
By Donald Hall
[J]ane Kenyon and I almost avoided marriage because her widowhood would have been so long, between us was there such a radical difference in age. And yet today it is twenty-two years since she died, of leukemia, at forty-seven—and I approach ninety. I was a high-school freshman and decided to write poems five years before Jane was born. She finished primary school in 1958, the year that I took a teaching job in her home town of Ann Arbor. With me came my wife, Kirby, and my son, Andrew; my daughter, Philippa, arrived three years later. The marriage crumbled after a decade, and I endured five wretched years of promiscuity and booze. To our endless good fortune, Jane and I found each other and, three years later, I quit teaching and we moved to New Hampshire. My children came east for their education and remained here as our neighbors. In my twenty years with her, everything in my poetic history happened again, this time to Jane: her first poem in Poetry, her first book, her second, an N.E.A. fellowship, her third book, a Guggenheim, her fourth book, multiple poetry readings, her reputation rising and spreading.
When we knew for certain that she was about to die, she told me the whereabouts of her unpublished poems, and I read them for the first time. They were dazzling, and I faxed them to the New Yorker. When we heard back from the poetry editor Alice Quinn a few days later, Jane’s eyes were open but she couldn’t see. I told her that Quinn was taking seven poems. She had stopped speaking, but her oncologist said that she could still hear.
Poetry begins with elegy, in extremity, as Gilgamesh laments the death of his companion Enkidu, watching worms crawl out of Enkidu’s neck. Homer sings of heroes as they die in battle, and Priam weeps to see the body of his son Hector dragged around the walls of Troy. Virgil follows Aeneas from the graveyard of Troy to the founding of Rome, Dido’s pyre flaming on the way. In the fifteenth century, poetry emigrated from Chaucer’s England north to the Scots, where William Dunbar wrote his elegy for the makers—in Greek, a poet is a “maker”—and grieved over twenty-five dead and dying Scots poets. Not a line from them remains. In “Lament for the Makaris,” Dunbar writes:
I that in heill wes and gladnes,
Am trublit now with gret seiknes,
And feblit with infermitie;
Timor mortis conturbat me.
He hes done petuously devour
The noble Chaucer, of makaris flour,
The Monk of Bery, and Gower, all thre;
Timor mortis conturbat me.
He hes Blind Hary and Sandy Traill
Slaine with his schour of mortall haill,
Quhilk Patrik Johnestoun might nocht fle;
Timor mortis conturbat me.
The refrain translates as “the fear of death confounds me,” but conturbat is more violent than “confounds.” A few years later, in Shakespeare’s English, Hamlet dies, Lear dies, and Prospero dies. In Milton’s “Lycidas,” the vowels of lament are golden, as erotic in sound as they are in “Paradise Lost,” but the grief is formal, not intimate; literary, not literal. Tennyson’s “In Memoriam” embodies grief before resolving it by theology. The profoundest or most mournful American lament is Whitman’s for Lincoln, “When Lilacs Last in the Dooryard Bloom’d.” A great elegy from the seventeenth century, rooted among the best poems of the English language, is Henry King’s “The Exequy”:
Accept thou Shrine of my dead Saint,
Insteed of Dirges this complaint;
And for sweet flowres to crown thy hearse,
Receive a strew of weeping verse . . .
His bride has died in her twenties: “Thou scarce had’st seen so many years / As Day tells houres . . . ” In almost a hundred lines, tetrameter couplets hurtling with a passion of grief, King looks ahead to his own death and the inevitable reunion with his bride. It is not compensatory.
Sleep on my Love in thy cold bed
Never to be disquieted!
My last good night! Thou wilt not wake
Till I thy fate shall overtake:
Till age, or grief, or sickness must
Marry my body to that dust
It so much loves; and fill the room
My heart keeps empty in thy Tomb.
When Jane and I lived in New Hampshire together, we suffered the deaths of dear friends and of cousins. Edna Powers, the granddaughter of my grandfather’s brother, was a parishioner of the South Danbury Christian Church—affectionate, large, warm, outspoken. She died, in her late fifties, on the operating table at the Franklin Hospital. I read Henry King’s “Exequy” aloud.
When death, as public as a President or as private as a lover, overwhelms us, it speaks itself in elegy’s necropoetics, be the subject a twenty-five-year-old bride or Enkidu or Edna Powers or Blind Harry or Abraham Lincoln or Jane Kenyon. “The Exequy” kept me company again when Jane died.
[W]hen I was nine or ten, Great-Uncle Wilfred felt a pain in his back at Cousin Nannie’s funeral. We buried him five months later. I woke in the night hearing myself declare, “Now death has become a reality.” My first poem, at twelve, was “The End of All.” At one point, I decided that if we flattered death, it might spare us, so I wrote “Praise for Death.” Between my two years at Oxford, I returned to the United States for my own wedding. My New Hampshire grandparents couldn’t attend—the year before, my grandfather had suffered a malfunction in a heart valve. The day after the wedding, before sailing to England, Kirby and I had only a day to drive to the farm where I had spent my childhood summers, listening to my grandfather’s stories, haying with him every afternoon, eating my grandmother’s chicken fricassee or red flannel hash for dinner. My mother’s father, Wesley Wells, had been my life’s love, the measure of everything. Kirby met Kate and Wesley; we ate a hen fresh from the henyard; we chatted; and when Kirby and I started upstairs for sleep, Wesley could not help but tell a funny story. The night he and Kate married, Kate’s cousin Freeman had wired a cowbell to their bedsprings.
