By Norman Nasser, Nadia J. Pruett, Jason Sawyer and Amy E. Nolen
Monika was a 77-year-old mother of 2 and grandmother of 4 who lived for many years with mental and physical health challenges. She had bipolar disorder, which was well managed by a psychiatrist in her final years of life.
Monika was a warm and loving person who cared deeply for her family, friends, caregivers and dog, Trixie. She loved music and gardening, and enjoyed many foods, especially sweets.
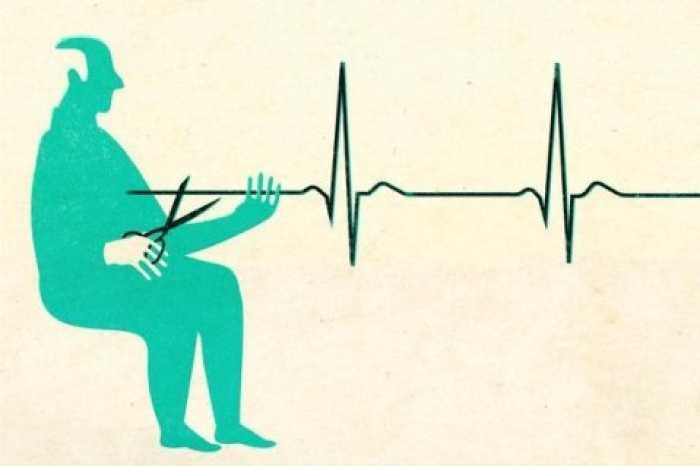
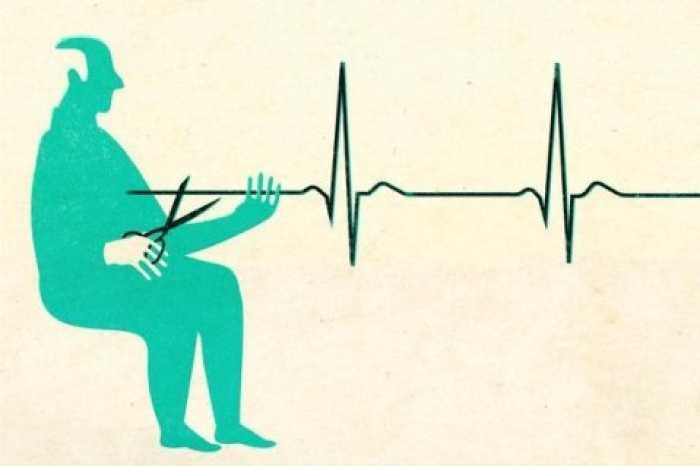
In 1996, Monika had attempted suicide, which had resulted in long-term paraplegia and associated chronic health problems, including progressive and chronic lower extremity pain. She had received numerous treatments over several years, including different classes of drugs (antispasmodics, nonsteroidal anti-inflammatory drugs, tricyclic antidepressants, anticonvulsants and opioids), medical cannabis, cortisone injections, injections of botulinum toxin and consultations with physiotherapists and physiatrists. Despite this, her pain escalated until she could no longer safely remain at home because of functional impairment from pain. She presented to the emergency department and was admitted to hospital.
In hospital, medical options for pain management were ineffective at achieving an acceptable degree of pain relief or resulted in intolerable side effects. These included trials of intravenous ketamine, lidocaine and suboxone.
Monika, with the support of her children, requested medical assistance in dying (MAiD). She was found eligible for MAiD under Bill C-7, an amendment to Canada’s assisted dying legislation that was passed in March 2021 and removed the previous requirement that a person’s natural death must be reasonably foreseeable.1 Bill C-7 includes several safeguards, including a 90-day period between initial assessment for eligibility and provision of MAiD. However, if there is concern that the patient might imminently lose capacity to consent, that period can be shortened.
During her month-long hospital admission, Monika had multi-factorial delirium that her clinicians felt placed her at risk for loss of capacity to consent to MAiD, and they shortened the 90-day assessment period.
Son’s perspective
I remember my mom as being very loving and supportive when I was a child. I relied on her warmth and wonderful personality.
At times, the last 26 years have been very difficult for us; my mom’s mental health struggles and physical deterioration often made day-to-day living incredibly difficult for her. Regardless, she felt that her quality of life was better than that of many people suffering around the world. She didn’t take life for granted.
