By
[H]ow would you react if you saw people dumping 800,000 gallons of formaldehyde, a carcinogenic substance, into the earth every year?
Then witness them cutting down four million acres of forests annually? I suspect the environmentalists who fight underground oil pipes would be raising holy hell about formaldehyde and rampant destruction of trees. Yet this is what it takes to bury the U.S. dead every year. So why are environmentalists so silent?
Now, a film called “Echo Death Takeover: Changing the Funeral Industry” has been produced by The Order of Good Death, founded by funeral owner Catlin Doughty who advocates green funerals.
Some readers may wonder why I’m writing about death when I’m trained to keep people alive. But pollution of many types is currently causing serious respiratory and other health problems. Moreover, for years I’ve questioned why religious people, who say their souls go to heaven, would go to such extremes to protect their dead body by embalming, select expensive wooden caskets and then even protect the casket. And although I’m not a religious authority, don’t they always say at funerals, “Ashes to ashes and dust to dust?”
So, what to do about the current burial procedure? Formaldehyde was discovered by a chemist, August Wilhelm von Hofmann, in 1867 and it quickly replaced arsenic as the prime way to embalm bodies. Now we know that formaldehyde is a hazardous substance, highly toxic to humans. It is linked to cancer and irritates the eyes, nose and throat.
Some readers would reply, “But what about cremation? Is this more eco –friendly?” Unfortunately, where there’s fire there’s smoke. Cremation also produces harmful substances such as carbon dioxide, hydrochloric acid, sulphur dioxide, dioxin, mercury from amalgam dental fillings and carcinogens.
If the body is embalmed, smoke also contains vaporized formaldehyde which remains in the atmosphere. That is, until it bonds with water. Then we are rained on with formaldehyde. So be sure to take a good raincoat and hat if attending a rainy funeral. Besides, cremation requires heat that could be used for other purposes.
So, what is a green funeral? It’s a process called alkaline hydrolysis, also called flameless cremation or water cremation. The body is placed in a pressurized steel container filled with 95 per cent water and five per cent potassium. For the next three hours the body undergoes chemical decomposition, reducing it to soft bone fragments. This mixture of amino acids, peptides, sugar and salt can then be used for fertilizer.
Water cremation is not an illogical proposition for the next century. It’s now legal for human disposal in four U.S. states and in 14 for pets.
Are there negatives to water cremation? I imagine some would be disgusted at the dissolving of a loved one in a warm alkaline bath. But, surely, it’s less psychologically shocking than having Grandpa inserted into a fiery inferno.
Another alternative is to wrap the body in a biodegradable shroud made of cotton or unbleached bamboo, place it in a biodegradable casket in a shallow grave and let bacteria break down all these ingredients.
So, what’s going to happen? I hope that good sense will one day finally prevail and the days of spending thousands of dollars on today’s burial rites will finally end.
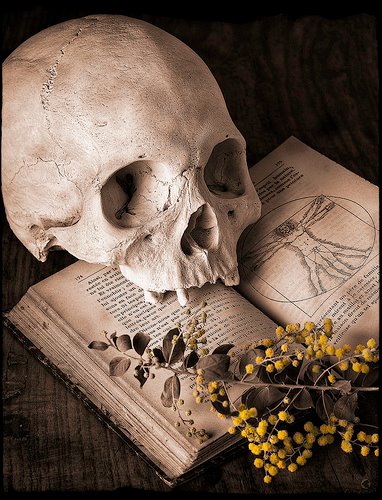
Shakespeare, in his play “Hamlet,” describes the scenario of life and death so well. He wrote: “Worms are the emperor of all diets. We fatten up all creatures to feed ourselves and we fatten ourselves for the maggots when we are dead. A man may fish with the worm that hath eat of a king and eat of the fish that hath fed of that worm.”
This is not a pleasant thought or the best bedtime reading. But regardless of how expensive the casket is the worms finally win. So, isn’t there a better way to protect the planet and return all the minerals and other elements to the earth?
So, what is my wish on death? My family knows I want a simple bench along the waterfront in Toronto where people can relax and enjoy the view. My ashes beneath can help the trees grow.
Complete Article ↪HERE↩!