Three days later, Kirby and I boarded the Queen Elizabeth for England and Oxford. In March, the airmail letter from my mother arrived—transatlantic telephone calls had to be scheduled—telling me that my family was burying my grandfather. In our Banbury Road flat, for a season, I sat at my desk writing “An Elegy for Wesley Wells,” fiercely iambic, making him the high point of the dying world. “Soon I will leave, to cross the hilly sea / And walk again among the familiar hills / In dark New Hampshire where his widow wakes.”
[T]wo and a half years after our wedding, Kirby gave birth. When the baby turned out to be a boy, we named him after my father and me, Donald Andrew Hall. We would call him Andrew. Every night, with pleasure, I gave him his 2 A.M. bottle. Every day, I worked on a poem called “My Son My Executioner.” The New Yorker published it, an anthologist put it in a college textbook, teachers assigned it, and for decades textbook anthologies reprinted it. I was the fellow whose son strapped him into the electric chair.
My son, my executioner,
I take you in my arms,
Quiet and small and just astir
And whom my body warms.
Sweet death, small son, our instrument
Of immortality,
Your cries and hungers document
Our bodily decay.
We twenty-five and twenty-two,
Who seemed to live forever,
Observe enduring life in you
And start to die together.
In Andrew’s first autumn, Kirby enrolled for her senior year of college. We had married after her junior year. I fed Andrew breakfast while his mother took classes and studied or wrote papers at the library. I gave him his bath, played with him, changed his diapers, put him down for his morning nap, changed his diapers again, walked around with the baby on my shoulder, and gave him another bottle. At noon Kirby relieved me. I liked to be part-time mother while remaining the father of my executioner.
[M]y father turned fifty-two on December 6, 1955. He died, of lung cancer, two weeks later, and we buried him, on Christmas Eve, in the Whitneyville Cemetery in Hamden, Connecticut, a block from the house he grew up in. During his seven months of dying, I drove the two hours to see him once a week. He could not speak outright of his approaching death. In a low voice that cracked and shuddered, he murmured, “if anything . . . should happen . . . to me . . .” Week after week I watched as his skin paled, he grew frailer. My mother, Lucy, rubbed his balding head. He died a few hours before one of my weekly visits. The last time I sat with him alive, I thought that every breath might be his last. I had not yet observed the brain-stem breathing—three quick breaths, a pause, and a long one—that I would see as my ninety-seven-year-old grandmother, and, twenty years later, my wife, died.
Everyone was there for my father’s funeral. My grandmother took the train from New Hampshire, from the tiny depot of Gale, three-quarters of a mile from the farm. She wore her Sunday black dress. Kirby brought Andrew, and I remember him playing with a plastic toy telephone. My mother, a widow at fifty-two, hadn’t had a night’s sleep for many months. She would live until almost ninety-one without dating another man. It was cold as we buried him in the early darkness.
For many months afterward I worked on “Christmas Eve in Whitneyville.” I used Thomas Gray’s stanza, if not the rhythms, of “Elegy Written in a Country Churchyard.” It was the best poem I had written, and it lamented that my father never did what he wanted to do. “’The things I had to miss,’ you said last week, / ‘Or thought I had to, take my breath away.’ ” I decided that, for the rest of my life, I would do what I wanted to do. I sent the poem to the Kenyon Review, the prestigious literary magazine of its day, and John Crowe Ransom accepted it, calling it “pious.”
[J]ane’s own necropoems began when her father died. During his cancer, she and I flew from New Hampshire to Michigan and, with her mother, took turns staying up all night beside him. Not long after he died, Jane’s poems attended my almost-death. Two years before her leukemia, I lost half of my liver to cancer. My surgeon said that, after such an operation, a man of my age had a thirty per cent chance of living five years. We wept driving home from the hospital. She showed me her poem “Pharaoh” as I lay in bed recovering from surgery:
I woke in the night to see your
diminished bulk lying beside me—
you on your back, like a sarcophagus
as your feet held up the covers. . . .
The things you might need in the next
life surrounded you—your comb and glasses,
water, a book and a pen.
“Is it all right?” Jane said, bending anxiously over me in the bedroom’s half-light. Jane had the habit of repeating a difficult sentence with a heavier emphasis. She said again, “Is it all right?” “It’s a wonderful poem,” I said as I finished it. I paused and added that, yes, it was remarkable to read of my own death, I was so used to writing about other people’s. When I was still skinny with chemotherapy, she showed me a draft of “Otherwise” beginning:
I got out of bed
on two strong legs.
It might have been
otherwise. I ate
cereal, sweet
milk, ripe, flawless
peach. It might
have been otherwise.
As she showed me the poem, it ended two stanzas later: “But one day, I know, / it may be otherwise.” I wonder if Jane suspected that I would change a word; frequently, we revised each other. I crossed out “may” and wrote “will.” And so it was, but not as we assumed.
When, twenty-odd years later, the New York composer Herschel Garfein set several of my poems to music for tenor and piano, he mentioned my name as he visited the medical school at Columbia. “Oh, yes,” a doctor-teacher told Garfein. “We use him.” After I published my book of poems about Jane’s death, many medical schools used me. Sometimes they invited me to read to their students and to answer questions. Twice, the University of Utah flew me from New Hampshire to Salt Lake City to read my poems at the School of Medicine. I told student doctors about our oncologist, Kris Doney, in Seattle, where Jane had her bone marrow transplant. Dr. Doney adhered to Jane’s suffering and to my own as husband and lover. After the successful transplant and our return to New Hampshire, when Jane’s leukemia outwitted her new marrow, Dr. Doney flew cross-country for Jane’s funeral.
