As a psychotherapist, Irvin Yalom has helped others grapple with their mortality. Now he is preparing for his own end.
By Jordan Michael Smith
One morning in May, the existential psychotherapist Irvin Yalom was recuperating in a sunny room on the first floor of a Palo Alto convalescent hospital. He was dressed in white pants and a green sweater, not a hospital gown, and was quick to point out that he is not normally confined to a medical facility. “I don’t want [this article] to scare my patients,” he said, laughing. Until a knee surgery the previous month, he had been seeing two or three patients a day, some at his office in San Francisco and others in Palo Alto, where he lives. Following the procedure, however, he felt dizzy and had difficulty concentrating. “They think it’s a brain issue, but they don’t know exactly what it is,” he told me in a soft, gravelly voice. He was nonetheless hopeful that he would soon head home; he would be turning 86 in June and was looking forward to the release of his memoir, Becoming Myself, in October.
Issues of The Times Literary Supplement and The New York Times Book Review sat on the bed, alongside an iPad. Yalom had been spending his stay watching Woody Allen movies and reading novels by the Canadian writer Robertson Davies. For someone who helped introduce to American psychological circles the idea that a person’s conflicts can result from unresolvable dilemmas of human existence, among them the dread of dying, he spoke easily about his own mortality.
“I haven’t been overwhelmed by fear,” he said of his unfolding health scare. Another of Yalom’s signature ideas, expressed in books such as Staring at the Sun and Creatures of a Day, is that we can lessen our fear of dying by living a regret-free life, meditating on our effect on subsequent generations, and confiding in loved ones about our death anxiety. When I asked whether his lifelong preoccupation with death eases the prospect that he might pass away soon, he replied, “I think it probably makes things easier.”
The hope that our existential fears can be diminished inspires people around the world to email Yalom daily. In a Gmail folder labeled “Fans,” he had saved 4,197 messages from admirers in places ranging from Iran to Croatia to South Korea, which he invited me to look at. Some were simply thank-you notes, expressions of gratitude for the insights delivered by his books. In addition to textbooks and other works of nonfiction, he has written several novels and story collections. Some, such as Love’s Executioner & Other Tales of Psychotherapy and When Nietzsche Wept, have been best sellers.
As I scrolled through the emails, Yalom used his cane to tap a button that alerted the nurses’ station. A voice came through the intercom, and he explained that he needed some ice for his knee. It was the third time he’d called; he told me his pain was making it difficult to concentrate on anything else, though he was trying. Throughout his stay, his wife of more than 60 years, Marilyn, had been stopping by regularly to refresh his reading material. The day before, he’d had a visit from Georgia May, the widow of the existential psychotherapist Rollo May, who was a colleague and friend of Yalom’s. When he runs out of other things to do, he plays on his iPad or his computer, using them with the dexterity of someone half his age.
Many of Yalom’s fan letters are searing meditations on death. Some correspondents hope he will offer relief from deep-seated problems. Most of the time he suggests that they find a local therapist, but if one isn’t available and the issue seems solvable in a swift period—at this point in his career, he won’t work with patients for longer than a year—he may take someone on remotely. He is currently working with people in Turkey, South Africa, and Australia via the internet. Obvious cultural distinctions aside, he says his foreign patients are not that different from the patients he treats in person. “If we live a life full of regret, full of things we haven’t done, if we’ve lived an unfulfilled life,” he says, “when death comes along, it’s a lot worse. I think it’s true for all of us.”
Becoming Myself is clearly the memoir of a psychiatrist. “I awake from my dream at 3 a.m., weeping into my pillow,” reads the opening line. Yalom’s nightmare involves a childhood incident in which he insulted a girl. Much of the book is about the influence that his youth—particularly his relationship with his mother—has had on his life. He writes, quoting Charles Dickens, “For, as I draw closer and closer to the end, I travel in the circle, nearer and nearer to the beginning.”
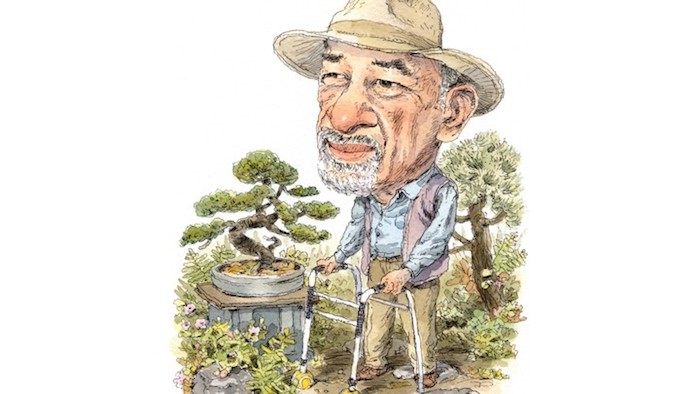
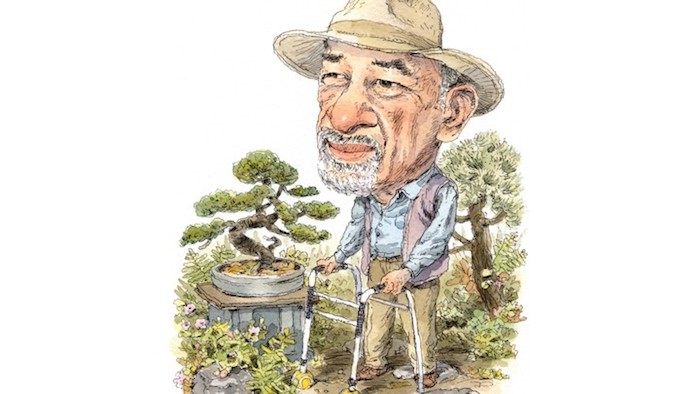
Yalom first gained fame among psychotherapists for The Theory and Practice of Group Psychotherapy. The book, published in 1970, argues that the dynamic in group therapy is a microcosm of everyday life, and that addressing relationships within a therapy group could have profound therapeutic benefits outside of it. “I’ll do the sixth revision next year,” he told me, as nurses came in and out of the room. He was sitting in a chair by the window, fidgeting. Without his signature panama hat, his sideburns, which skate away from his ears, looked especially long.
