— In interviews with people who were dying, we learned they wanted to mark their final days with meaningful experiences and leave their affairs in order. It’s time to reset logistics, last days and legacy.

He died fuller of faith than of fears,
Fuller of resolution than of pains,
Fuller of honour than of days.
Inscription, Westminster Abbey, 1631
Why do we so often die badly? How does it happen that so many of us arrive at the end of life unprepared for the journey? Somehow, we are stumped when it comes to creating a better model of dying. Our unique qualities as individuals are lost in the processes of medical institutions and funeral homes. For those facing our last days, we have a pretty good sense of what’s involved.

Twenty years ago, I started a nonprofit organization called Older Adults Technology Services (OATS) based in New York City that helps senior citizens build new models of aging while learning technology skills. We use design thinking methods to create new programs for social impact, using approaches like co-creation, prototyping and customer satisfaction metrics.
We met with people in their hospice beds, in their homes, and on one adventurous occasion, in the Fabergé room at the Metropolitan Museum.
Recently we turned our innovation lens toward what was happening with older people in end-of-life situations to see if we could design new programs to help them. Using a design thinking methodology, we met with people who were dying and asked questions like, “What is a good day like for you?” and “If you could change one thing about your end-of-life process, what would it be?”
We met with people in their hospice beds, in their homes, and on one adventurous occasion, in the Fabergé room at the Metropolitan Museum. Some had been told they had months left, while others were living with just a few weeks in their prognosis. We visited other hospices around the country and spoke with social workers, chaplains, elder law attorneys and service providers. We read books on death and dying by Caitlin Doughty, Atul Gawande and Richard Rohr. We had weekly review sessions and talked to experts on business planning and branding and customer experience design.
We Are Failing at Dying
Here is what we learned.
We are failing at dying. Instead of a time for growth, deep connection, reflection and deliverance, our ends of life are consumed by petty distractions and institutional imperatives. The dying people we interviewed had not given up on life; rather they were full of desire to mark their final days with meaningful experiences and leave their affairs in order.
Yet almost everyone expressed sadness and frustration that they lacked a path for the right kind of death, the kind of passing that would reflect well the kind of life they had lived and the essence of the person they had become.
People described an entrenched group of institutions, resistant to change and wielding enormous power, which have grown to dominate the last stage of life — hospitals, funeral homes, home care agencies, religious organizations. When asked what they wanted instead people asked for three kinds of help: logistics, last days and legacy.
We were expecting ruminations on the duration of the soul, and instead people were preoccupied with getting the sheets clean and arranging pet care.
The Burden of Unmet Tasks
“Do you know someone who can come clean out my attic?” asked one woman in her fifties, fighting cancer and concerned that her overworked and grieving husband was sinking under the weight of daily tasks such as lawn mowing and housework. It was a startling response, in a bedside interview, to the question, “what’s most important to you now?” We were expecting ruminations on the duration of the soul, and instead people were preoccupied with getting the sheets clean and arranging pet care.
Logistics, it turns out, are top of mind for people who are dying. One woman spoke of her satisfaction in having arranged her funeral details and even set aside a dress to wear in her coffin. In an echo of Maslow’s famous hierarchy of human needs, the quotidian tasks form the base of the pyramid, and it seems difficult for people to elevate their thinking while still burdened with a laundry list of unmet tasks.
Many people commented on the need for legal help with logistics; writing wills, advance directives, health care proxies and financial plans. For many people, procrastination on legal matters resulted in family conflicts, loss of control over health decisions and anxiety about financial losses.
Unfortunately, once people were already in hospice, it was sometimes too late to interview lawyers and schedule notaries for important documents. Critical decisions about health, finances and death planning were left to caretakers and service providers, leaving the dying individual with little control over final decisions.
Death Needs a Reset
Being able to choose the location, activities and company of one’s last days was a recurrent theme. Despite being just days from passing, people expressed interest in writing articles, visiting museums, doing last trips with family members and exploring culture. My organization was able to arrange a robot tour of the Whitney Museum for one woman, who drove a telepresence robot around the museum from her hospice bed in Connecticut. At the end of the day, she drove the robot to the window and silently watched the sun setting over the river.
One clear message emerged from the interviews: death needs a reset. The handoff from doctor to hospice nurse to priest to funeral director is no longer the only path.
Finally, hospice patients were predictably focused on their legacies. We spoke for hours with people about their thoughts on post-death rituals, the value of a personalized funeral and the services that might help them express their individuality after passing. There was a great deal of openness to modern, innovative funeral approaches— “living funerals,” celebratory parties after death and eco-friendly caskets and cremations.
One clear message emerged from the interviews: death needs a reset. The handoff from doctor to hospice nurse to priest to funeral director is no longer the only path. What’s at stake is no less than our self-determination as free individuals. Like any life transition, death is a chance to explore and express ourselves in our mature stage, when we have perhaps the most important things to say. Modern culture offers endless chances for tailoring this most personal of events to our unique needs, but our social discomfort talking about death blocks us from acting.
Time for Innovative Thinking
We need a new approach to this experience, with higher expectations and more focus on dying well, not just expiring.
We found some truly innovative models in our research: “death cafes” where people gathered to explore themes of mortality and end-of-life planning; alternative hospices such as the Zen Hospice in California and Regional Hospice in Connecticut; digital death planning apps and sites such as Everplans and Everest Funerals; community learning programs run by the Plaza Jewish Community Chapel; and a national dialogue and events series sponsored by the San Francisco-based nonprofit Reimagine. Unfortunately, these programs only serve a small percentage of those who want them.