Stories of dying and death used to reside outside medical discourse. Death was medical failure, and doctors concentrated on the not yet dead. Then, in the second half of the twentieth century, attention turned to the only event common to everyone. In 1967, in England, the doctor Cicely Saunders founded St. Christopher’s Hospice, not to prolong life but to comfort the dying. Death and grief were subject to intimate analysis in Elizabeth Kubler-Ross’s “On Death and Dying.” Gradually, we have equipped ourselves to think and talk about the dread of terminal suffering. Palliative care has become a medical profession, and dying the subject of lyric and narrative attention. Columbia offers a master’s degree in narrative medicine, directed, appropriately, by Dr. Rita Charon. A doctor at the Yale School of Medicine, Anna Reisman, quoted Jane’s last poem, “The Sick Wife,” on NPR, saying that doctors still “don’t really understand what patients are going through.” Ira Byock wrote “Dying Well.” Atul Gawande’s “Being Mortal” was a bestseller for a year. Every season adds to the literature of dying. Necropoetics includes necromemoir. The young neurosurgeon Paul Kalanithi wrote “When Breath Becomes Air” as he was dying of cancer at thirty-six. Smitten with multiple tumors, he continued to operate on patients. While dying, he made his suffering into a devastating memoir. Last year, in the Journal of the American Medical Association, Dr. Jed Myers, a psychiatrist who lives and works in Seattle, wrote “Poetry’s Company” after he watched his father die over six months of glioblastoma. He quotes from my poems about Jane’s death, then from my friend Christian Wiman, afflicted for decades with his own multiple cancers. Myers ends by addressing the medical profession. “I commend to you, fellow physician, the pragmatically useless treatment called poetry, whereby we might leave our patients less alone when our medicine leaves us all alone.”
[B]efore she became my student, Jane had lived a quiet, rural life, just outside the bustle of Ann Arbor. Her parents were musicians, and she grew up in a house full of books. In junior high, she started writing poems and keeping a journal. She enrolled in the University of Michigan, flunked biology, dropped out, took a job, returned to major in French, studied to be a teacher, switched to English, and took my lecture course in Yeats and Joyce. The following year, she applied to take my poetry workshop, and most of the poems she submitted were slight and fantastic, a habit of the moment that Robert Bly called “light verse surrealism.” Yet one of her poems was darker and stronger. She wrote of trying to capture the attention of her sick grandmother, approaching the hospital bed “like the young nurse with the needle.” The image brought her into my class and altered our lives forever.
In the first three years of our marriage, when we stayed in Ann Arbor, she worked on poems mostly when I flew out of town to do poetry readings. When I was at home my presence appeared to inhibit her. In New Hampshire, for the first time, she worked on poems every day. Here she had no job, no local past nor friends. We had each other, we had our house, we had our landscape, we had my cousins in the small white clapboard church. Every day was devoted to each other or to making poems. She wrote tentatively about inhabiting my place, my history. She saw, or imagined she saw, my ancestors haunting our kitchen. She floated in space like an astronaut detached from the mother ship—or was she attached? She found in the shed a woman’s long gray hair.
A poet from Ann Arbor had moved to Boston, a woman Jane’s age who belonged to the Alice James Poetry Cooperative. Joyce Peseroff recruited Jane, and the Cooperative published her first book, “From Room to Room,” in 1978—the beginning of her career in poetry. Jane and Joyce started a poetry magazine, Green House, addressing their generation of young poets. It was eight years before Jane did another book, the second of the four, but as she published new poems in magazines she came to national attention. I remember when the New Yorker bought its first poem by Jane, “Thinking of Madame Bovary.”
The year when Jane published her first book, I brought out my seventh—that’s what she had to put up with. “Kicking the Leaves” was a breakthrough for me, deriving its force from the ecstasy of marrying Jane and the change from university teaching to life in New Hampshire. My bland first collection, in 1955, had been overpraised. When the second book followed—and the third and the fourth and the fifth and the sixth—no one paid much attention. (Just before “Kicking,” I published a prose reminiscence of older poets. Friendly reviewers found it ironic that the author of “Remembering Poets” had once been a promising poet.) “Kicking the Leaves” was reprinted many times, selling in the end ten times as many copies as my first six titles together. With my marriage to Jane and my return to old sources, I had found myself as a poet.
Meanwhile, Jane’s reputation bloomed, poem after poem and book after book. Three or four times a year she workshopped with Peseroff and Alice Mattison, who published short stories in the New Yorker, and would return from the three-woman workshop triumphant. I watched her excitement and progress with joy and envy.
For decades, she and I had written what could be described as the same sort of poem. It was free verse—mostly short poems in lines of largely similar length, delicate rhythms with forceful enjambments and an assonance of diphthongs. My earliest poems, long before Jane and I knew each other, were rhymed and metrical. Ten years after Jane’s death, out of love for Thomas Hardy and the seventeenth century, I wrote metrical poems again, many of them about Jane. But in the long middle of my life I improvised, like Jane, a sensuous sound without meter. Our work had been different enough—people knew us apart—but we belonged together to a stylistic consensus. Then, as Jane moved from glory to glory, the language of my poems began to diverge from hers. In one lengthy collection, my lines became more ironic and more ingenious in structure. A subsequent, still weaker book collected brief plain poems of anecdotal reminiscence. It appeared just after Jane died, and a compassionate reviewer attributed its failure to my anguish. Over the years I have come to understand how or why my poems altered and deteriorated. Working beside her, I felt overwhelmed as I read “Let Evening Come” and “Briefly It Enters.” I admired the embodiment of her struggle with depression in “Having It Out with Melancholy.” I remember when she handed me “Twilight: After Haying,” one summer after a neighboring farmer finished cutting our fields:
Yes, long shadows go out
from the bales; and yes, the soul
must part from the body:
what else could it do?