Monika’s pain became terrible and progressive. Over the last few months of her life, she called me many times a week, crying in anguish. Regardless of what was tried — yet another specialist, medication or treatment — nothing worked. I felt helpless. My sister Nadia and I were worried that she would overdose on pain medications. I couldn’t imagine her going through that alone.
My mom decided to apply for MAiD, with our full support. When she was stressed or in pain, it was challenging for her to communicate effectively, so we were worried about how she would be assessed by her health care team, given the COVID-19 restrictions.
In hospital, the palliative care team involved the acute pain service and were incredibly supportive and compassionate. We spoke almost daily, and my mind was at ease that my mom was getting the best care possible. The compassion and patience of everyone made the experience tolerable; I felt that they were advocating for her. However, the pain persisted in spite of everything that was attempted.
When the planned waiting period of 3 months was suddenly shortened to only 48 hours, I understood. Why spend time saying goodbye when that time was spent struggling in pain? Those 2 days were a blur to me. Surprisingly, my mom had a sound sleep for the first time in months. Why? Was it the partial effectiveness of the analgesics, was it the onset of delirium or was it from the calm that came with knowing that her suffering would finally end
The last few hours came and went too quickly. Nadia, my mom and I laughed together; we cried, music played and my mom sang an old German song that I had not heard in decades. I did not say “Goodbye” or “I love you” in those brief, final seconds, but our bond was as strong as ever. Her passing was so gentle. It was impossibly difficult to be there, but I still would not change anything about that day. — Norman Nasser
Daughter’s perspective
Nothing is harder than witnessing someone you love be in excruciating pain with no relief. Mom had been in pain off and on since her accident in 1996. It had become unbearable during the 8 months before the end of her life.
My brother Norm was persistent in organizing appointments with generalists and pain specialists, as well as helping her try alternative treatments, from osteopathy to hypnotism. Nothing worked for more than a few days, if at all.
I felt incredibly helpless, knowing that there was nothing I could do to relieve her pain.
Norm and I shared a sad moment when we thought that Mom would very likely take matters into her own hands and attempt suicide. She had mentioned this as a quick method to end her pain. She would undoubtedly be alone, which was an awful thought. What if she wasn’t successful and made matters worse? We did not want a suicide attempt to be an option for our mom. We made a desperate call to Mom’s family physician, who recommended an admission to hospital for intensive management of her pain.
When Mom made the decision to pursue MAiD, I thought that the assessment period of about 3 months would give us enough time to say goodbye, reminisce and spend time together; time that we would cherish. When the assessment period was drastically shortened, I was thankful that the expedited process would fulfill Mom’s wishes, but it was a shock to know that she would be gone so soon. Time could no longer be taken for granted. It became a privilege, and it was running out very quickly.
I was allowed to visit Mom on the day before MAiD and be there with her until the procedure was over. Mom, prone to high anxiety, was the calmest she had been in a very long time. She slept through the night, which she hadn’t done in years.
The morning of the procedure, Norm, Mom and I said our goodbyes with a Tom Jones album playing, drinking German beer and enjoying her favourite foods. I felt that I needed to put on a brave face so that I wouldn’t upset Mom. It was so hard. However, I knew that Mom was at peace with her decision, and that made me feel at peace with losing her.
The void is huge. I miss her so very much. She haunts me like she promised she would! I still talk to her and hear her voice. I am so very thankful to my brother Norm for his determination in getting her the help she needed and to the medical team for listening intently and fighting for her right to be put to rest with dignity. — Nadia Pruett
Pain management nurse practitioner’s perspective
Several times a year, my palliative care colleagues reach out for assistance with patients who have complex pain management needs. I enjoy those collaborations. Becoming part of the circle of care for Monika turned out to be a very unique experience. I was told that debilitating pain had led Monika to request MAiD. Before meeting her, different thoughts went through my mind: “Is this really the goal? If pain becomes well controlled, will Monika’s outlook change?”
When I met Monika, her suffering was readily apparent. Her posture, her expressions and the sudden spasms contorting her body underscored her descriptions of pain and suffering. Despite this, Monika chose to present herself to the world with calmness and dignity. She was a very proud woman. She was inspiring.