Here is a vision for reshaping end-of-life services and systems in accordance with what people asked for in the interviews.
Logistics: We need insurance and financial products that recognize the need for intensive health and personal assistance during the end-of-life period and provide enhanced benefits for people who need them. Government might create tax-free plans for legal fees associated with end-of-life plans, and the service sector should increase programs to ensure that people over the age of 60 have a legal will, advance directive and other necessary basic documents.
Last days: Incubate and accelerate a new service sector focused on proper preparation and programming for end-of-life. As major life transitions go, dying is on a par with getting married or having children, so let’s build an industry of death services to rival wedding planners and baby showers. Bring on the social entrepreneurs!
Legacy: Encourage innovation at end of life. We spoke to several innovators who had to pursue legislative recourse to overturn outdated regulations that restricted new approaches in hospice and funeral care. New York City has over 10,000 nonprofit organizations but only one nonprofit funeral home. We need to open the sector to more innovation and reduce regulatory barriers to innovation.
Fear of death and decline holds a strong sway over our minds as we age, and it’s no wonder that we are reluctant to face it. But the longevity revolution means we are living longer and expecting more from each day of our lives, and technology is adding powerful tools for managing our last days and legacies. We need a new approach to this experience, with higher expectations and more focus on dying well, not just expiring.
Complete Article ↪HERE↩!
I Promised My Sister I Would Write About How She Chose to Die
By Steven Petrow
On the day before my sister Julie died, I lay down on her bed and held her gingerly in my arms, afraid that any pressure would hurt her. She had lost so much weight that she looked like a stick figure I might have drawn when we were kids. As her body had wasted, her tumors had grown — now several of them bigger than baseballs. Her abdomen looked like the lunar landscape, with protrusions everywhere, the sources of her pain plainly visible.
Two and a half months earlier, her oncologist explained that these tumors might soon block the liver’s ability to drain properly, resulting in liver failure, usually a fast and painless death. “It will be as though you’re going to sleep,” I remember him telling us on a Zoom call.
That had not happened. Those tumors continued to grow. No matter the doses of fentanyl and morphine, Julie cried out in pain, the only time during her long illness that she suffered like that.
On the bed, Julie and I said little as I smelled her hair, rubbed her back and told her how much I’d miss her. Born five years apart (I am the elder), we were a pair of matching bookends — from our teenage years, when we’d go to our respective queer bars, to later in life, when each of us faced a cancer diagnosis. I asked if we had anything unresolved between us, as my therapist had suggested. “Nope,” my sister replied. “I don’t want to leave you all, but it’s time.”
A few hours later, she joined the rest of the family for our last supper together. I don’t remember much of the evening; either I failed to capture that memory or I’ve erased it, too painful to keep. I do recall Julie had one bite of a friend’s homemade Key lime pie. Apparently, a sweet tooth never dies, even if you are about to. Before bed, Julie hugged and kissed each of us: her wife and two daughters; my brother, Jay, and his wife; and me. Tucked in under the covers, I pulled out my iPhone to continue a ritual I’d recently begun with my siblings. From the guest couch, I texted:
Steven: Good night, sibs
Jay: Good night 😘
Julie: Good night to the best big brothers in the whole world 💚💙❤️
Jay: Love you to the moon and back!!
Steven: And to the bestest sister ever
***
Two months earlier, I joined a conversation my sister and her wife were having with a social worker, a new member of their hospice care team. They kept discussing “the MAID,” which I soon came to understand is the acronym for the New Jersey law referred to as Medical Aid in Dying. It allows New Jersey residents with terminal illnesses to choose to end their lives by taking a cocktail of life-ending medications.
This important piece of legislation was enacted in 2019, and as of last year, 186 people had chosen to die this way. (That’s a very small percentage of annual New Jersey deaths.) Julie, a lawyer, had done her research and had told me that the Garden State is one of only 11 jurisdictions (10 states and the District of Columbia) that allow medical aid in dying, also known as death with dignity and end-of-life options.
If you live in one of the other 40 states, you must wait for the Grim Reaper to pay a visit, no matter how much pain and suffering that entails. Nor can you pack up and move to New Jersey (or most other states where MAID is legal), because you must be a resident to qualify, which, at best, can take time. Time is usually not readily on hand for those who are terminally ill.
In late 2017, Julie learned she had advanced ovarian cancer. Since then, she’d endured one nine-hour surgery, six rounds of chemo, three recurrences and two clinical trials. “Enough,” my sister told her oncologist a few days before her 61st birthday, in April of this year. “I’ve decided to end treatment,” she added, to make sure he understood, and then sang, off-key, the famous Carol Burnett song, “I’m So Glad We Had This Time Together.” She asked, “How much time do I have left?” His reply: “Two or three months, at the most.”
My sister understood from Day 1 that she’d most likely die from this cancer, which, when advanced, has a mortality rate of 80 to 85 percent, according to Dr. Jason Konner, a gynecologic oncologist in New Jersey. One by one, women she had befriended in an online support group died, their last weeks and days often made awful by what Julie called “Hail Mary” treatments — drugs, many with harsh side effects, often used out of desperation or denial.
“I do not want to die like that,” my sister told me repeatedly. “This is about me taking control of my life.” She added, “I want you to write about this after I’m gone, because not enough people know about this option, even when it’s available.”
