
By Kirk Johnson
Leslie Christian recently added unusual language to her living will: After death, she hoped her remains would be reduced to soil and spread around to help out some flowers, or a tree. In essence, compost.
“It seems really gentle,” said Ms. Christian, 71, a financial adviser. “Comforting and natural.”
A bill before the Washington State Legislature would make this state the first in the nation — and probably the world, legal experts said — to explicitly allow human remains to be disposed of and reduced to soil through composting, or what the bill calls recomposition.
The prospect has drawn no public opponents in the state capital as yet, but it is a concept that sometimes raises eyebrows. Funeral directors say a common reaction to the idea, which has been explored and tested in recent scientific studies, is to cringe.
“There’s almost a revulsion at times, when you talk about human composting,” said Brian Flowers, the managing funeral director at Moles Farewell Tributes, a company north of Seattle that supports the bill.
In truth, composting is an ancient and basic method of body disposal. A corpse in the ground without embalming chemicals or a coffin, or in a quickly biodegradable coffin, becomes soil over time.
But death certificates in many states include a box that must be checked for burial or cremation, with no other options. Aboveground composting, through a mortuary process that requires no burial or burning of remains, is a new category without regulation about how it should be done or what can be done with the compost. What that means is that hardly any funeral director — even in states where laws about human remains are loosely worded — would risk offering it without state permission.
Pete Seeger, the folk singer, crooned about the idea: “If I should die before I wake, all my bone and sinew take. Put them in the compost pile to decompose a little while,” goes the song “In Dead Earnest.”
“When radishes and corn you munch you may be having me for lunch.”
In America, there are regional patterns to what comes of bodies after death. In the South and Midwest, where religious or cultural traditions run deep, more families opt for caskets and concretes vaults, and fewer choose cremation, experts say. In the Northeast, where family roots sometimes extend back centuries, people often favor burial in local cemeteries alongside ancestors.
In the Pacific Northwest, by contrast, death is treated somewhat differently, for reasons that sociologists and religious experts have long pondered. It’s a region where transient newcomers have defined the culture since pioneer days. Church attendance is among the lowest in the nation. Preservation of the environment is a central concern.
In Washington State, a larger percentage of residents are cremated than in any other state. Washington has more “green cemeteries,” which encourage a return to nature without manicured lawns and chemicals, than most states; only California and New York have more. And laws allowing physicians to help terminally ill patients hasten their deaths, known as “death with dignity,” were pioneered in the Pacific Northwest.
“It’s this interesting combination of environmental sensibility and individual choice,” David C. Sloane, a professor of public policy at the University of Southern California, said of the Northwest region. Now the prospect of legalized human composting, he said, puts many of those regional impulses in a spotlight. “It’s a test case for seeing how people think,” he said.

Jamie Pedersen, a Democratic state senator from Seattle, is leading efforts to pass the legislation to permit a composting process after death.
Democrats control both chambers of the State Legislature, and Mr. Pedersen, the bill’s sponsor, said he had enlisted support from Republicans as well. Gov. Jay Inslee, a Democrat, has taken no position, a spokeswoman said.
At a hearing this month, no one spoke in opposition, though a state association of funeral directors said that it hoped clearer information could be added to the bill about where composted remains could be distributed. It was uncertain, too, whether such a measure would be seen as a priority during a legislative session crowded with issues that may be easier for politicians to talk about and win points on.
The bill would also legalize a separate process sometimes known as water cremation or alkaline hydrolysis. Under that process, already legal in 16 states, bodies are dissolved using a mixture of heated water and lye, leaving behind bone fragments and a sterile liquid.
People are drawn to the idea of aboveground decomposition mainly for environmental reasons, Mr. Pedersen said. There’s no coffin, no chemicals, none of the fossil fuels that would be needed for cremation, and no expensive cemetery plot required. Some religious traditions also favor ideas of simplicity and of earth returning to earth.
Though the process sounds simple, it would not be cheap. Preliminary estimates suggest that it could cost at least $5,000 — less, perhaps, than an elaborate burial service, but more than the most basic cremation.
In a study last year at Washington State University, six bodies donated for the research were placed in a closed container, wrapped in organic materials like alfalfa, then bathed in a stream of air warmed by microbes, and periodically turned. Lynne Carpenter-Boggs, a professor of soil science and sustainable agriculture and the lead researcher in the study, said that after about 30 days, the bodies essentially became soil.
Fears that composted remains might smell bad or contain toxic elements — from dental fillings, for example, or pharmaceutical residues — were allayed, Dr. Carpenter-Boggs said. She said that the heat generated by micro-organisms broke down organic matter and pathogens, and levels of pollutants like cadmium and mercury were within federal limits.
“It certainly is feasible that families would take home a small portion that they could keep for a long time,” Dr. Carpenter-Boggs said. “Or families could bring home a small amount that would be interred into their landscape, placed under a loved one’s favorite tree, similar to what people do with cremains.”
Katrina Spade, the founder and chief executive of Recompose, a Seattle company that hopes to build the first facility to use the new method and conduct funeral services based around it, said the movement toward cremation — now used in more than half of deaths in the nation — has led to an erosion of essential rituals. Remains are often just picked up from a crematory, she said, and that’s that.
“This is not simply a process to convert bodies to soil; it’s also about bringing ritual and some of that ceremony back,” Ms. Spade said.
Ms. Christian, the woman who is hoping recomposition will be an option after she dies, says she has long been uncomfortable with the other choices. She has ruled out burial. And she does not like the idea of cremation because of environmental costs — emissions and climate impacts of fossil fuels used in the burning process. But her friends remain divided on the issue.
“The vast majority are like, ‘That is so cool,’” she said. “And then the other response is, ‘Oh, gross.’”
Complete Article ↪HERE↩!







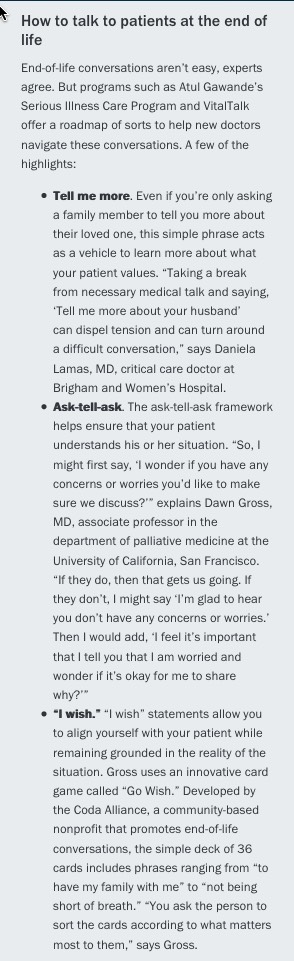 accredits medical schools, does not require clinical rotations or courses on palliative medicine or end-of-life care. Part of the issue is that these skills “can’t be taught through lectures and demonstrations,” says Susan Block, MD, a professor of psychiatry and medicine at Harvard Medical School. “The only way to improve competencies is through field practice and feedback.”
accredits medical schools, does not require clinical rotations or courses on palliative medicine or end-of-life care. Part of the issue is that these skills “can’t be taught through lectures and demonstrations,” says Susan Block, MD, a professor of psychiatry and medicine at Harvard Medical School. “The only way to improve competencies is through field practice and feedback.” 