My dad died nine years ago after he suffered a long, debilitating illness. It was an outcome we knew was inevitable when he was diagnosed 10 years prior, but that didn’t make it any less difficult to see him slowly lose all of the functions that are necessary for one to live a fruitful life. At the end, I spend two weeks at his bedside, in his home, alongside my family, and there were times where — despite the visits from the wonderful and dedicated hospice nurses, and despite knowing this was ahead of us — the emotional toll we experienced as we honored his directive to finish his life at home without invasive life saving measures was overwhelming.
I know I’m not alone here. That every day, people are dealing with the overwhelming feelings and decisions that accompany the death of a loved one. It’s something we will all experience at some point in our lives, yet it’s a topic we’d rather avoid, that we’d rather not think about or deal with until we absolutely have to.
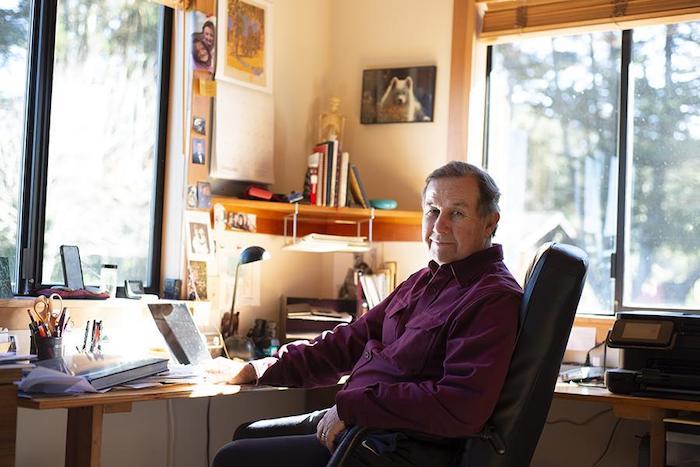
A couple of months ago I listened to a podcast that examined our stigmas and stereotypes surrounding death, and I was introduced to the concept of a “death doula.” We are generally familiar with the concept of a doula at birth — someone who is not your doctor or midwife or nurse or partner or family member — but is there to provide physical and emotional support for the mother before, during, and after the birth. A death, or end of life doula, provides physical and emotional support for those who are dying, and their families, throughout the death process. It makes so much sense! Of course this needs to be a thing! And indeed it is, right here in our community. Not long after this initial introduction to the concept, I stumbled across the Instagram profile for Threshold End of Life Doula Services, a relatively new service started by Melanie Sheckels, a local hospice nurse.
Sheckels has been a nurse for almost eight years, many of those years with cardiac patients, and has been present for deaths not only professionally, but more recently in her personal life. Her mother passed away just over a year ago, and her nursing experience gave her insight into how to counsel and advocate for her mother throughout the process. “She and I had many in depth conversations about what quality of life meant to her, and she asked me to advocate for her if she was not able to do so for herself. She had an end stage lung disease, and it was very difficult for her to talk and breathe, so she asked the doctor to just ask me to make decisions for her. Those decisions really supported her comfort and her dignity, and it created a lot of peace and healing for us both. So when I look back at that experience, I can see so many ways that could’ve been a really traumatic experience, and I was able to make it a really good one relative to the situation.”
Not all dying people and their families have the benefit of a close friend or family member with a working knowledge of what the dying process looks like, so Sheckels felt that she could use her experience to provide such a service for those families in our community.
“To be perfectly honest, a lot of my experiences around the dying and their families during the end, professionally, have been rather traumatic. Hospital deaths aren’t often pretty. Obviously we do our best, but it’s a cold sterile environment, it’s unfamiliar, and almost nothing that’s happening is within the control of the person who is doing the dying. It’s hard to maintain comfort let alone anything meaningful, ceremonial. I really noticed that all of these experiences had given me this insight and skill for being able to be present for people in a way that really improved their experience.”
So, what does it look like to be an end of life doula? Sheckels emphasizes that it’s really different for every person, every family, but that it ranges from talking through those practical issues such as advanced directives and what different medical interventions look like, to being sort of a life coach. She tries to help each person identify their priorities, and look to those priorities to determine what quality of life looks like for them. Often people have unrealistic expectations of the medical industry, that their loved one is just one intervention away, when this is often not the case. “There’s this idea that if we can then we should. This idea that death is something that has to be fought off. These things put a lot of pressure on the person that is dying.” Sometimes their experience becomes a “prolonged experience of life as a dying person.”
Sheckels helps the person create a care plan called The Best Last Three Months that addresses the emotional, spiritual, physical, and mental domains of life. “We identify what they really need to feel a sense of completion in that area. If you were to pass tomorrow, what would be the hardest thing for you to let go of? Sometimes those things are not really achievable, so we try to tease out what the significance is of that thing and find a meaningful and realistic way to do it.”
Legacy planning is also a part of the discussion. She helps people work through those big questions: “did I matter, how did I matter, and will the people that I’m leaving behind be okay without me?” For the family, she helps them work through planning vigil during active dying, and how she can help facilitate that. It may mean having a doula present for days, 24 hours at a time. Sheckels works with another end of life doula to help accommodate these more intense situations. She can also be a resource for lessening caregiver burnout by listening and allowing that person to express their emotions or staying with their loved one so they can get out and about.
The concept of an end of life doula has really emerged with the past 10 years, and while there is not yet a certification for the practice, there are various organizations that offer training. Sheckels trained with the Conscious Dying Institute. She explained that many of these organizations are working to develop a certification exam and create an industry standard, and they are also connecting with the National Hospice and Palliative Care Organization to blend their work with hospice work, much like a birth doula works alongside midwives and doctors.
Beyond the personal care of families, it’s clear that Sheckels hopes to educate the community about the dying process. As she states, “A lot of people aren’t ready to approach death in a straightforward manner.” It goes back to fear and avoidance. “We take our fear and denial and put it in a closet and don’t look at it.” Through her work, she hopes to bring that fear and denial out into the open to work through it in an honest way.
I’ve often marveled at those who work with the dying and their grieving families, and I wonder about their well-being — their ability to care for themselves and separate from those intense emotions from time to time. Sheckels eloquently shares her strategy for self-care. “To walk people to and from the gate of mortality, I have to be able to navigate that terrain for myself. I have to regularly undertake personal work to maintain the ability to be present in the moment, to connect deeply with myself and others, and to embrace the impermanence of all living things, up to and including myself. That looks like meditation, journaling, therapy, connecting with nature, and completing my own end of life care planning.”
You can find out more about Threshold End of Life Doula Services through Facebook or Instagram, or reaching out at thresholddoula@gmail.com.
Complete Article ↪HERE↩!