She was right. Few of our friends knew of this option, even those living in New Jersey. Kim Callinan, the chief executive of Compassion and Choices, a nonprofit that led the effort to pass New Jersey’s MAID legislation, told me these “laws are meaningless if patients are not aware they exist, which is why we focus on public education during the first five to 10 years after a jurisdiction has authorized medical aid in dying.”
The doctor’s sobering “two to three months” estimate easily qualified Julie for MAID. But that was about all that was straightforward. To hear opponents of the right to die talk, you’d think it was easy to obtain the life-ending medications. New Jersey and most other states where MAID is legal require a patient to be a mentally capable adult resident diagnosed as being terminally ill by two doctors. Julie had to request the drugs twice verbally, with a minimum of 15 days in between each request. At the time of the second ask, she had to be given the opportunity to rescind her directive. The law also required her to sign a written request in the presence of two witnesses, one of whom could have no financial interest in her death.
Julie persisted.
In recent months, lawmakers in at least nine other states have introduced MAID legislation, but opponents remain adamant. As recently as last year, Pope Francis condemned assisted suicide, saying, “We must accompany death, not provoke death or help any kind of suicide.” Other objections come from advocacy groups like the National Council on Disability, an independent federal agency that advises on government policies affecting people with disabilities; the council fears the potential exploitation of vulnerable people, especially if they feel they are a burden to family members. Julie was well aware of these concerns, but she believed MAID’s built-in safeguards prevented such exploitation.
***
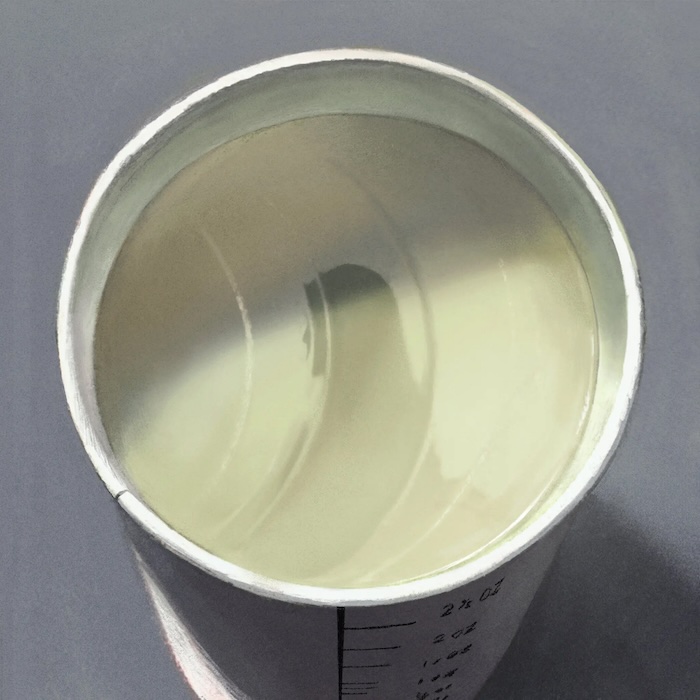
With the MAID request approved, Maddy, Julie’s spouse of 35 years, picked up the prescription from a local pharmacy. The price: $900, which is not covered by Medicare, the Department of Veterans Affairs or many private insurance plans. A study published in The Journal of the American Geriatrics Society last year found that 96 percent of people who died by medical aid in dying were white and 72 percent had at least some college education. “The reality is that communities of color, for a wide variety of reasons, also are more likely to utilize aggressive care and less likely to use other end-of-life care options, such as hospice and palliative care,” explained Ms. Callinan. People without the resources to pursue MAID may be forced to make a different choice: suffer through a painful death or take matters into their own hands. “Be sure to include these statistics when you write about this,” my sister directed me.
With her pain unabated, my sister’s next task was to choose the day she would die. Our entire family supported Julie’s decision; still, we did not want to say goodbye. We made silly excuses for why certain days were inconvenient. “I have an invitation to my friends’ 35th anniversary in Provincetown the third week of June,” I blurted out. One of Julie’s daughters said, “I’ve committed to a writing workshop starting July 4.” Julie’s best friend, Jenny, had plans to travel, too. “Please don’t let Julie schedule it before the 25th!” Jenny texted me.
Julie chose Friday, June 30. She gave us four days’ notice, which allowed for time to complete her obituary, finalize the guest list for her memorial and create the program. The day before, my brother handed me a draft of the program for one last copy edit. I’d expected her date of death to be left blank; after all, we could fill it in later. Or maybe I still hoped for a miracle that would make all this preparation unnecessary. But right there, on the program’s cover, I saw dates for the first and last days of her life, her death foretold.
Julie never wavered in her decision, which proved a godsend for the rest of us. That final morning, my sister got up early to write letters to her three girls: her wife and their two daughters. Then she called the insurance company to argue with them about a payment, trying to take one thing off Maddy’s list of to-dos. I heard her say, “I’m doing MAID at noon. I need you to get back to me before then.” That is — was — my sister.
With the sun creeping toward its zenith, Julie took one last walk in her garden, blossoming with hydrangeas, zinnias and some faded irises. Then we twice watched the video Jay had put together for her service — a lifetime of memories condensed into 14 minutes. We took one last family photo, the bookend to hundreds of others, most of them with our Julie in the center. I was confounded by how to pose — a big smile, a little smile, a frown? In looking at the photo now, I think my face looked blank, which was pretty much how I felt.
