Whether or not we want to plan for it, we all inevitably die. A hard subject for some to grasp, death can bring forth a variety of emotions, conflict, or even chaos, depending on whether or not the deceased had a pre-established estate plan.
To some extent, everyone has assets, but what happens when music is one of those assets—specifically song lyrics and the recording of those songs? We often think about the physical attributes of an estate plan after someone dies—like jewelry, amplifiers, and guitars—but how does a musician plan their legacy that will proceed their death?
Some Minnesota musicians and artists have developed assets over time and have developed their own plans for their music as part of their estate planning process.
Musician Chris Osgood, one-third of the punk-rock trio The Suicide Commandos, has spent time organizing his own musical assets with his fellow bandmates, and for himself, as he continues his own estate-planning process.
“People like myself have a tendency to forget non-physical property is still an asset,” Osgood says over the phone. “When you are doing your death planning, the first thing you think about is, who gets which guitar and objects? The last thing you think about is intellectual property, like your songs, that hopefully will continue.”
Working with musicians, artists, and other talent, attorney Ken Abdo has helped create estate plans that include music assets and legacy planning.
“An artist’s music assets, in the context of estate planning, are really just one of many assets that an artist has,” Abdo says. “The estate planning does not limit itself just to the music aspect. They may have a house, debts, other property, other children. It is part of the whole estate of an individual.”
When you are a musician, prominently known or not, you may have the additional, non-physical assets of copyright, trademark, and even name and likeness potentially included in estate planning. All of these assets together are better known in estate planning as intellectual property.
“When we are talking about music assets, we are really talking about the greater world of intellectual property,” says Abdo. “Copyright is one of those parts. There are two different copyrights involved in the recording of music: there is the underlying composition or songwriting part of it, and then there is the recorded version of that song.”
Protected under United States copyright law, a musician’s compositions and recordings are preserved for 70 years past their death. Musical assets can continue making money well past the death of the musician—an estate plan can determine who benefits from or administers these royalties. Once the copyright period expires, the music enters into the public domain, which helps explain the popularity and exorbitant recordings of songs like “Silent Night,” or other classical hits—because the originator is no longer protected, anyone can write and record the song without the penalty of payment.
Osgood and the other members of The Suicide Commandos have a musical history that spans back to 1975. Planning everything from songwriting credits to publishing rights to trademark, Osgood and his fellow bandmates recently meticulously combed through their catalog and assigned the appropriate credits for their music to each band member.
“When we put out the last record “Time Bomb,” we got a publishing deal from a company called Words and Music down in Nashville,” says Osgood. “It was mandatory when we accepted that contract, to go through each song of our entire catalog and figure out who wrote what and make sure that all parties were content with the fractions. It was easy for us to agree. Songwriting credits are pretty easy to divvy up. Song lyrics hold equal weight to the music.”
A newer technology is helping to preserve intellectual property: holograms. Holographic tours have grown in popularity amongst some musicians, and although the process to create a holographic tour is complicated, it can help protect an artist’s name and likeness, trademark rights, copyright rights, and enable an income source for heirs.
As for reputation and how musicians want people to see their image after death, they can include that in their estate planning under the right of publicity, also known as “personality rights,” which applies to 23 states and controls the commercial use of their identity.
“When you die, that is an asset, where you can bequeath the rights to your name and likeness to another person,” says Abdo. “If you died and were famous and branded, you would want to make sure that your name and likeness fall into the right hands. You would designate that person for trustee, or someone who could shepherd your legacy by making good and correct use with guidance, to keep your legacy going—it survives your death. [For] most people, when you die, you’re dead. But when you are a famous person, you have a name and likeness that has value after your death.”
Although most people do not start their estate planning process until their 50s according to a national survey, Osgood believes being pragmatic is important when dealing with assets- especially when creative assets such as music, are a part of the process.
“It’s still mailbox money and money that can go to someone who is handling my estate,” says Osgood. “I think a lot of people overlook that and don’t think a lot about it. For most of us this side of Steely Dan, it’s not that big of a deal one way or another. It could be, and it often is, if someone’s song gets picked up for a movie or an ad posthumously.”

For anyone that has music as an asset, Osgood believes that musicians should include their work in their planning, even if they do not work full-time in the industry.
“For any creative person, don’t sell yourself short or think that because you are not making a complete living from your art, whatever it happens to be, that it isn’t important or that it wouldn’t be important for future generations,” says Osgood.
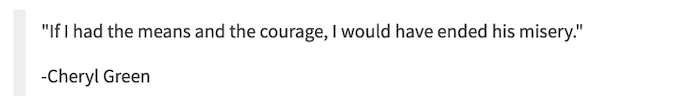
Reflecting on artists like Aretha Franklin, who recently made headlines for not having a formal estate plan, Osgood believes that musicians and others who have assets can learn from those public eye experiences.
“It’s a cautionary tale for anyone,” says Osgood. “You are taken aback that somebody of that stature hasn’t given that some thought. Maybe they didn’t because they were afraid of death, or something spooked them. It doesn’t spook me. It’s the last part of life. You have to prepare for it the same way you fill up your car before you take it on a trip.”
Complete Article ↪HERE↩!