– Creating a “Just In Case” Checklist

By Kyle Prevost
Preparing for the death of a spouse has got to be one of the worst personal finance tasks out there.
I think it might be slightly easier for us to prepare for our own demise than it is to place that burden on our spouse. That statement is especially true if your household division of labour is “the norm”, in that one spouse generally defaults to handling most of the financial planning and paperwork.
As I’ve been writing more and more about retirement lately, the idea of a “just in case” file or a “just in case” checklist has come up more and more. I’m not just talking about complicated tax issues to consider when a spouse passes away, or complex estate maneuvers. I’m more referring to how to handle the basic nuts and bolts of day-to-day life.
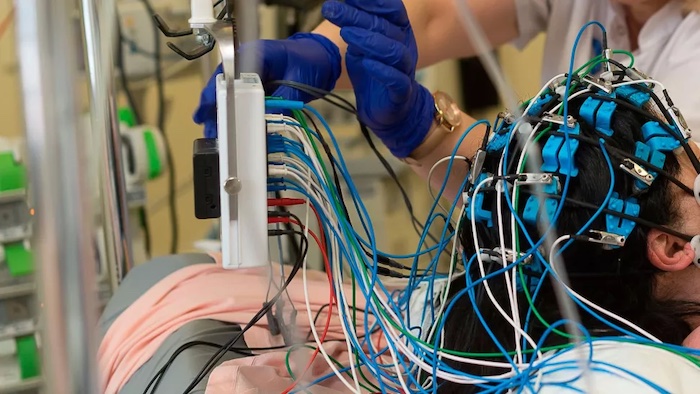
And remember, if you’ve decided that one spouse is going to be chiefly responsible for the finances, that individual does not have to pass away for a very bad scenario to occur. Cognitive decline is an unpleasant reality for many of us, and there is no obvious way to tell that someone has reached the point where they are decisively not able to handle the household finances any longer.
Planning sooner rather than later for that day is a responsible way to handle an unpleasant situation.
Financial Planning for Death
While financially planning for the death of a spouse – or your own trip to that great tax haven in the sky – is one of the least fun afternoons that I can contemplate, it is quite likely to head off some truly awful scenarios down the road.
Before preparing a “what to do when a spouse dies checklist” like the one below, let’s just get this important step out of the way first and foremost: You really do need to get that Will, Advanced Care Plan (often called a “living will” thanks to US media), and Power of Attorney set up if you haven’t already.
Yes, it’s boring – but it doesn’t have to be time consuming and expensive. I wrote about my personal experience creating a will a few years ago. It cost me $32 and took about an hour.
Also, consider taking an additional half hour to designate the recipient of non-financially valuable possessions that may not have made it into your will. I know several family squabbles that were caused by a combination of grief and irritating disputes over family heirlooms or relatively small possessions that seem much more important after someone has passed away.
What to Put In My “In Case I Die” Checklist
1) A “How To” for Notifying Service Canada of Your Death
Your OAS benefits stop when you do. Your CPP benefits on the other hand are a bit more complicated. You can read our Ultimate CPP Guide for more benefits information, but the most pressing issue will be collecting the death benefit that is part of the program.
2) Transferring Registered Accounts to Surviving Spouse
Ideally you have read our What Happens to Your TFSA and RRSP After You Die article and have identified the beneficiary and successor holder on your accounts. Those accounts will now have to be transferred to your name solely.
3) Removing Name From Shared Accounts and Utility Bills
When someone passes and is survived by their spouse, their name needs to be taken off of shared accounts, as well as utility bills, etc. A list of these accounts will come in really handy.
Settling and Cancelling Credit Cards
If you are always the one that paid the credit card, directions on how to do that, and then cancelling the credit card (or removing one name from the account) are essential.
5) A visual Step-by-Step Cecumulation Plan if You’re Still Managing Your Own Assets – or Revisiting The Idea of an Annuity/Robo advisor.
Robb Engen over at Boomer and Echo was the one who alerted me to the issue of one spouse often being the household “Chief Financial Officer” – and then passing away – leaving a huge burden of responsibility on the remaining spouse when it comes to maintaining the household decumulation plan.
Robb is a big fan of shifting over your assets to a robo advisor sooner rather than later, as they can assist a surviving spouse with basic retirement income mechanics such as selling investments and moving money to a chequing account. They’re also a great option for automating a RRIF drawdown for example.
I think as one gets older and knows their days of handling complicated decumulation strategies are starting to recede into the rearview mirror, the idea of revisiting the idea of annuities really makes a lot of sense.
Regardless of what path you choose, some combination of current-day learning, easy-to-understand graphic organizers showing a step-by-step process, and very specific directions as to what to do with investments, should really be a priority.
Remember, this stuff can be like a very intimidating new language for non-financially savvy folks. We’re looking at a situation where a spouse will have to learn that new language as they grieve and take care of 101 other things. Making things as easy as possible will be much appreciated.
6) A Passwords List
This can likely be combined with the “important stuff binder” below. A non-hackable physical document that either provides simple hints to passwords, or partial passwords, should be written out and stored in an ultrasafe location such as a safety deposit box.
Just think about all the passwords your digital footprint likely includes these days. Take a half hour and make this simple.
7) Navigating Probate and Life Insurance
As part of your will you should think about how the sequence of events will occur once you pass away. Our life insurance for seniors in Canada guide will explain both why you shouldn’t get talked into insurance that you don’t need, as well as what happens to a life insurance payment when you pass. Make sure all of the relevant contact details and the processes involved are easy to find.
8) A Physical Binder of “Important Stuff” For a Safety Deposit Box
In this day and age of online storage you might prefer to make copies of important documents and store them in a super safe online storage solution. But personally, the vast majority of folks that I know are still reassured by the idea of a physical copy of something in a safety deposit box.
Upon your death or the death of a spouse having important documents like birth certificates, marriage licenses, lists of accounts and/or loans, property deeds, pension information, contact details of professionals that you depended on such as accountants or advisers, etc – easily accessible will greatly reduce stress during an inevitable stressful time.
You can also put copies of keys in this binder as well if you really want to make life simple.
Consider leaving a copy of that binder with the trusted individual who will be the executor of your will.
Conclusion – How to Plan for the Death of a Spouse or Loved One
From my limited experience, there is no real way to prepare for the emotional trauma of losing a loved one. That said, there is no need to compound that grief by failing to prepare financially for the death of a spouse or your own demise.
Getting your affairs in order sooner rather than later can mean saving untold heartaches and headaches down the road, so I really do think it’s worth taking the time to do it right.
Complete Article ↪HERE↩!