The men sprawl near the baler,
too tired to leave the field.
They talk and smoke,
and the tips of their cigarettes
blaze like small roses
in the night air. (It arrived
and settled among them
before they were aware.)
The moon comes
to count the bales,
and the dispossessed—
Whip-poor-will, Whip-poor-will
—sings from the dusty stubble.
These things happen . . . the soul’s bliss
and suffering are bound together
like the grasses. . . .
The last, sweet exhalations
of timothy and vetch
go out with the song of the bird;
the ravaged field
grows wet with dew.
Such sensuous beauty. As the dew falls the soul eases into bodily receptiveness. These devastating enactments of Jane’s art became daily events. The emotional abundance of her language climbed to the summit of literary achievement, the pupil exceeding her teacher, and I made my poems as unlike Jane’s as I could manage.
[W]hen Jane was put to bed in Dartmouth-Hitchcock, an hour north of our house, I rented a motel room next door and spent every day with her. I took notes in brief lines of verse—observations, anecdotes, humors, terrors. I found and used a few of these lines later, when I assembled my poems of her death. Only six months into Jane’s leukemia, I had drafted the poem “Without” in the present tense. She had been diagnosed in January. In the New Hampshire Hospital, as we waited for a stranger’s bone-marrow match and a flight to Seattle in late August, I saw the trees begin to turn yellow from the window. I had not noticed the melt of March nor the green leaves when they arrived in April. We inhabited not the natural world but the landscape of leukemia. I read a draft of “Without” to Jane. From her bed, Jane said, “You’ve got it, you’ve got it!” A year later, I put the poem into the past tense, and eventually it became the title of my book of Jane’s death.
In the weeks after her funeral, I drove four times a day to her grave. I read novels only if they exercised rage and misery—“No Country for Old Men,” not “The Ambassadors.” I took pleasure only in disaster: Oklahoma City, an airplane crash in New York with everyone killed. My days were misery, except for an hour in the morning, when I revised the wailing and whining I had drafted beside her hospital bed. Today I realize that these death poems had already begun to bring my language back to life. One morning I looked out of the window at her garden. Her peonies, basketball-sized, stood tall and still unopened late in May, with weeds starting from the black earth around them. I began the poem that, by autumn, became “Weeds and Peonies.”
Your peonies burst out, white as snow squalls,
with the red flecks at their shaggy centers
in your border of prodigies by the porch.
I carry one magnanimous blossom indoors
and float it in a glass bowl, as you used to do.
Ordinary pleasures, contentment recollected,
blow like snow into the abandoned garden,
overcoming the daisies. Your blue coat
vanishes down Pond Road into imagined snowflakes
with Gus at your side, his great tail swinging,
but you will not reappear, tired and satisfied,
and grief’s repeated particles suffuse the air—
like the dog yipping through the entire night,
or the cat stretching awake, then curling
as if to dream of her mother’s milky nipples.
A raccoon dislodged a geranium from its pot.
Flowers, roots, and dirt lay upended
in the back garden where lilies begin
their daily excursions above stonewalls
in the season of old roses. I pace beside weeds
and snowy peonies, staring at Mount Kearsarge
where you climbed wearing purple hiking boots.
“Hurry back. Be careful, climbing down.”
Your peonies lean their vast heads westward
as if they might topple. Some topple.
It was Jane’s “prodigies”; it was Jane’s “magnanimous” blossoms; it was Jane who saw Gus’s “great tail swinging” and the “repeated particles” of snow. After her death I was able again to assume a diction as potent as Jane’s. I revised and finished “Without” and “The Porcelain Couple” and “The Ship Pounding.” I wrote “Letter With No Address” in our common language, and continued my posthumous one-way correspondence through “Letter After A Year.” After “Without,” I continued to write about Jane in “The Painted Bed,” sometimes returning to metrical forms. In the months and years after her death, Jane’s voice and mine rose as one, spiralling together the images and diphthongs of the dead who were once the living, our necropoetics of grief and love in the singular absence of flesh.
Complete Article HERE!
Most Families Wait Too Long to Utilize Hospice Care
Researchers say elderly people are in hospice care for an average of only 12 days. Why aren’t they admitted sooner?
by Gigen Mammoser
[H]ospice centers provide valuable end-of-life care for the elderly.
So, why aren’t more people using these centers?
The Medicare hospice benefit (MHB) was established in 1982 in order to give recipients access to high-quality care near the end of their lives.
But, new research in the Journal of the American Geriatrics Society states that those who utilize the service often do so too late.
The study included 562 individuals, all aged 70 and older with an average age of nearly 87 years.
Of these older adults, only 43 percent of them were admitted to hospice during their last year of life.
While hospice is available to individuals with six months or less to live, researchers found that for half of the study participants their duration of hospice care was less than 13 days.
The authors say underutilization of hospice care can create a burden for healthcare workers, and result in patient suffering.
Why don’t people utilize hospice?
