End-of-life treatment guidelines would help families, physicians and nurses confront the inevitable with care and compassion.
By Theresa Brown
My patient, an octogenarian with pneumonia and acute leukemia, was too frail to tolerate the standard treatment for his cancer, and trying to cure his pneumonia with intravenous antibiotics, when the leukemia had already compromised his immune system, would only have weakened him further. It made sense to switch him to “comfort measures”: to focus on alleviating his suffering rather than curing him.
It would also make sense to have general treatment guidelines for situations like this, guidelines to indicate when comfort, not cure, is most appropriate. But no such guidelines exist.
Which is why the patient’s family physician could come to the hospital, imagining himself as the cavalry, and switch the patient back to active treatment, including full resuscitation if he had a cardiac arrest. The patient was so sick that active treatment necessitated intensive care.
I took him to the intensive care unit myself. When I got there, I got into an argument with the receiving nurse about the patient’s status.
Looking to defuse the situation, the nurse apologized. “I hate these cases where there’s no point to what we’re doing,” he said.
No point. The patient’s stay in intensive care was the clinical equivalent of bailing out a sinking boat. He might gain a little time, but not much.
Modern health care accomplishes great feats of healing every day. But life ends; there are patients for whom real healing has become impossible. Their bodies have simply taken too many hits. Aggressive care can push back their death for a few days, but it is unlikely to keep them from dying soon.
These situations tend to be obvious to clinical staff, and especially nurses. We administer the hands-on care. But for those around us — physicians, families and the hospital generally — they are not at all clear, and too easily clouded by emotion. That’s why we need end-of-life treatment guidelines.
Such guidelines exist for a host of conditions: cardiac arrest, diabetes, depression. Though they can be controversial — viewed as too restrictive in some cases, in other instances too loose — they set a bar for an appropriate course of care.
‘He Nodded, Apparently Took the Sign Literally and Rushed Up the Steps’
A simple treatment guideline for clinical situations like my octogenarian patient’s might look like this: For patients who have one terminal illness that is either resistant to treatment or can’t be safely treated, combined with a second very serious illness or complication, along with a high degree of physiological frailty, physicians should consider comfort measures instead of cure.
To me, a hospice nurse, this guideline reads like common sense. But doctors who look at patients primarily as collections of individual problems, rather than very sick individuals, can miss the obvious.
Another patient I cared for in the hospital had received a liver transplant, was H.I.V. positive, and had been newly diagnosed with lymphoma. One of his sisters recited his physician’s hope-filled words back to me: “His body isn’t rejecting the liver, his H.I.V. is under control and his lymphoma can be treated.” His mental state had deteriorated to the point that he routinely tried to eat his own feces, but that symptom wasn’t considered relevant.
Health care has many financial incentives that encourage continued treatment, no matter how pointless. Liability issues arise too: Some physicians worry about being sued if they stop aggressive care for dying patients.
But my experience in hospice suggests that the fundamental issue is more basic: lack of time. According to the family of one patient I cared for — 94 years old, septic, minimally conscious, with an intestinal obstruction and a new diagnosis of cancer — no one told them how very ill she was. I would guess the staff didn’t have time, or wasn’t able to make time.
These kinds of discussions take a while because the family’s understanding of the patient’s illness must be sussed out, and their fears, worries and angers must be aired and addressed. “Comfort care” has to be explained in the context of a failing human body. That difficult, time-consuming emotional work can be avoided by simply sending patients to I.C.U. or to another hospital.
Some physicians also believe that they should have the final say about their patients’ care, especially when a patient’s health is failing. Each case is unique, and a physician’s input is invaluable. But doctors are also generally acknowledged to be unrealistically positive prognosticators. The hard truth is that every single one of us will one day reach a point where our irreparable vulnerability, and decline, cannot be denied or reversed.
As technology advances, will it continue to blur the lines between public and private? Explore what’s at stake and what you can do about it.
It helps to look at this question through the lens of medical ethics. In general, the many treatment possibilities available via modern health care are viewed as actively good, or as medical ethicists would say, beneficent. Honoring patients’ autonomy at the end of their lives is also seen as beneficent. In clinical practice, when these competing goods conflict, the treatment decisions that get made tend to be, as I have described, random and disordered.
The guidelines I propose for comfort care introduce a third term into the discussion: maleficence. Pursuing curative care that is pointless creates harm for patients and staff, who, like the frustrated I.C.U. nurse taking over my octogenarian patient, experience moral distress in these situations and a feeling of professional uselessness.
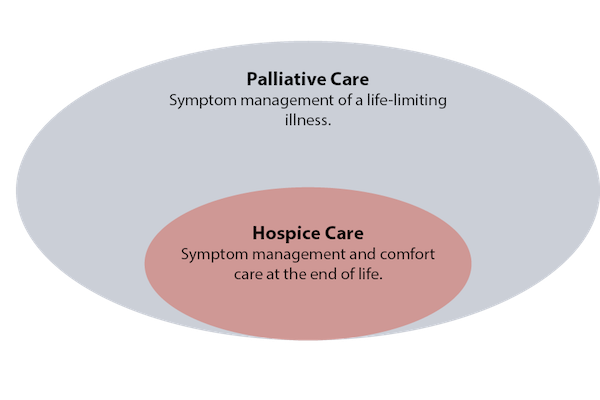
Such guidelines would introduce clarity into end-of-life decisions while still respecting patients’ autonomy. An end-of-life guideline might automatically call a palliative care clinician to the bedside to help patients and family members understand the choices available to them. The guidelines would empower nurses to advocate for comfort care, irrespective of physicians who view aggressive treatment as always being in the patient’s best interest.
For patients who choose full resuscitation and treatment despite being very ill and fragile, a guideline would ensure that they learned about comfort care. But they would never overrule a patient’s wishes for curative treatment.
The day after my octogenarian patient’s transfer to the I.C.U. he returned to our floor, back on comfort measures. I was told that the patient’s oncologist took his family physician aside and, in a scene worthy of a medical TV show, yelled at him.
The family doctor had skipped over the leukemia diagnosis, had reacted to his patient being essentially put on hospice for pneumonia, and either out of sympathy or hubris, had rushed over to the hospital to save him. But he couldn’t be saved, and we all knew that. He died a few days later.
Our society makes admissions of medical futility in the face of human frailty harder by equating “cure” with “fighting back” and “comfort” with “giving up.” A set of guidelines won’t change that. But it would help nurses and doctors acknowledge when cure is impossible, and comfort is the most compassionate, ethical route.
Complete Article ↪HERE↩!