Before heading upstairs with her wife and daughters, Julie cried for a moment and said softly, “I don’t want to leave you.” A few minutes later, my sister made herself comfortable on the Ultrasuede sofa in her office. Maddy prepared the medications, and after they all recited the Serenity Prayer, my sister gulped it in one shot. Within minutes, she was unconscious, in a liminal state between life and death. Maddy gently laid her wife down on the sofa and then asked Jay and me to come upstairs. I stroked her face; I whispered to her how courageous she was to have made this decision. (After all, it’s commonly said that we lose our sense of hearing last.)
I also vowed to keep my promise to tell this story, a brother’s last act of devotion to a sister he loved beyond all measure.
Complete Article ↪HERE↩!
Why You Should Consider a Death Doula
— End-of-life doulas are compassionate and knowledgeable guides who can walk with you through death and grief.

We’re all going to die, and before that, we will probably navigate the deaths of several people we love along the way.
Too dark? Discomfort with the idea of death may be the reason that people rarely talk about it, plan for it, or teach each other how to cope with it.
“Many people in our society are death phobic and do not want to talk about it,” said Marady Duran, a social worker, doula, and educator with the International End-of-Life Doula Association. “Being an end-of-life doula has been so much more than just my bedside experiences. I am able to talk with friends, family, and strangers about death and what scares them or what plans they have. Being a doula is also about educating our communities that there are many options for how end-of-life decisions can be made.”
When you or a loved one inevitably faces death, there can be an overwhelming feeling of What do I do now? What do I do with these feelings… and all this paperwork? End-of-life doulas (also called death doulas or death coaches) are compassionate and knowledgeable guides who can walk with you through death and grief.
The experience of supporting a childhood friend through her death at the age of 27 motivated Ashley Johnson, president of the National End-of-life Doula Alliance, to commit herself to this role.
“Walking alongside her during her journey, I recognized the tremendous need for education, service, and companionship for individuals and their families facing end-of-life challenges,” Johnson said. “The passing of my dear friend only solidified my commitment to this path. I saw it as my calling to extend the same level of care and support to others who were navigating the complexities of end-of-life experiences. I firmly believe that every individual deserves the dignity of a well-supported end-of-life journey, and that starts with demystifying the process, reducing fear, and helping families achieve the proper closure they need to heal.”
What to expect from a death doula
The services provided by an end-of-life doula are actually pretty varied and flexible. Much like birth doulas, they do not provide any medical care. These are some of the services Johnson said she provides in her work:
- Advance health care planning. This might include a living will, setting up durable power of attorney for health care, and advance directive decisions. “We help individuals and their families navigate the complex process of advance healthcare planning, ensuring their wishes and choices are respected and documented,” Johnson said.
- Practical training for family caregivers. End-of-life doulas can teach caretakers and family members how to physically care for their loved ones as they near death.
- Companionship to patients. “We provide emotional support and companionship to patients, helping to ease their feelings of isolation and anxiety,” Johnson said.
- Relief for family caregivers. Caring for a dying family member can be relentless, but caregivers need time to step away and care for themselves too.
- Creating a plan for support at the patient’s time of death. A person nearing the end of their life may be comforted by many things in their environment, from the lighting, music, aromatherapy, and who’s present. A doula can help coordinate all the details.
- Grief support. “Our role extends into the grieving process, offering support to both the dying person’s loved ones and the patient during the end-of-life journey and beyond,” Johnson said.
- Vigil presence for actively dying patients. “We ensure that no one faces the end of life alone by being a comforting and compassionate presence during the active dying process,”Johnson said.
- Help with planning funeral and memorial services. Planning services is a complicated task to tackle while you are likely exhausted with grief. Doulas have been through this process many times and can be a steady hand while you make decisions.
“Our aim as death doulas is to enhance the quality of life and death for all involved,” Johnson said. “We provide a range of non-medical support, fostering an environment where individuals and their loved ones can find comfort, guidance, and a sense of peace during this profound and delicate phase of life.”
When is it time to bring in a doula?
Death doulas can provide comfort and support to both the dying person and their loved ones at any stage of the process. They can step in to help before, during, or after a death.
- At any time, before you even receive a terminal diagnosis, doulas can help you prepare emotionally and practically with planning for end-of-life wishes, advance care planning, and creating a supportive environment.
- During the end-of-life phase, doulas are more present to offer emotional, spiritual and practical support. They may be available weekly or daily, as needed.
- After death, doula services continue for the family of the deceased.
“There really is no timeline for grief,” Duran said. “Some will want to meet one or two times after the death, and some do not want to do grief work at all. It is a personal journey, and some people may take years to do the work.”
Support for an unexpected death
Not all deaths come with an advanced warning or time to prepare and plan. Even in the case of an unexpected death, an end-of-life doula can help you handle practical details and process grief. They can:
- Provide emotional support
- Help you understand the grief process
- Teach you coping strategies
- Help with arrangements, legal, and financial matters
- Help you create meaningful memorial rituals to honor the deceased
- Provide connection and community
- Listen and validate your feelings
- Provide long-term support
“My mentor Ocean Phillips, who is also a doula, always reminds me that ‘grief is another form of love,’” Duran said. “Grief gets a bad rap, and many people do not want to feel grief, but it can be transformative for many who experience it. People who go through an unexpected death of a loved one may feel guilt—‘If only I…I could have…’ The doula can hold space for them and allow them to share that. We can never fix or change, but we can stand with them and provide loving kindness along the way.”
Other professionals to help you navigate a death
Death doulas work in conjunction with many other professionals, including healthcare workers and hospice staff, to help families go through the process of death and all that follows.