Although he gave up teaching years ago, Yalom says that until he is no longer capable, he’ll continue seeing patients in the cottage in his backyard. It is a shrink’s version of a man cave, lined with books by Friedrich Nietzsche and the Stoic philosophers. The garden outside features Japanese bonsai trees; deer, rabbits, and foxes make occasional appearances nearby. “When I feel restless, I step outside and putter over the bonsai, pruning, watering, and admiring their graceful shapes,” he writes in Becoming Myself.
Yalom sees each problem encountered in therapy as something of a puzzle, one he and his patient must work together to solve. He described this dynamic in Love’s Executioner, which consists of 10 stories of patients undergoing therapy—true tales from Yalom’s work, with names changed but few other details altered. The stories concentrate not only on Yalom’s suffering patients but also on his own feelings and thoughts as a therapist. “I wanted to rehumanize therapy, to show the therapist as a real person,” he told me.
That might not sound like the stuff of potboilers, but the book, which came out in 1989, was a commercial hit, and continues to sell briskly today. In 2003, the critic Laura Miller credited it with inaugurating a new genre. Love’s Executioner, she wrote in The New York Times, had shown “that the psychological case study could give readers what the short fiction of the time increasingly refused to deliver: the pursuit of secrets, intrigue, big emotions, plot.”
Today, the people around the world who email Yalom know him mostly from his writing, which has been translated into dozens of languages. Like David Hasselhoff, he may well be more of a star outside the United States than at home. This likely reflects American readers’ religiosity and insistence on happy endings. Mondays with Yalom are not Tuesdays With Morrie. Yalom can be morbid, and he doesn’t believe in an afterlife; he says his anxiety about death is soothed somewhat by the belief that what follows life will be the same as what preceded it. Not surprisingly, he told me, highly religious readers don’t tend to gravitate toward his books.
Yalom is candid, both in his memoir and in person, about the difficulties of aging. When two of his close friends died recently, he realized that his cherished memory of their friendship is all that remains. “It dawned on me that that reality doesn’t exist anymore,” he said sadly. “When I die, it will be gone.” The thought of leaving Marilyn behind is agonizing. But he also dreads further physical deterioration. He now uses a walker with tennis balls on the bottoms of the legs, and he has recently lost weight. He coughed frequently during our meeting; when I emailed him a month later, he was feeling better, but said of his health scare, “I consider those few weeks as among the very worst of my life.” He can no longer play tennis or go scuba diving, and he fears he might have to stop bicycling. “Getting old,” he writes in Becoming Myself, “is giving up one damn thing after another.”
In his books, Yalom emphasizes that love can reduce death anxiety, both by providing a space for people to share their fears and by contributing to a well-lived life. Marilyn, an accomplished feminist literary scholar with whom he has a close intellectual partnership, inspires him to keep living every bit as much as she makes the idea of dying excruciating. “My wife matches me book for book,” he told me at one point. But although Yalom’s email account has a folder titled “Ideas for Writing,” he said he may finally be out of book ideas. Meanwhile, Marilyn told me that she had recently helped a friend, a Stanford professor’s wife, write an obituary for her own husband.* “This is the reality of where we are in life,” she said.
Early in Yalom’s existential-psychotherapy practice, he was struck by how much comfort people derived from exploring their existential fears. “Dying,” he wrote in Staring at the Sun, “is lonely, the loneliest event of life.” Yet empathy and connectedness can go a long way toward reducing our anxieties about mortality. When, in the 1970s, Yalom began working with patients diagnosed with untreatable cancer, he found they were sometimes heartened by the idea that, by dying with dignity, they could be an example to others.
Death terror can occur in anyone at any time, and can have life-changing effects, both negative and positive. “Even for those with a deeply ingrained block against openness—those who have always avoided deep friendships—the idea of death may be an awakening experience, catalyzing an enormous shift in their desire for intimacy,” Yalom has written. Those who haven’t yet lived the life they wanted to can still shift their priorities late in life. “The same thing was true with Ebenezer Scrooge,” he told me, as a nurse brought him three pills.
For all the morbidity of existential psychotherapy, it is deeply life-affirming. Change is always possible. Intimacy can be freeing. Existence is precious. “I hate the idea of leaving this world, this wonderful life,” Yalom said, praising a metaphor devised by the scientist Richard Dawkins to illustrate the fleeting nature of existence. Imagine that the present moment is a spotlight moving its way across a ruler that shows the billions of years the universe has been around. Everything to the left of the area lit by the spotlight is over; to the right is the uncertain future. The chances of us being in the spotlight at this particular moment—of being alive—are minuscule. And yet here we are.
Yalom’s apprehension about death is allayed by his sense that he has lived well. “As I look back at my life, I have been an overachiever, and I have few regrets,” he said quietly. Still, he continued, people have “an inbuilt impulse to want to survive, to live.” He paused. “I hate to see life go.”
Complete Article ↪HERE↩!