The reason why hospice care isn’t used more frequently is complex.
According to statistics from 2000, only 23 percent of Medicare beneficiaries who died were in hospice care at the time.
The MHB was initially offered for those with end-stage cancer. However, more and people have begun seeking hospice care for noncancer-related ailments.
The problem is that other issues, such as frailty and dementia, may be harder to discern when determining an individual’s eligibility for hospice care.
“It is well documented that the prognostication [predictability] for those patients with a noncancer diagnosis is more difficult and is a complicating factor for physicians and others who refer patients to hospice care,” said John Mastrojohn, executive vice president and chief operating officer of the National Hospice and Palliative Care Organization (NHPCO).
Lead study author, Dr. Thomas Gill, a professor of medicine at Yale University, agreed.
“Cancer tends to have the most predictable course,” he told Healthline, “meaning it is generally easier to predict when someone with cancer is in the last six months of life than someone with another terminal condition.”
“The challenge is even greater for older persons since many die from a combination of different conditions and/or debility, none of which may meet criteria for hospice,” Gill added.
That gets even more problematic when you look further at the results of Gill’s research:
The most common conditions leading to death were frailty and organ failure, not cancer. However, hospice acceptance rates for frailty were the lowest, and for cancer the highest.
Waiting too long
Not only is care jeopardized by condition, but by duration of stay as well.
The median of 12.5 days spent in hospice indicates that even when individuals do utilize the MHB, it is at the last possible moment.
“A large proportion were admitted shortly before they died, which makes it difficult for hospice to optimize its benefits,” said Gill.
Hospice care offers a unique opportunity to individuals who are near death in that it is not intended to cure them.
It is strictly palliative, meaning it is meant to provide comfort and quality of life.
Benefits of hospice care, Mastrojohn told Healthline, include expert pain management, spiritual support, as well as social and physical activities, tailored to the individual.
Hospice also provides service to families through bereavement support to help them deal with the loss of a loved one.
“Hospice is a benefit delivered by clinicians who are expert in the care of those with serious, advanced illness,” said Mastrojohn. “It is my hope individuals would be more open to receiving hospice services so they can maximize the many benefits they need and deserve.”
Changing how hospice is viewed
While this new research helps to highlight the underutilization of hospice care, it does not provide crystal clear answers why.
However, the authors hope that their work will lead to better strategies for addressing those who need hospice care, and getting them enrolled sooner in a program, rather than waiting until the last moment.
But hospice care also represents a difficult dilemma for families, which may help explain why duration of stay is so low.
For some, putting a loved one in hospice care can sometimes be seen as a sign of defeat.
“Some patients and/or families might interpret hospice as ‘giving up,’ but this is clearly not the case,” said Gill.
Complete Article HERE!
How To Take Charge Of Your End-Of-Life Care—And Why You Should Care About It Right Now
Simple tips for navigating the world of advance directives and health care proxies.
To get started, it’s a good idea for every adult over 18 to create an advance directive—a set of legal documents that typically has two components: a health care power of attorney, in which you appoint someone called a health care proxy to make decisions for you if you’re unable to, and a living will, in which you lay out your end-of-life treatment preferences.
You might specify, for example, that you consent to antibiotics and pain medications but not CPR, which can cause internal injuries. You can also state that you prefer to die at home. In fact, according to the New England Journal of Medicine, people with advance directives are more likely to avoid dying in a hospital.
Assembling the documents is easy. You fill out paperwork available online through your state’s Department of Aging, and these documents become legally valid after you sign them in front of witnesses. The number of witnesses required varies by state, but you don’t need a lawyer, according to the National Hospice and Palliative Care Organization. After signing the paperwork, give copies to your health care proxy and your doctor. You can change your plan at any time.
Despite the ease of creating the documents, most Americans haven’t done it. In the most thorough study on the topic to date, University of Pennsylvania researchers examined data on more than 795,000 people from 150 studies and found that advance directives were only slightly more prevalent among people with chronic illnesses (38.2%) than healthy adults (32.7%).
“We need to address common barriers to filling out these important documents, particularly among chronically ill patients,” says study co-author Katherine Courtright, MD, an instructor of medicine at Penn. These obstacles include a reluctance to talk to family members about end-of-life preferences—one Yale study found that 40% of people ages 55 and older said they hadn’t broached the topic with relatives—and concerns about the potential time and expense involved.
“Dying in America today can be a protracted, painful, and traumatic experience,” says Sara Moorman, PhD, an associate professor of sociology at Boston College. “And that’s unfortunate, because we possess the know-how to make most deaths comfortable and even meaningful.”
Here are two resources to get you started:
The Conversation Project
Studies have shown that many people don’t talk to family members about what medical interventions they would or wouldn’t want at the end of life. The Conversation Project, however, can help you do just that. The site provides starter kits for family discussions and for appointing a health care proxy.
Prepare for Your Care
Prepareforyourcare.org provides advance directive forms and takes you through filling them out and sharing them with family and medical providers.
Complete Article HERE!
Death, too, is part of life cycle
By HOLLY WOLTZ
[I] live, breathe and eat being a veterinarian. I see a pet on a leash, and I check its gait. I see a grey whiskered dog and think of senior issues. I overhear a conversation about a pet’s illness, and I want to add my two cents.
Work is hard. Work is fun, and every day brings challenges. However, I had no idea when I signed up for this job, the sheer number of euthanasias and sadness I would face.
All pets die, and we know this when we adopt them into our lives. We are angels of death to so many, and this is a very, very important part of our lives.