“The whole team has a piece in being able to connect with those navigating grief and death. I always recognize that I am just one small part of the larger community that will help support those facing death and loss,” Duran said.
These are a few other professionals you might want to reach out to when facing the death of a loved one:
- Grief counselor
- Social worker
- Chaplain
- Community leaders
- Estate planning lawyer
- Probate lawyer
- Funeral service professional
- Financial planner
- Tax accountant (to help you file on behalf of the deceased and the estate)
- Estate liquidator or clean out-service.
Complete Article ↪HERE↩!
Are You Prepared for Death?
— A former award-winning TV news anchor wants you to learn from her mistakes
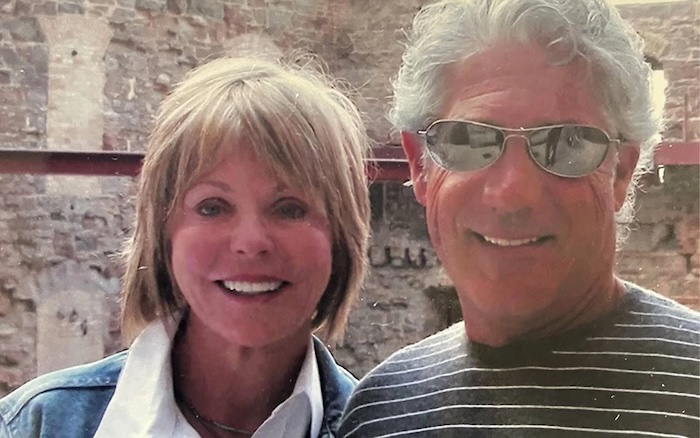
It’s been nearly five years since Pat Miles’ husband, Charles “Bucky” Zimmerman, died at age 72 after a short bout with pancreatic cancer. He was healthy, she says, so his illness came as a shock. Another unwelcome surprise? What happened after his death.
Instead of being able to grieve fully, Miles was consumed by attorney battles, tracking down account numbers, and sorting through investments. She says it was a “nightmarish” scenario where the people she thought were on her side weren’t interested in her well-being. The retired, award-winning Twin Cities TV anchor and radio host, who now lives in Arizona, was truly lost when it came to navigating her husband’s death and consumed by what she calls the “grim fog of grief.”
“If you wait until someone’s sick and dying, you’ve waited too long because you’re not going to get the information you need at that point.”
“Bucky and I had a will and a trust – I thought everything was taken care of,” Miles, 73, says. “As it turned out, nothing was taken care of. If you wait until someone’s sick and dying, you’ve waited too long because you’re not going to get the information you need at that point. You’re thinking about keeping this person alive for another day or getting them to drink a bottle of water. You’re not thinking about the account numbers, the investments, the other things you don’t know about. If you don’t do all these things when times are good, you’ll have a tough time, just like I did.”
Determined to help people avoid her mistakes, Miles wrote “Before All Is Said and Done: Practical Advice for Living and Dying Well” featuring the voices of fellow widows along with financial, legal and medical experts.
“The people who have read the book tell me they are taking action,” Miles says. “They’re making changes. They’re dealing with it. They’re thanking me for writing and speaking about this. That’s very gratifying
Turning Anger Into Action
Miles listened to hundreds of people tell their stories during her journalism career. But the experiences people tell her about now hit differently than during her time as a broadcaster.
“I tell people I used to be like you. I never would have come to listen to me talk about this book.”
“When I sign books after a speaking engagement, everybody has a story to tell me, and I’d say 90% of these are not good stories,” says Miles, who has talked to many different groups, including major financial institutions, since the book’s release. “It had me reliving a lot of it. They say my mom went through this; my mom had this happen. As a culture, we don’t want to deal with death. I tell people I used to be like you. I never would have come to listen to me talk about this book.”
Writing “Before All Is Said and Done” was anything but a cathartic experience. However, Miles doesn’t think of it as a “sad” book but an informational one.
“I was motivated to write the book because I got extremely angry – at myself and Bucky,” she recalls. “It was pure anger at being stupid and naive. Bucky died, assuming everything was going to be fine. He said I wouldn’t have to worry about anything. That wasn’t true.”
The Power of Preparation
Miles has seen first-hand how powerful it is to be prepared for death. Her co-author, Suzanne Watson, took all the advice they collected for “Before All Is Said and Done,” including changing her and her husband’s estate plan and checking in with a financial advisor. When Watson’s husband recently died, she was able to fully grieve his loss without worrying about the things that Miles struggled through.
“It gave her peace of mind because she was so prepared,” Miles says. “That’s why I wrote the book; this doesn’t have to happen to you if you educate yourself. I’ve started preparing for my death. My kids will have all the information they need when I’m gone. It’s like any other fear — you must face it. That fear starts to go away because you’re dealing with it.”
“You need someone to walk alongside you. There are many good people out there, and I wish I would have met them earlier.”
Many families avoid conversations about death because they’re uncomfortable. Miles addresses this theme throughout the book, including in the chapter “Dad Never Told Us That: The Quandary of Stepchildren.”
“It causes families to split up and siblings never to speak again,” she says. “It doesn’t have to be that way if we just take the time to communicate and properly prepare.”
She recently had a conversation with a woman whose husband was in a coma. Her stepchildren had power of attorney, changed everything, and left the woman with nothing. But her husband eventually recovered, found out what happened, and made sure his wife would be well taken care of in the future.
