— Here’s What to Expect From Each One
Everyone who grieves experiences them, but we do it in our own way on our own timetable.
By Madeleine Burry
Whether it’s the death of a loved one, the loss of a job, the end of a relationship, or any of life’s small and large tragedies, we all grieve at some point. While you shouldn’t anticipate that your grief will resemble another person’s, there are certain common stages of grief we all experience.
Where the stages of grief originated
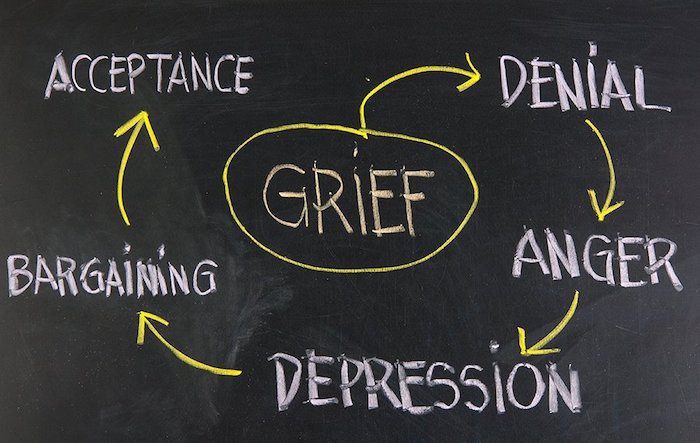
These stages of grief have typically been classified as denial, bargaining, anger, depression, and acceptance. The five stages originate from a 1969 book, On Death and Dying, written by psychiatrist Elizabeth Kübler-Ross. Though there’s some dissent about these five stages and not everyone goes through them at the same time or the same way, they’ve been accepted by psychology experts for decades and remain the model that is applied to all forms of loss.
“Coping with a loss is a very singular and unique experience to each person,” Holly Schiff, PsyD, a licensed clinical psychologist in Connecticut with Jewish Family Services of Greenwich, tells Health. Nor is the grieving process accompanied by a timetable, although often the worst symptoms peak at the six-month mark, she notes.
The grieving process is a “messy jumble of highs and lows, ebbs and flows, steps forward and backwards,” Schiff says.
Here, a look at what happens during each of these five stages, along with coping strategies for grieving.
Grief stage 1: denial
This initial stage of grief helps us to cope and survive a loss, Schiff says. “You are living in a ‘preferable’ reality, rather than actual reality,” she says. You might refuse to acknowledge the loss by keeping it to yourself and going about your life. When emotions start to overwhelm you and urge to to face the loss, you fight back and focus your mind elsewhere.
You may experience shock or disbelief while navigating denial, Arianna Galligher, LISW-S, associate director of the STAR Trauma Recovery Center at Ohio State University’s Wexner Medical Center, tells Health. “Many people describe feeling numb,” Galligher says, or struggle to connect with their emotions.
Grief stage 2: anger
Grief-related anger may lead you to ask “Why me?” or wonder why life is unfair, Schiff says.
“This response may be directed outward, inward, or both,” Galligher says. That is, it’s not unusual to blame yourself or to feel anger toward friends, family members, and others. In the case of a bad medical diagnosis, for instance, the target might be a doctor who didn’t catch the disease early on-or, someone who is fired may feel fury at their boss.
If it’s a loved one’s death you’re grieving, you could also be angry at the person-furious that they didn’t seek help sooner for a health symptom or mental anguish. If you’re grieving the end of a relationship or job, you might feel anger toward your ex or boss, blaming them for things ending.
Anger may feel unfamiliar, or maybe immature. But don’t avoid this necessary stage of grief, Schiff says. “The more you allow yourself to feel it, the more quickly it will dissipate.”
Grief stage 3: bargaining
During the bargaining phase of grief, people seek to resume their pre-loss life. Essentially, it becomes an attempt to negotiate out of the grief, Schiff says.
Many people experience guilt during this phase, too. “This response is often punctuated by ‘what if’ or ‘if only’ thoughts that seek to regain some sense of control when a person is feeling helpless or powerless over the outcome of a situation,” Galligher notes.
These thoughts may circle around and around: What if we’d skipped that errand-then we would have avoided the car accident. Or if only I’d made time for weekly date nights, we’d still be together.
Grief stage 4: depression
Facing the new, post-loss reality can lead to sadness and despair, Schiff says. “This is a natural and appropriate response to grief,” she explains.
During this phase, you may feel lonely, cry frequently, or feel disengaged from your regular activities and relationships. Depression can affect your sleep and appetite. People in this stage might find themselves losing or gaining weight, or they could feeling fatigued during the day because they’re waking up throughout the night.
Depression isn’t always displayed with a lot of emotion, however; sometimes it mean simply feel uninterested in day-to-day life and not feeling strongly about anything. If you don’t cry, it’s doesn’t mean you aren’t in the depression stage of grief. Think of “depression” as more of a stage where your emotions are muted, with grief preventing you from finding pleasure or contentment in things.
Grief stage 5: acceptance
Reaching the acceptance stage of loss doesn’t imply that you feel happiness-it simply indicates that you’ve acclimated to the loss and your new reality, Galligher says.
That means that while your emotions may stabilize, during the acceptance stage you may still feel sorrowful. During this phase, you’re learning to live with your loss, Schiff says.
While your emotions may stabilize, and you may no longer have the extremes of other stages, sadness may still occur.
Other ways of looking at grief
The Kübler-Ross theory can make grieving seem like an orderly, step-by-step process.
But in reality, mourning a loss isn’t a math equation: You may find yourself going from one stage to another and then again, Schiff says. Or, you may “even feel like you are in multiple stages at once as you cycle through a variety of emotions,” she says.
This rigidity is one of a few reasons for critiques of the Kübler-Ross model, Galligher says. This approach also assumes that all cultures conceptualize-and therefore, cope-with grief in the same way, she notes, which is not necessarily accurate. Other modern theories of grief focus less on stages and more on grief-related tasks (think: accepting the loss), Galligher says.
When to seek help
The grieving process can feel isolating and overwhelming. “It is important for people to seek help when they are grieving, and lean on family and friends for support,” Schiff says.
Grief can understandably affect your mental health, so consider reaching out for professional help if grieving-and feelings associated with the process-are making it hard for you to handle day-to-day functions or maintain relationships, Galligher says. Attending support groups or seeing a therapist can help you navigate life after loss, she says.
“If you feel like grief is taking over your life, speak to someone,” Schiff says.
Grief coping tactics
Navigating grief is innately challenging, but here are some therapist-recommended strategies to potentially ease the process:
Let your support system go work
While your grief is personal, there’s no need for it to be a solo operation. Seek support from friends, family, therapists, and support groups, Schiff recommends. She also recommends informing people in your workplace as needed. That way, “your job doesn’t expect the same ‘you’ to show up every day.”
Feel your feelings
“Give yourself permission to feel a range of emotions without judgement,” Galligher recommends. Expect challenging days and weeks to occur. It can be helpful to allocate a certain amount of time each day to grieving, Schiff says. But give yourself the grace of grieving without a deadline-again, there’s no set end-date for the process.
Prioritize self-care
Make sure you’re taking care of your physical and emotional needs: Don’t neglect sleep, exercise, and eating, Galligher says. And, avoid self-medicating with alcohol or drugs, she adds.
Plan ahead
Anniversaries, holidays, and other milestones can trigger feelings of grief, Galligher notes. “Engage in intentional self-care in anticipation” of these moments, she recommends. That might mean, for instance, deleting social media in the lead-up, taking time off of work, or reaching out to loved ones for support.
Complete Article ↪HERE↩!