The veterinary profession is unique when it comes to being comfortable with death. Like many aspiring veterinarians, I thought euthanasia would be the hardest part of my job, but it isn’t – not by a long shot.
MDs don’t get it. In the human world, euthanasia is a grave sin even when someone is suffering from a terminal illness.
“Futile care” occurs when a physician cracks the chest of an elderly patient in multi-organ failure who has just arrested, or the oncologist details a complicated journey for a deadly metastatic cancer.
The older you get, the more likely you are to die in a hospital. According to the Centers of Disease Control, 73 percent of people over the age of 65 die as inpatients.
It sounds like a horrible way to go. I hope that statistic changes as more states enact the Death with Dignity Act, and I add more years.
Almost every day I counsel clients as to “When is the right time to let go?” I have changed my criteria for euthanasia over the years and now answer that question with “Consider 6 things that your pet loves to do. If they are no longer able to do at least half of them, then it is time to let go.” This helps, but it is still far from simple.
Every situation and every family is different. I think relief from suffering is a moral obligation, and that it is better to end life too soon than too late. Euthanasia is truly a gift of love.
Never was this more apparent than last week. You might recognize this family because I’ve already written about Buddy.
I shared Buddy, a magnificent Golden Retriever, with Dr. Sybil Davis (a certified rehabilitation specialist).
When I first referred him to her 4 years ago, he could barely walk from a myriad of problems. In 6 months, he was walking and feeling great again.
His family simply refused to give up on him. He’s been a “frequent flyer” patient for both of us over the years.
This visit was different, and when I stepped into the examination room, I knew he was in trouble. He could barely stand and his breathing was labored.
Although Buddy lived in a family of three, he was really the son’s dog. They grew up together, and Alec brought Buddy in for visits. I always thought of Norman Rockwell’s paintings of boys and children whenever I saw them!
After diagnostics and quiet conversation, it was clearly time to let go, but we would not be rushed in making this decision. End of life should be kind – to the owner, as well as the animal.
I tried to walk the emotional landscape that accompanies the decision to euthanize. Do we refer, try hospice care, sleep on this decision for a day or two and reconsider? Could we give Buddy more days of good living? And, if we euthanize, what do we do afterward?
The whole family was present with Buddy, and the parents deferred the decision to Alec. He knew. I could see it in his eyes, but it was too hard to verbalize.
In his heart, he knew that Buddy had finally worn out. What a wonderful young man to put his dog first, and I know his parents were proud of him.
Buddy didn’t know what was happening. All he knew was a sense of tranquility from sedation, a quiet comfortable room and his family surrounding him. He died with grace and dignity, quickly with no pain. It was a gift from his best friend.
I am sometimes overwhelmed by these last moments, but I am also thankful that I can be a part of them. Without great love, there cannot be grief.
Thank you, Alec, for making the right decision, and thank you, Buddy, for the memories.
Complete Article HERE!
Helping create a better death is a new doula concept
By Gary Rotstein
[O]n a sunny Sunday afternoon marked by perfect September weather, a gathering of nine women and one man wasn’t focused on talk about nature, recreation, hobbies or other aspects of enjoying life.
This group instead met for two hours in a downtown Greensburg office building to discuss the dying process and how to make it better.
The attendees at a free community training session about serving as end-of-life “doulas” heard Promise Hospice President Elizabeth Aungier, who hosted the session, talk about the goal of “a better death” for both terminally ill patients and their families. The former nursing home administrator has run her Greensburg hospice since 2010, but in navigating her own father’s death in 2015 she needed to lean on a friend for help.
She realized an additional layer supplementing a hospice team would be useful for families during a daunting, emotional process that is new to many of them.
“After my dad passed away I figured, if I needed extra support and I’m supposed to be an end-of-life expert, what about the individual that doesn’t have that knowledge? How can we help fill the gap between what the medical profession provides and maybe what a family needs?”
Ms. Aungier became intrigued by what she heard of end-of-life doulas and went through training herself last year in New York City from Doulagivers Inc. There she learned communications and technical skills related to helping people with their dying wishes and the closure they sought in relationships with others, as well as more procedural issues such as advance directive preparations and the type of funeral or memorial services they wanted.
Doulas are taught to sit, talk with and — especially — listen to terminally ill people in a non-judgmental way. If it goes right, they learn about their lives, build a rapport and help them face whatever fears they may have about the future. They can do so without the baggage of family members or the requirements of hospice staff who may be on a busy schedule to provide personal care and pain relief before moving on to the next client.
“The doula may spend extensive time helping an individual do a life review or legacy project or tangible account of history we can give to people they leave behind,” Ms. Aungier added, while emphasizing they are to leave medical issues to professionals such as a hospice nurse.
The end-of-life doula concept is new in southwestern Pennsylvania, she said, with New York and California among the still relatively rare places in the country where organizations like Doulagivers provide detailed training for a fee. Doulas are more commonly associated with births; while employed in only a small minority of those, they are nonetheless accepted as providing non-medical emotional and educational support for new mothers.
In either case — for births or deaths — doulas generally lack government certification or regulation and are paid by private resources rather than Medicare, Medicaid or other insurance.
Ms. Aungier sought to supplement her hospice business by starting PromiseCare Doulas in June, advertising $50 hourly services to support dying individuals through their final stages, but it has been slow to find clients. Ms. Aungier is undeterred, believing it’s an important and helpful concept. She has had most of her hospice staff trained in it to help them in their regular duties as aides, nurses and social workers.
