In just a few weeks, almost every corner of San Francisco will have death at its heel. The topic both universally experienced — and stigmatized — will be up for discussion in a variety of forms around the city.
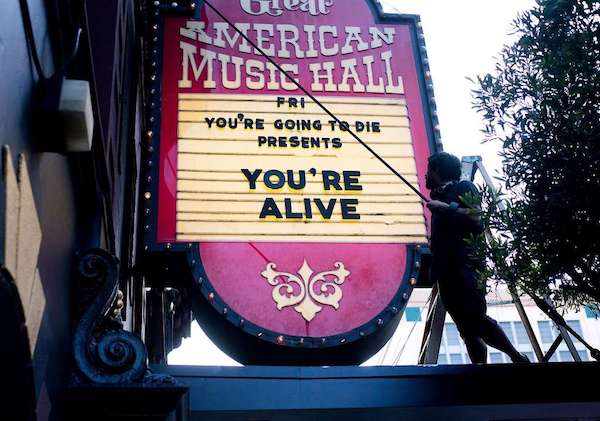
[R]eimagine, a nonprofit sprouted from IDEO, is putting on the Bay Area’s first so-called “death event series.” More than 100 events, each hosted by an individual organizer, will be offered to the public beginning on April 16 up until April 22. The nonprofit expects 7,000 people who are still alive to attend.
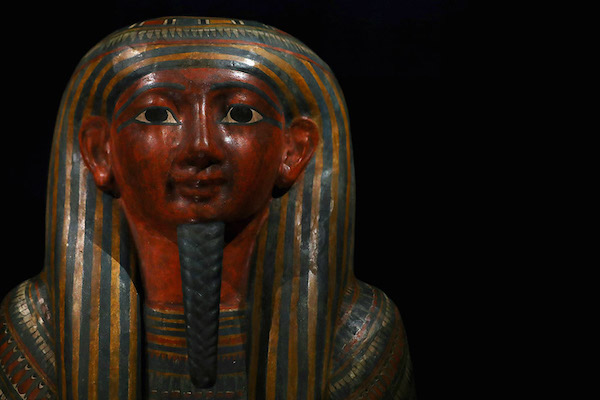
The events will cover all the ways death alters our lives — from the pragmatic (working with physicians to get Advanced Directives straightened out) to the artistic (drinking from ceramic cups made using the ashes of 200 anonymous people) to the literary (the science around the use of psychedelics and death with Dr. Richard Miller).
There will be highly-mortal film screenings (including a talk with Lee Unkrich, director of “Coco”), comedy shows (Mortified: Let’s Talk about Death, Baby), and psychodrama taken to the next level (Dead for a Day: Attend your own funeral to “altar” your life). Actress Francis McDormand will also be at the Castro Theater on April 19. for a “Theatrical Exploration of Death, Dying and Suffering.”
Aside from the arts, the events will draw on the subjects of healthcare, design, and spirituality. Brad Wolfe, Executive Director and Founder of Reimagine, wanted the event series programming to be valuable for — and reflective of — as many people as possible.
The death-positive movement — which is broad enough to contain anything from Caitlin Doughty’s Ask a Mortician YouTube series to amateur banjo sessions about the beautiful uncertainty of our mortality — has valiantly taken on the challenge of eliminating a major stigma. But in some cases, it has also been critiqued for being white-centered, and glamorizing a topic that has never, and will never, for many communities of color, feel whimsical.
That concern is exactly what Reimagine’s founders kept in mind, in the pursuit of designing an event series that would be inclusive of people outside death talk’s main demographic: middle-class white people who have the luxury of mortal musings. One such event will be hosted by Dr. Jessica Zitter, a Critical and Palliative Care Specialist at Oakland’s Highland Hospital in conversation with Pastor Corey Kennard at Glide Memorial Church.
The talk will explore the wealth of research behind racial inequities in healthcare at the end of life, and discuss the divide between dying African-American patients and a healthcare system that falls short of providing the right kind of support.
Zitter wrote an insider’s perspective on the problems with the way the dying are treated in our current medical culture in her 2016 book, “Extreme Measures: Finding a Better Path to the End of Life.” The book has been lauded by the likes of BJ Miller, a UCSF doctor and triple amputee and Lucy Kalanithi, a Stanford doctor and the widow of a Stanford doctor whose memoir on dying from cancer was released posthumously.
Her conversation with Kennard will also touch on her anecdotal experience with an aspect of healthcare that’s untaught in the medical world: finding a common language with patients who are dying that’s beyond the withdrawn and overly sterile protocol.
In her practice, she said, she underestimated the role that things like prayer, miracles, and hope mean to her African-American patients, who, “come into a hospital in their darkest hours and are met with language and concepts that feel like in a way that they’re robbing of their humanity, robbing of their opportunities for being whole.”
It was only through the years she’d been working with Betty Clark, an African-American chaplain, that she began to notice the vital components of healthcare support for her patients of color that she’d overlooked.
“There are many, many areas I had wished to delegate to others that I felt were not part of my job that are absolutely part of my job.” Zitter said.”But I really have to say that it’s really powerful to [pray with my patients]. It’s not necessarily about God, but it’s about connecting to them, and supporting them.”
The second in her series of discussion with Kennard will take place at the Oakland Museum of California on April 17., and cover the intersections of faith and medicine at the end of life.
A full event schedule is available on Reimagine’s website. Some highlights are in the slideshow above.
Complete Article ↪HERE↩!