“If her husband hadn’t woken up, she said she would have been living in her car,” Miles recalled.
Surrounding Yourself with Allies
When she started researching the book, Miles scoured the internet for resources. She found things about grief, estate planning, and wills, but there was no what she called “How to be a Widow for Dummies.” As she dug into her project, she was surprised at the universal themes surrounding death.
“The most amazing thing is that every single person I talked to had issues – financial, attorney, family, stepchildren,” she says.
“We plan for everything in our lives — a big wedding, a baby’s birth. Death is a big event, too,” she continues. “You need to plan for this event as much as you plan for anything else in your life because it will happen to 100% of us. Dying is a very lucrative business, and the people in it want to make money, and they will make money off you if you don’t know what you’re doing.”
Miles advises people to assemble a team of trusted advisors, including a friend to take with you to meetings. She wishes she would have listened more carefully when she and Zimmerman met with financial experts and lawyers because once he died, she was on her own.
“You need someone to walk alongside you,” she says. “There are many good people out there, and I wish I would have met them earlier.”
The Little Things
Even a recent trip to a warehouse club store reminded her that there are still so many things she doesn’t know even after writing her book. When she went to renew her membership, which was in her late husband’s name, the employee helping her commented on all the rebates that come with the card. Miles was dumbfounded.
“It was in his name, but my card has my picture on it,” she says. “I didn’t get any rebates for five years. It’s stuff you don’t know. Even the little things.”
Miles doesn’t hesitate to answer when asked what she thinks Bucky would feel about all she’s done since his death.
“He’d be extremely proud,” she says. “He always was very proud of me. Bucky loved to have his picture taken, and he loved to have people talk about him. I think he’d be very happy about all of this.”
Complete Article ↪HERE↩!
Message From A Death Doula
— Everyone Needs A Death Plan (Not Just A Will)

By Hannah Frye
Death is a taboo subject in American culture. So much so that, by the time someone close to you passes, you may not have any idea how they want their affairs handled.
But according to death doula Alua Arthur, getting an “end-of-life plan” in place can make death easier to think and talk about at any age. And this plan goes far deeper than the financial and logistical items covered in a will.
Here’s how Arthur recommends making your end-of-life plan and the benefits it can bring for a well-lived life.
What is an end-of-life plan?
Arthur thinks everybody should have an-end-of-life plan. While the exact contents will be unique to each person, here are some items she recommends including:
- Your end-of-life care: When you’re nearing the end, what kind of environment do you want to be in? Where would you like to be? What type of food do you want to eat? How do you want to feel? This will help your loved ones make the best decisions for you if you’re physically unable to.
- Your body & funeral service: What do you want done with your remains? Do you want a funeral? What does it look like? Any places you’d prefer not to have it? If you don’t know your options, consider looking into it. There are so many innovative and beautiful ways to handle remains you probably haven’t heard of yet.
- Your possessions & financial affairs: This tends to be covered in a will, but can be included in your end-of-life plan as well.
- Your pets & non-relative dependents: Are there any living beings you take care of that you want to pass on information about but may not be included in your will? If so, add a plan for them in this document. Consider pets here if you have any.
Now, it’s important to remember that these end-of-life plans are meant to change and evolve with you.
If you learn about a new burial service that interests you, add it to the document. If you went to a funeral and saw something you wouldn’t want for yourself, put it in your document. This way, when you do eventually pass, your loved ones will know it’s up-to-date with your honest wishes.
Why are end-of-life plans important?
For those who prefer to shy away from discussions about death, don’t worry—you’re not alone. But here are a few reasons that making an end-of-life plan and talking more openly about death can actually help us live healthier lives:
1. Too often, we see death as “a failure”
Shoshana Ungerleider, M.D. has a unique perspective on death as an internal medicine physician and the founder of End Well–a nonprofit on a mission to change how the world thinks about the end of life.
Ungerleider says some of the strong distaste toward the topic stems from how Western medicine views death in a hospital setting. “It’s partly because we as doctors see death very, very often as a failure. And we try to do everything we can to avoid failure in medicine,” she explains.
But in the end, she notes, “Death keeps us awake to our lives.” By pushing thoughts of death away, we can actually increase the power they have over us. Making an end-of-life plan is a way to accept death for what it is and take away some of the stigma that surrounds it.
2. Speaking about it can help with death-related anxiety
On an individual level, death can be scary and anxiety-inducing to think about. The unfortunate truth is that we don’t control how we pass or when. But, what you can control (at least a little bit) is how your death is handled, hence the freeing effect of the end-of-life plan.
Knowing this part of the equation is sorted can actually bring an element of known to the unknown, potentially easing death-related anxiety.
3. A plan can help support your loved ones when the time comes
Having these big questions answered ahead of your death is a service to your loved ones who will care for you in your final days. By taking some of the work off your loved ones’s plate through pre-planning, you’ll help them grieve your passing with just a bit less stress related to logistics. Think of it as paying it forward to those who will care for you during this time.
Though it may not be accessible for everyone, working with a death doula could also prove helpful for you and your loved ones (and you can even request that in your end-of-life plan).
4. Acknowledging death can make you more present
Your considerations around death don’t need to stop once you wrap up your end-of-year plan. Instead, Arthur strongly recommends that everyone start talking about death more often. This doesn’t need to involve serious sit-down conversations. In fact, sometimes easing into it with casual topics can take away the initial shock and overwhelm.
