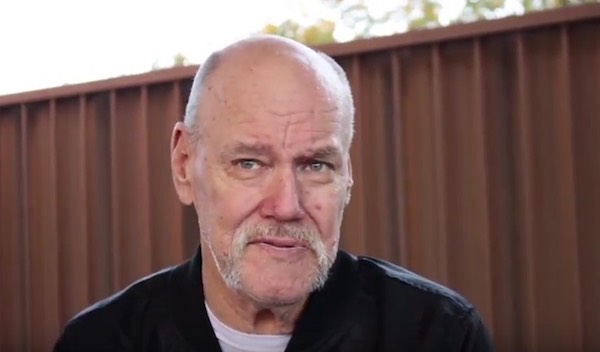
Caretaker and end-of-life doula Lisa Jeansonne helps people who are dying stay in their homes rather than having to go to a hospital.

By Liz Welter
[J]ohn “Jack” Zito, 96, doesn’t give up easily. When his wife of 73 years was facing her final days last year, Zito put every ounce of energy and effort he could muster into caring for her so that his beloved Noni could die at home.
Noni died in May; she was 95. It was about a year before she died, as her health was rapidly deteriorating, that Lisa Jeansonne began helping Zito. An experienced end-of-life caregiver, Jeansonne’s gentle presence and calm demeanor was the balm Zito sought as he cared for his ailing wife.
Zito’s eyes moistened and he dabbed at them with a handkerchief in a recent interview, remembering his wife and the care Jeansonne lovingly gave her.
“That is why Lisa is here now,” Zito said. “She looks after me. When that time comes, she’ll be here to help me, too.”
Jeansonne would go on to receive specialized training from her employer to become an end-of-life doula — a professional who can provide comfort to a dying person, and support to that person’s family. It’s part of a growing recognition across Wisconsin and nationally that caring for the dying is a skill — for some, a calling — and can be a pillar for family members.
For Zito, Jeansonne’s care for Noni, given name Margaret, helped forge a lasting emotional connection.

A World War II veteran and retired Chicago business owner, Zito has the strong, clear voice of a younger man. He enjoys puttering about the kitchen cooking, verbally sparring with Jeansonne as they duel in Scrabble games and “letting her” drive when the duo completes household errands. Noni’s death has left a chasm in Zito’s heart and Jeansonne’s companionship partially fills the void.
The Zitos literally landed in Door County after summers of sailing the Great Lakes when they retired to their favorite boating site. They immersed themselves in church and community activities in northern Door County from their home nestled in the woods near Sister Bay. Noni avidly painted watercolors of the area’s fabled scenery and wildlife, while Zito happily assumed the housework and cooking duties.
For decades their health was good and the couple relished visits from family and hosting barbecues with friends.
Old age began to catch up with the Zitos in 2016 when Noni was diagnosed with congestive heart failure. Zito said he knew the end was coming, but he was determined to care for Noni so that she could die in their cherished home in the northern Door County woods.
The pressure to care for his dying wife was fatiguing and it was emotionally draining to watch Noni decline, he said. Although Zito insisted to his children, who are scattered across the nation, including in Door County, that he didn’t need help, his family arranged for a part-time caregiver from Advocates In-Home Care in Sturgeon Bay.
Since Zito was adamant he alone could care for his wife, he devised a plan. When the hired caregiver arrived for the first day of work, he was going to be friendly, and explain he had everything well managed.
That plan slowly melted when Jeansonne knocked on Zito’s front door about two years ago. Her handshake was firm and she looked him in the eye while explaining her role to help him.