“We’ve learned how to be more one-on-one now with patients in the dying process, understanding better how to walk them through that,” said Ginny Cabala-Carper, 28, a hospice aide for five years who was among staff in the spring going through weekend-long doula training sessions Ms. Aungier arranged for them.
“This will help us in our personal life, too,” Ms. Cabala-Carper said. “We’re all going to have loved ones die someday, and this helps me see what my parents and grandparents will need.”
Sunday’s session was the first of a series of free, two-hour educational presentations Ms. Aungier said she intends to provide for anyone from the community. They could be for those interested in being hospice volunteers, whether for her operation or others. They could also be for people simply interested in increasing knowledge to help relatives, friends and neighbors.
And others could treat it as the first step to someday hanging a shingle to offer service themselves as an end-of-life doula, though Ms. Aungier cautioned that they shouldn’t expect an immediate flood of calls.
“People don’t really seem to get it yet,” she said, having heard more commonly from people interested in getting help with bereavement after a death.
Arleen Hawk of Greensburg, a retired hospice social worker who was among the group Sunday, said it sounded to her like doulas could do more for families than the more limited aspects of what she did in her role while working.
“They can take it to the next step and help families feel they’re not missing anything,” she said.
Nisha Bowman, an intensive care unit social worker at UPMC Presbyterian with a pronounced interest in death and dying issues, attended to learn more about the doula concept as someone who may focus her career on end-of-life issues in the future.
“It just make sense,” said Ms. Bowman, 34, of Perry South. “If we have it for births, why not have it for deaths? … To know that there’s people who are trying to help people do death better is very heartening, because there’s still a lot of stigma to it.”
Complete Article HERE!
Why the Irish get death right
We’ve lost our way with death, says Kevin Toolis – but the Irish wake, where the living, the bereaved and the dead remain bound together, shows us the way things could be done

By Kevin Toolis
[I]n the narrow room the old man lay close to death.
Two days before, he had ceased to speak, lapsed into unconsciousness, and the final vigil had begun. The ravages of cancer had eaten into the flesh leaving only a skeletal husk. The heart beat on and the lungs drew breath but it was impossible to tell if he remained aware.
In the bare whitewashed room, no bigger than a prison cell, 10 watchers – the mná caointe – the wailing women, were calling out, keening, sharing the last moments of the life, and the death, of this man. My father. Sonny.
“Holy Mary, mother of God, pray for us now, and at the hour of our death.”
In the tight, enclosed space, the sound of this chorus of voices boomed off the walls, the ceiling, louder and louder, reverberating, verse after verse, on and on, cradling Sonny into death.
This death so open, so different from the denial of the Anglo-Saxon world would, too, be Sonny’s last parental lesson.
How to die.
If you have never been to an Irish wake, or only seen the movie version, you probably think a wake is just another Irish piss up, a few pints around the corpse and an open coffin. But you would be wrong.
In the Anglo-Saxon world, death is a whisper. Instinctively we feel we should dim the lights, lower our voices and draw the screens. We want to give the dead, dying and the grieving room. We say we do so because we don’t want to intrude. And that is true but not for these reasons.
We don’t want to intrude because we don’t want to look at the mirror of our own death. We have lost our way with death.
On the Irish island where my family have lived in the same village for the last 200 years, and in much of the rest of Ireland, death still speaks with a louder voice. Along with the weather reports of incoming Atlantic storms, the local Mayo country and western radio station runs a thrice daily deaths announcement enumerating the deaths and the funeral arrangements of the 10 or so daily freshly departed. There is even a phone line, 95c a minute, just so you can check up on those corpses you might have missed.
There should be nothing strange about this. In the absence of war and catastrophe, humans across the planet die at an annual rate of 1%; 200,000 dead people a day, 73m dead people a year. An even spread. It’s happening all around you even as you read this article; the block opposite, the neighbouring street and your local hospital.
If the local radio in London or New York did the same as that Mayo station, the announcer would have to read out the names of 230 dead strangers, three times a day, just to keep up.
Of course, if you live in a city such as London, where 85,000 people die each year, you would never know of these things. Such a very public naming of the dead, an annunciation of our universal mortality, would be an act of revelation in the Anglo-Saxon world. And likely deemed an outrage against “public decency” – which would almost certainly lead to advertising boycotts and protests.
More shocking still then would be the discovery of another country where the dying, like Sonny, the living, the bereaved and the dead still openly share the world and remain bound together in the Irish wake.
And death, in its very ordinariness, is no stranger.
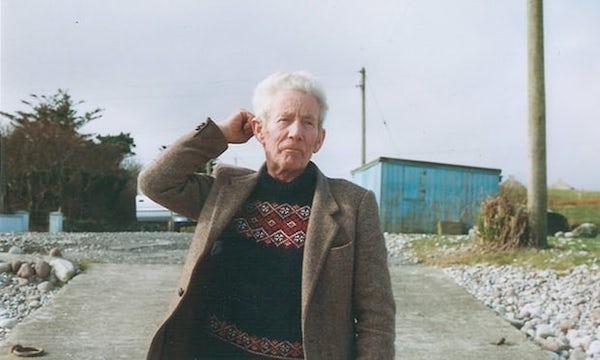
My father, Sonny Toolis, was too a very ordinary man. He was never rich or powerful or important. He never held public office and his name never appeared in the newspapers. The world never paid him much attention and Sonny also knew the world never would. He was born poor in a village on an island, devoid of electricity, mains water and tarred roads, in much the same way the poor have been born in such places for most of human history.