Having more casual conversations around death can improve your quality of life and presence. Ungerleider notes that her colleague Lucy Kalanithi, M.D., often says that living and dying aren’t separate things. We’re doing both at the same time. This perspective can make death a bit less scary and unfamiliar since it reminds us that while we are living every day, we are dying every day, too.
Death keeps us awake to our lives
Making an end-of-life plan probably won’t make you completely fearless when it comes to death. But there’s a chance that it can ease your anxiety around it a bit, as well as provide support to your loved ones.
5. Don’t be afraid to ask for help
If you feel strong anxiety or fear when you think or speak about death, consider reaching out to a therapist for help. They can guide you through difficult emotions that come up and process any potential trauma that could be impacting your fear of death.
The takeaway
Death doula Alua Arthur recommends making an end-of-life plan that includes preferences related to remains, funeral services, how you’ll be cared for in your final days, and other important considerations that may not be covered in a will. If you find the topic of death uncomfortable to talk about, you’re not alone. However, getting familiar with your wishes and desires may benefit your mental health and presence, and help those around you in the long run.
Complete Article ↪HERE↩!
How to Plan for the End of Life With Cancer
— Reflect on your wishes ahead of time to help ensure they will be followed.

No one can predict exactly how long you will live with cancer, whether you have metastatic stage 4 disease (cancer that has spread to distant organs) or a less advanced stage. No matter where you are in your cancer treatment, end-of-life planning can ease some of the burden on you and your loved ones. If you take time now to reflect on your wishes, you can increase the chances you’ll achieve the outcomes you want.
Soon after any cancer diagnosis is a good time to consider end-of-life planning. Your doctor can answer questions about your prognosis, including what the realistic options are and what those treatments can achieve, says Steven Pantilat, MD, the chief of the division of palliative medicine at the University of California in San Francisco.
Laura Shoemaker, DO, the chair of palliative and supportive care at Cleveland Clinic, adds, “Care planning, ideally, is about planning for the entire trajectory of the illness, including but not limited to end of life.”
This can be done at any time and should be tailored to your needs.
Reflect on Your Values, Priorities, and Wishes
This reflection process can be difficult to initiate, but will be well worth it. It should include talking with your family, caretakers, or even a counselor.
“Each person’s plan will be a reflection of their lives, values, and personal priorities,” says Kate Mahan, LCSW, an oncology social work counselor in the Canopy Cancer Survivorship Center at Memorial Hermann the Woodlands Medical Center in Houston.
“It is often helpful to think of this as a series of discussions instead of a single talk,” she adds. “While we all know that no one lives forever, it is often very challenging to consider our own mortality.”
End-of-life planning allows your healthcare team to understand what matters most to you, says Mohana Karlekar, MD, the section chief of palliative care at Vanderbilt University Medical Center in Nashville, Tennessee.
It’s important to think about expressing your end-of-life wishes in writing if your cancer has progressed, or you’re experiencing more complications from your treatments.
This may be the time to ask yourself where you would prefer to spend your final days — for instance, at home or in a hospice house, says Eric Redard, a chaplain and the director of supportive care at High Pointe House, part of the Tufts Medicine Care at Home network, in Haverhill, Massachusetts.
Do you want to accomplish anything special? Is there a meaningful place for you to visit while you’re still mobile? “The list is endless,” says Redard.
Appoint a Decision-Maker
By communicating openly with your healthcare team, you can make more informed choices about the medical care you want if the time comes when doctors and family members have to make decisions on your behalf.
One of the most important end-of-life decisions for any person with a cancer diagnosis involves selecting someone who will be a voice for you when you can’t speak for yourself.
“Ask yourself, who would I want to make decisions for me? Anyone with cancer could — and should — do that,” says Dr. Pantilat.
Your choice can be enforced through a durable power of attorney for healthcare. It’s a type of advance directive, sometimes called a “living will.” This document names your healthcare proxy, the person who will make health-related decisions for you if you can’t communicate them to your providers.
Write Advance Directives
Outline your wishes in advance directives. The following are decisions you may want to consider including in these documents, says Redard.
- Tube feeding Nutrients and fluids are provided through an IV or via a tube in the stomach. You can choose if, when, and for how long you would like to be nourished this way.
- Pain management It’s helpful for advance directives to include how you want the healthcare team to manage your pain. You can request as much pain-numbing medicine as possible, even if it makes you fall asleep, or just enough to reduce pain while allowing you to remain aware of the people around you.
- Resuscitation and intubation You may decide that a do-not-resuscitate (DNR) order is right for you. This is a medical order written by a doctor that informs healthcare providers not to perform cardiopulmonary resuscitation (CPR) if your heart stops beating. Similarly, a do-not-intubate (DNI) order tells the healthcare team that you don’t want to be put on a ventilator if your breathing stops.
- Organ and tissue donations You may want to specify that you want to donate your organs, tissues, or both for transplantation. You may be kept on life-sustaining treatment temporarily while they’re removed for donation. To avoid any confusion, consider stating in your advance directive that you are aware of the need for this temporary intervention.
- Visitors You may wish to make it known in advance who will be able to see you and when. This may include a visit from a religious leader. For some people, such a visit can provide a sense of peace.
Even if you write advance directives, it’s a good idea to discuss them with everyone involved in your care. “There is no substitute for meaningful conversations with loved ones and medical providers about one’s care goals and preferences,” says Dr. Shoemaker.
The advance directives can also specify if you would like to receive palliative care.
