No one wants to talk about death. But when a loved one is faced with old age or a serious illness, there are choices that need to be made. How does the patient feel about life-sustaining measures in the face of terminal illness? Does he or she have strong feelings about mechanical breathing, CPR or chemotherapy? What factors will be most important to the dying person — physical comfort, no pain, treatment costs?
As an emergency medicine doctor, Laura Vearrier, MD, a clinical assistant professor at Drexel University College of Medicine, sees plenty of family members having to make these decisions for sometimes impaired or incapacitated patients. Stress is high. Emotions are involved. What’s worse, there isn’t time for physicians to sit down and properly explain medical procedures or lay out options.
Advanced care planning allows people to maintain authority in their medical decision-making. However, the current legal framework for advance directives make them inadequate as an effective end-of-life planning tool, argues a recent paper from Vearrier, published in the HealthCare Ethics Committee Forum.
Her solution? More mandatory, frank communication between primary care physicians and their patients about the end of life and medical care — long before a patient is unhealthy.
Vearrier weighed in on problems with the current end-of-life care paradigm and how it can be improved.
What is end-of-life planning? Who does it primarily concern?
A lot of people don’t start talking about end-of-life care until they have a chronic disease, but advance care planning is really something that every adult should be thinking about early on, long before a time of illness, when there are a lot of emotions involved. End-of-life care decisions fall on a continuum that ranges from a focus on prolonging life with all available technology, to a focus primarily on comfort. There are decisions people need to make about, for instance, whether having more time alive with family and friends is preferable, even if that means prolonging suffering and giving up independence. Advance directives, commonly known as a living will, allows you to document your end-of-life medical treatment preferences. A healthcare proxy allows you to designate a person you trust as a decision maker on your behalf.
How did you become interested in the issue of end-of-life planning?
In the Emergency Department, I see many patients who are critically ill, and their families haven’t thought about their options ahead of time. When doctors present families with options about their loved one, they often don’t understand what the doctor is talking about, much less what their loved one would want. And with having to deal with the stress of a sick family member, it’s even harder to process new information.
How common are living wills?
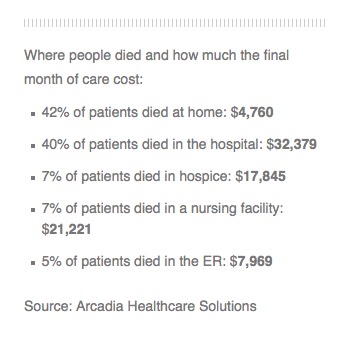
According to the 2008 Advance Directives and Advance Care Planning: Report to Congress, only 18 to 36 percent of the adult population has completed advance directives. And even those with serious medical conditions have completed advanced directives at only a slightly higher rate. A study of cancer patients in 2000 showed that only 9 percent of patients had discussed advanced directives with their oncologists, and only 23 percent of the remaining patients indicated they wished to do so. There are also differences between racial and socioeconomic groups. The report shows that white race and a higher socioeconomic status are related to a greater likelihood of having a living will.
What is the Physician Orders for Life-Sustaining Treatment Paradigm?
POLST was developed as a response to the failed process of advance directives as an end-of-life planning tool, but it is not intended to replace advanced directives. It is a health care planning tool that encourages doctors to speak with patients who are very ill and can be transferred between different health care facilities. A POLST form is completed by a health care professional rather than a patient. The POLST form identifies “Do Not Resuscitate” orders, but it also lists other treatment preferences, like whether a patient would wish to go to a hospital or stay home.
You are critical of the POLST form in your recent paper. Why?
POLST has played an important role in increasing the documentation of end-of-life preferences. However, the problem remains that people do not really understand a lot of their options. The POLST form uses a lot of specialized jargon, and it can be even more confusing than advance directives. Even social workers who discuss the forms with their patients have a poor understanding of some of their options. So when it comes time for a physician to interpret the orders, they might not really be fulfilling the patient’s treatment wishes.
What surprised you the most when researching this topic?
I was surprised about how poorly people understand their options when it comes to having to make decisions about end-of-life care and also how uncommonly people discuss it with their physicians. Physicians may not even be aware that their patients have an advance directive.
What’s the solution?
Increased communication that occurs on a routine, non-emergent basis. I think talking about the end of life and medical care should be a discussion that starts when someone is healthy, with the awareness that it’s something that may, and probably will, change over time. Since treatment preferences may change with age, health status and the current state of medical technology, discussions should occur on a yearly basis with every adult patient in the case that something happens to them. Also, everyone should be discussing their preferences with their families.
A lot of physicians are hesitant or may feel poorly prepared to have these discussions, which is why they don’t happen until someone is ill or has exhausted all of their treatments. Then lack of time becomes a barrier. To change this, it should be something that’s done on a routine basis at every yearly check-up with a primary care doctor. It’s just like the “in case of an emergency” safety protocols that are communicated on every single airplane flight. It’s repeated every time, so everyone is aware what could happen and what the procedure would be. There needs to be a culture shift, so that patients are educated and empowered about their treatment options, in case they are ever in a position where they are no longer capable of making those decisions.
Complete Article HERE!