Later that day, a bond began to develop as Jeansonne and Zito sipped coffee at the kitchen table while Noni slept. Lisa said to Jack, “I know you. Your kids are about the same age as me and we used to play together in the summer.” Lisa refreshed his memory with tales of summers boating, swimming and fishing off of the Ephraim marina with his kids.
Zito’s eyes filled with tears as he told the story of that day, but he was also smiling. From the very first day, Zito said, he could see that Jeansonne’s quiet presence and easy manner was exactly the help he and his wife needed.
“That day, I saw how good Lisa was with my Noni, and, why she was practically like family,” Zito said.
New movement to die at home
While Jeansonne was hired as a caregiver, she also assumed a role that she has fulfilled dozens of times during earlier positions with families — giving specialized, attentive care to a family member who was dying.
The care Jeansonne provides isn’t medical. Rather, it focuses on doing whatever is needed to ensure the dying person is comfortable. It’s a holistic approach that offers emotional, spiritual and physical support to clients and families.
Jeansonne and other caregivers at Advocates In-Home Care are trained as end-of-life doulas. It’s part of a new movement to enable the dying to remain in their homes.
Similar to a doula who cares for and supports a woman through her pregnancy, an end-of-life doula supports a patient and the family through the dying process, said Marggie Hatala, a registered nurse and end-of-life doula in Door County.
Hatala also is a certified trainer for Doulagivers End of Life Elder Care Training Program and founded Doula Givers of Door County more than a year ago to offer free seminars about end-of-life care and also the training for certification as an end-of-life doula — or, as it is sometimes known, a “death doula.”
The end-of-life doula is there to listen and develop a relationship with the patient that transcends the illness and may last days, weeks or years depending on the prognosis, Hatala said.
“Dying and death has become institutionalized, that everyone dies in a hospital or nursing home,” Hatala said. “Most people want to die at home and they don’t want to die alone.
“People are awakening to the fact that there is a way to have a good death.”
About 25 percent of the Door County population is 65 years or older, according to the state data from 2015. In the same year, about 12 percent of the state’s population was 65 years or older.
Based on population trends, Wisconsin’s elderly population in the state will grow 72 percent by 2040, according to the Department of Health Services.
“This is happening throughout the United State — as the baby boomers are aging, there is going to be a growing need for in-home care,” Hatala said. “Door County already has a large aging population that wants to grow old in their homes.”
A former hospice nurse, Hatala said she was frustrated by being limited to providing medical care when she saw that patients wanted and benefited from having a person consistently with them as they were dying.
“I felt a true need to remain with a patient and their family without any agenda, simply to be present to them,” Hatala said. She became trained as a doula and later completed the certifications to teach and train others after she moved to Door County about five years ago.
In 2017, Hatala’s first class of caregivers from Advocates In-Home Care, including Jeansonne, became certified through Doulagivers of Door County program. Besides training to provide physical, emotional and spiritual support to the dying and their families, doulas also receive training to support family members following the death.
End-of-life doula care is paid for privately unless there is a portion of the service that is covered through the caregiver services provided to a client. The cost for end-of-life doula care is about $20 an hour.
Death can be frightening for an ailing patient and it also raises anxiety for family uncomfortable with death, said Mary Beth Williams, a hospice nurse and caregiver with Advocates In-Home Care. “Most people do not want to die alone, and they want to die at home where everything is familiar with people that they love.”
Doulas work in tandem with medical professionals and hospice programs to provide care that integrates the emotional, spiritual and physical support clients and families seek. It’s different from being a hospice nurse, Williams said, because while the nurse in hospice care focuses on a patient’s medications, a doula’s role is to provide a patient with comfort.
“As a doula, you’re aware of the pain (a patient has) and the medications they are taking, but a doula finds other ways to provide comfort; for example, if someone is short of breath, a fan on their face or elevating their head might be beneficial,” Williams said.
Hatala also conducts online training classes for people throughout Wisconsin.
The participants in Hatala’s online classes are as diverse as the regions of the state where they live. They include a paralegal from Sheboygan, a retired minister from Manitowoc and a practitioner of alternative pain management therapies from Green Bay.
They shared similar stories of being drawn to doula care after exposure to aiding the dying and finding it was a fulfilling and gratifying experience.
The Sheboygan paralegal, Shannon Shaurette, was exposed to hospice care while her father was dying from cancer seven years ago at a Milwaukee hospice.
“The hospice workers were beyond amazing to my dad, my mom and the rest of our family … and after my father died I thought about volunteering at a hospice, but the timing wasn’t right,” Shaurette said.
A friend from Vermont told Shaurette about the growing movement to die at home with the support of an end-of-life doula. She started the classes because she wanted “to be able to bring the same feeling of comfort, peace and love to others, as the staff at the hospice did for my family,” she said.

A way to a ‘good death’
For Zito, the care Jeansonne gave his wife made her “almost family.”
Prior to the day Noni died, she had been talking and sharing memories with family who had gathered at the Zito home. When she slipped into a deep sleep May 21, family members stayed at her side, holding her hand throughout the day. Zito was gone for a few minutes to make more coffee in the kitchen. When he came back, Noni had died.
“It was very peaceful,” he said. “People were with her, she was holding her son’s hand and she had a smile on her face.” Zito said he will be “eternally grateful” for the hospice care and Jeansonne’s attention to details that provided Noni and his family additional comfort.
Since Noni’s death, Jeansonne has continued to provide part-time care for Zito.
“I do the cleaning and we do grocery shopping, trips to the library or the hardware store together. We like to play Scrabble and Jack loves to read,” she said. “Jack can pretty much take care of himself, but I’m here for the help he does need.”
When Zito’s time arrives for his final journey, Jeansonne said, she will be there to help him and his family.
“He’s a wonderful man and adored his Noni. It’s a gift I can give him to make him as comfortable as possible,” she said.
Learn more about the end-of-life doula program
To learn more about Doulagivers of Door County, call Marggie Hatala at 920-495-1566 or check the website www.marggiehatala.com
Complete Article ↪HERE↩!