>Monika wanted her pain to be better managed, but what was most important to her was to maintain her mind because that was “all she had left.” I outlined some new options for pain control and we agreed on a plan. I met her son, Norm, and I remember wondering, “How does he feel about all of this?” It was apparent that Norm was fully supportive of his mother’s goals and decisions. He had been tirelessly advocating for her for so long. I sensed he was finding some peace and that her request for MAiD finally provided a clear path to what she wanted.
Although the new treatments provided Monika with some brief periods of pain control, they were short-lived. Monika reported feeling clear-headed after stopping many of her longstanding pain medications and starting new ones. I like to think this increased clarity helped everyone feel just a little bit better about Monika’s decision to receive MAiD.
I saw Monika on her last day. It was amazing to see her room filled with pictures and music. Norm and Nadia were there. The delicious smells of some of Monika’s favourite foods filled my nostrils. It was nice to feel like I was not in a hospital for a brief period. In many ways, it felt like I was at a retirement celebration; a retirement from a life well lived. A retirement on Monika’s terms. It was difficult to leave the room. Helping Monika and her family find peace on her terms was a privilege and honor. — Jason Sawyer<
Palliative care physician’s perspective
At the height of the third wave of the COVID-19 pandemic, I was asked to see a new patient admitted to hospital with chronic pain. She had requested a palliative care consult, which was unusual in the absence of a life-limiting diagnosis. And so I went to meet her.
As I stood at Monika’s bedside, she was consumed by paroxysms of pain, but in her brief periods of reprieve, she showed a wry sense of humour. On her bedside tray was a small stack of pages that listed the myriad specialists who had tried to manage her complex pain. Also unusual — at the bottom was a note: she wanted to be assessed for MAiD.
I saw Monika daily over the subsequent month. I drew on the expertise of every specialist team I could for second and third opinions about pain management. Monika gamely agreed to every therapeutic option we proposed, while at the same time, from the moment of our initial encounter, she showed great conviction in her desire to move forward with MAiD.<
Bill C-7 had been enacted in Canada just weeks earlier, expanding access to MAiD for individuals who, like Monika, do not have a reasonably foreseeable natural death. I had provided MAiD under the previous legislation, and I supported C-7 in principle. But this was new territory. Suddenly I was engaging with C-7 much more quickly than I had anticipated. More than anything, Monika wanted to alleviate suffering, but I wrestled with the idea of providing MAiD to a patient who might otherwise live for years, albeit in agony.
I proceeded slowly, with valuable input from mentors. I tried to meet Monika’s request with openness. I learned of her years of living with chronic pain and the clarity of her wishes. I noted the unwavering support of her family. I reaffirmed with experts that her wish was within the law. I came to realize that what she needed now was the support of her health care team. Soon, I was navigating this terrain with a comfort I had not anticipated.
I encountered a new challenge when Monika developed medical complications that could jeopardize her future ability to consent to MAiD. She had intermittent delirium that was caused by a variety of factors, such as changes in hospital rooms, medications and a urinary tract infection for which she declined treatment. If she became persistently confused, she would lose her ability to access MAiD. We made the decision to set a MAiD provision date for that same week, only 30 days after we had first assessed her. It was a careful balance between avoiding haste and respecting Monika’s wish, and though the decision was agonizing to the medical team and her family, it was a great relief to Monika.
Monika’s medically assisted death was a moving experience. COVID-19 visitor restrictions meant only her son and daughter could be present, but the room was filled with photos and mementos from her life. The atmosphere was far from melancholic, but was suffused with calm and Monika’s palpable relief that her wishes were to be honoured. I am grateful to have had the opportunity to learn from Monika. — Amy Nolen<
360 Cases is a new type of Practice article that highlights the interpersonal and systemic aspects of health care that are seldom discussed in other Practice articles. Each comprises a brief case summary, followed by personal reflections from 2–4 people involved in the clinical encounter. One author must be a patient, family member or caregiver; the other authors may be anyone involved in the encounter (i.e., physicians, nurses, social workers, dietitians, etc.). For more information, see https://www.cmaj.ca/submission-guidelines or contact Victoria Saigle (Victoria.saigle@cmaj.ca).
Complete Article ↪HERE↩!