. “Sometimes we just want a space to talk about the people who have passed and there’s not really any great comfort you can give in words,” they told me. “What’s better than listening in a neutral space? That was the power of it. I don’t think you have to be a witch or be practising to do that.” They ate cheese, skull-shaped pizzas and a pumpkin pie.
Feeling underqualified to host my own silent supper, I ask for advice. “Making it dark, with only candles, really helps because people feel they are not as exposed,” says Tatum. “And it’s important to say something at the beginning. I acknowledged that grief is messy and complicated.” Another witch who loves a silent supper is Emma Griffin, who shares the ritual with her children. “It’s really nice for them to know their heritage,” she says. “We’ll have supper and talk about death, look through photos and also talk about death bringing changes. This year we are making food that my dad would like – meat and potato pie, mash and gravy.”
She advises me to make the space sacred and gentle. “I suggest giving people a dress code. When they come over your threshold, give them a little tealight. Remember, it’s a celebration of life. And you want to burn myrrh,” she says, gently but firmly as she talks me through my first ever online myrrh purchase. “It will smoke a lot, so don’t panic.”
The most pressing question of all is what on earth am I going to feed the dead? “Traditionally, the dead seem to want luxury foods,” says Purkiss. “They tend to eat dessert first, you know, life is short, eat dessert first. The dead always feel undervalued and in a way it makes them shirty so you are trying to get them to a position where they feel you value them.”
So, before the event, I threw myself (and my partner) into planning a six-course feast, my guests constantly in mind, especially the dead ones. What would they want? What would we give them if we had the chance again?
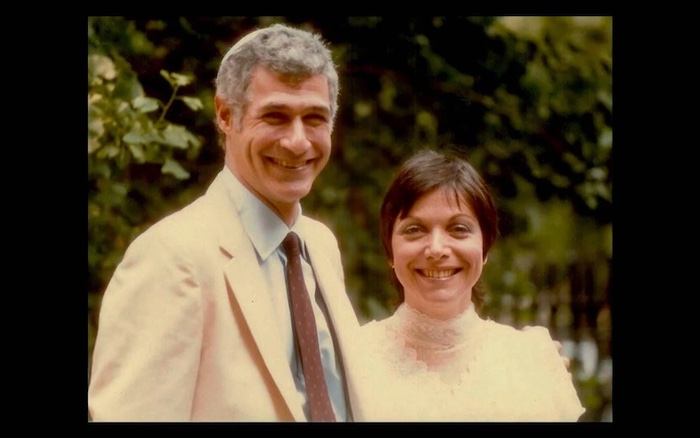
I bring Grandma Suzette. The family rarely talks about her
Purkiss approves. “Isn’t that what we all want?” she says. “When someone dies, virtually the first thing you feel is, ‘Oh, if only. If only I’d done this, or if only I’d found the time’. And the whole point of the ceremony is to give yourselves the healing chance to show great aunt Sarah you did really care.”
On the night itself, I choose to bring Grandma Suzette, who I have never met. She died when my dad was a baby. The family rarely talk about her. As my own son turned one, the loss of her for my dad and his siblings, and for me, started to ring loudly in my body. I am desperate to grieve for her.
And that’s what we’re here to do tonight. There’s a lot of normal party noise in the kitchen, but when we enter the dining room, absolutely brimming with myrrh smoke, everything softens. First, we light a candle and welcome our dead guests to the table. It feels a little strange, but maybe it should be normal. After all, eating for – and even with the dead – was once a living tradition, one that’s been purposefully rubbed away.
“There was this way of seeing the dead as beings that you interact with,” says Purkiss, adding that Catholic death rituals, such as kissing ornately decorated bones of saints, or praying in huge ossuaries stacked with bodies, went out during the Reformation. “Protestants threw all of that out, partly because they thought it had become a bit of a scam and it probably had in some cases. But the phrase throwing out the baby with the bathwater comes powerfully to mind.”
And she might be right, because it’s only minutes into the evening when it becomes painfully, joyfully clear that everyone around the table needs this communion with the dead. The phrase “I haven’t allowed myself to grieve” comes up time and again. One friend hasn’t allowed herself to grieve for her mum for 11 years. Another drifted from someone she adored and never felt she had permission to mourn them. A pal describes her love and grief for her dog Buddy as tied up with her longing for a baby. We also share joy and memories. My sister brings my other hilarious, powerful granny. A friend shares the story of a grandad who brought him pure and uncomplicated joy.<
The talking is a release, but so is acknowledging the empty places. “People did that a lot after the First World War,” Purkiss says. “They would lay places at Christmas dinner for people who had died. It makes sense.” There are three mini courses that we eat without speaking. We reflect or we write, and then we burn things we wished we could say to them.
As the courses continue to roll out, my guests talk about how much their plus-ones would have loved the feast, the wine. The chance to eat dessert again and again. We make them feel loved through food. Buddy the dog would have had a field day.
We eat too much, raise glasses of sweet mead to everyone, say the names of people out loud many, many times. We look each other straight in the eyes. No one shies away from death. By the end we all stink of myrrh, but it is as though something had shifted, for all of us. For me, I know how to talk about my grandma now, and I cannot wait to keep celebrating the people I miss in my life.
Complete Article ↪HERE↩!







:quality(70)/cloudfront-eu-central-1.images.arcpublishing.com/irishtimes/CKIPYSQKWRGVDCLSLU4Z6J6HLA.JPG)
:quality(70)/cloudfront-eu-central-1.images.arcpublishing.com/irishtimes/DKJWNBS4RZGPPNUFB2BW7KJRME.jpg)
:quality(70)/cloudfront-eu-central-1.images.arcpublishing.com/irishtimes/Q3P2A2FZFZAPFJDLMA3YG3GH2E.JPG)