Choose Palliative Care
“Palliative care provides symptom control and supportive care along the entire disease continuum, from diagnosis of advanced cancer until the end of life,” says David Hui, MD, the director of supportive and palliative care research at MD Anderson Cancer Center in Houston.
It treats a range of symptoms and stress issues such as pain, fatigue, anxiety, depression, nausea, loss of appetite, and nutrition.
“We generally advise that patients with advanced cancer gain access to specialist palliative care in a timely manner to help them with their symptom management, quality of life, and decision-making early in the illness trajectory,” says Dr. Hui.
The goal of this approach is to provide an extra layer of support not only for the patient but for loved ones as well, especially family caregivers, according to the Center to Advance Palliative Care. It is appropriate at any age and at any stage of a serious illness, and you can receive it along with curative treatment.
Consider Hospice Care
Hospice care is one branch of palliative care. It delivers medical care for people who are expected to live for six months or less, according to the Hospice Foundation of America.
You may decide to consider hospice when there is a major decline in your physical or mental status, or both, despite medical treatment. Symptoms may include increased pain, significant weight loss, extreme fatigue, shortness of breath, or weakness.
Hospice can help you live with greater comfort if you decide to stop aggressive treatments that may have weakened you physically without curing your cancer or preventing it from spreading. Hospice care does not provide curative therapies or medical intervention that is intended to extend life.
A hospice care team often includes professionals from different disciplines, such as a doctor, nurse, social worker, chaplain, and home health aide. This team can guide you in managing your physical, psychosocial, and spiritual needs. They also support family members and other close unpaid caregivers.
Find Comfort at the End of Life
Finally, remember that end-of-life planning isn’t solely about medical care. It’s also a time when you will need emotional support. So, consider mending broken relationships, surrounding yourself with pictures of family and friends, and playing music that soothes your soul.
“People can write letters to loved ones, forgiving them or reconciling,” Redard says.
End-of-life planning is a topic people tend to shy away from, but it removes the burden from those left behind. “Once it’s over,” says Redard, “there’s relief.”
Complete Article ↪HERE↩!
The Language of Hospice Can Help Us Get Better at Discussing Death

By Haley Weiss
Just because death is inevitable doesn’t make it easy or natural to talk about. In a new study, researchers wondered if hospice workers—experts in end-of-life care—had lessons to teach the rest of us when it came to speaking with patients and families about death.
Daniel Menchik, an associate professor of sociology at the University of Arizona who studies the use of language in different fields of medicine, spent eight months sitting in on team meetings at a hospice care facility that were also open to patients’ families. His goal was to study how both groups talked to each other about the impending death of the patient. His findings, which will be published in the journal Social Science & Medicine, reinforce the importance of framing death as a process rather than an outcome when caring for frightened patients and loved ones. It’s a helpful strategy that he says everyone could use when facing loss.
“People aren’t dead until they’re dead,” Menchik says. “And even then, they may not be experienced that way by the people that they are connected to, especially if they’ve had quality time with that person.”
In the study, Menchik noticed that hospice workers used three different types of verbs in meetings with family members: predictive, subjunctive, and imperative. Predictive verbs are used to assert things about the future and include words like “will” and “going to.” Imperative verbs carry a similar firmness, but include a call to action; the most common one Menchik encounters in medical settings is “should.” Subjunctive verbs convey some sort of personal stance when talking about the future. “Think,” “feel,” “want,” and many other expressive phrases fall in this category.
When a family starts hospice care, “their capabilities to engage in intense conversations [about death] are usually pretty limited,” Menchik says. But he believes that hospice workers help bridge that gap by minimizing their use of imperative verbs. In meetings he observed, imperative verbs made up just 17% of the verb phrases used by hospice professionals. That’s fairly uncommon in medicine. Menchik has also researched how surgeons speak—a field where questions about courses of treatment and illness progression demand quick and conclusive answers—and found that they use imperative verbs much more often, likely as a way of projecting that they have control over outcomes.
A higher priority in hospice is emotional management. “With the language that they’re using, they’re there as guides, not as the authorities,” says Dr. Maya Giaquinta, a pediatric resident at the Medical College of Wisconsin who worked with Menchik on the paper (and emphasized that she’s speaking in her own capacity, and not on behalf of the school). Using more predictive and subjunctive verbs allows hospice experts to orient care around current emotional needs, rather than future events.
While predictive verbs were used the most often in the meetings Menchik and Giaquinta observed, at least half of the verbs most frequently used were words that conveyed uncertainty, like “could,” “might,” and “may.” In declining to talk about future events as set in stone, the researchers found, professionals were better able to redirect conversations to the current moment and focus on anxieties and emotions.
Hospice professionals aren’t taught about care at a grammatical level in training, at least not explicitly, says Dr. Robert Gramling, a physician and the chair of palliative medicine at the University of Vermont, who was not involved with the study. Research that describes and identifies the skills experts pick up over time can be valuable for expanding the general public’s ability to think and talk about death, he says.
Gramling has studied end-of-life conversations, which he says require “thinking granularly about the words we use and how they land with other people.” When speaking to a family or a patient facing death, ask yourself: “Am I referring to this person as dying? Or am I referring to this person as living?” Gramling suggests. Such reflection grounds the conversation firmly in the present. Another question to consider about your wording: “Is that framed in the language of the person who’s experiencing it, or is it really my perspective of things?” In hospice, where patients face only one outcome, speaking with empathy and compassion along the path to it is one thing within people’s control.
Complete Article ↪HERE↩!