Sonny never got the chance to get much of an education and worked most of his life as a foreman on building sites earning the money to pay for the university education of his seven children.
Sonny was good with his hands though. Useful to have around if things went wrong with the electric, the drains, or you needed the furniture moved. He had his limitations; he did not like strange peppery foods, he wasn’t very comfortable wearing suits, and he was terrible at giving speeches at weddings.
He did have a great singing voice, played the bagpipes and the accordion, and taught his children to sing by what he called the air – by listening along. In the 1960s, he bought a 35mm German camera, took pictures, and ran the prints off in his own darkroom. He even shot film on Super 8. But it was never more than a hobby. Like a lot of us, Sonny had some talents he would never fully realise in life.
But Sonny really did have one advantage over most of us. He knew how to die. And he knew how to do that because his island mothers and fathers, and all the generations before, had shared their deaths in the Irish wake and showed him how to die too.
His dying, his wake, his willing sharing of his own death, would too be his last parental lesson to his children and his community. A gift.
The wake is among the oldest rites of humanity first cited in the great Homeric war poem the Iliad and commonly practised across Europe until the last 200 years. The final verses of the Iliad, the display of the Trojan prince Hector’s corpse, the wailing women, the feasting and the funeral games, are devoted to his wake. And such rituals would be easily recognisable to any wake-goer on the island today.
For our ancestors, a wake, with its weight of obligations between the living and the bodies of the dead, and the dead and living, was a pathway to restore natural order to the world, heal our mortal wound, and communally overcome the death of any one individual. An act, in our current, thin psychological jargon, of closure.
Through urbanisation, industrialisation and the medicalisation of death, the wake died away in most of the western world and death itself came to be silenced by what might be called the Western Death Machine. But out in the west, among the Celts, this ancient form of death sharing lives on.
When he was 70, my father was diagnosed with pancreatic cancer – still among the most fatal cancers among western men. Sonny never flinched. He did not want to die but when he knew he had no choice, he never wasted the time he had left. He wasn’t angry or embittered but something wiser – he accepted his death. He got on with his dying the same way as he had got on living, day by day, pressing forward, husbanding his energy.
Sonny’s time had come but neither he nor his community denied his impending death. Unlike the shunning of the Anglo-Saxon world, his house filled with visitors who came to see him because he was dying.
Dying is an exhausting, self-centring act. Sonny, always a powerful physically imposing man, rapidly shed powers like a snake shedding skin. His world shrank to two rooms and Sonny knew he would never see the end of that fateful summer.
Sonny’s fatherhood was ending and my own beginning. Our last words together on his deathbed were very ordinary, bland. “I’ll let you go, son,” he said as I left to return to the city. When I returned, he had lapsed into a coma and could no longer speak.
But our parting was fitting. There was no more mystery to share. No revelation to be uncovered. Our identities as father and son had already been written out in the deeds of our life together; Sonny changing my nappy, not losing his temper in my teenage contrariness, encouraging me in my education and the summers we shared on building sites when I worked alongside him while still a student. And in all the countless ways he showed me in his craft how to be a man and father myself.
Sonny died just before dawn on the longest day of the year at home in the village of ancestors. No one called for help, or the “authorities”. He was already home with us. His body was washed and prepared for his coffin by his daughter and sister-in-law. He was laid out in his own front sitting room in an open coffin as his grandchildren, three, five and nine, played at the coffin’s feet.
His community, his relatives, some strangers even, came in great numbers to pray at his side, feast, talk, gossip about sheep prices or the stock market, and openly mark his death in countless handshakes and “Sorry for your trouble” utterances.
We waked together through the night with Sonny’s corpse to guard the passage out for his departing soul and man the Gate of Chaos against Hades’ invading horde lest the supernatural world sought to invade the living world. Just as the Trojans too before us had watched over Hector’s corpse. A perpetual quorum; dying in each other’s lives and living on in each other’s deaths at every wake ever since.
It was blessing of a kind, an act of grace. We give ourselves, our mortal presence, in such death sharings, or we give nothing at all; all the rest of our powers, wealth, position, status, are useless.
To be truly human is to bear the burden of our own mortality and to strive, in grace, to help others carry theirs; sometimes lightly, sometimes courageously. In communally accepting death into our lives through the Irish wake we are all able to relearn the first and oldest lessons of humanity. How to be brave in irreversible sorrow. How to reach out to the dying, the dead and the bereaved. How to go on living no matter how great the rupture or loss. How to face your own.
And how, like Sonny, to teach your children to face their death too.
Complete Article HERE!
Festival of Death and Dying explores topic Australians ignore
News headlines can feel like a catalogue of death and destruction, but are we really grappling with the reality of human mortality? The answer is no, according to a new festival.
By Eloise Fuss and Lisa Skerrett
The Festival of Death and Dying wants us to stop focusing on our jobs, mortgages, children and relationships for a minute to consider life’s biggest unknown: death.
“We all live in a way as if we’re going to live forever,” said Festival of Death and Dying director Dr Peter Banki.
“To produce a cultural shift we need to do more than just talk about death and dying, I think we need to actively learn more about it, and even experience it in a certain way.”
The festival takes place in Melbourne this weekend after a successful debut in Sydney last year, with plans to also expand to Adelaide and Berlin.
Using art installations and immersive workshops, it hopes to provoke contemplation about how societies mark death and come to terms with the inevitable loss of friends and family.
“[Death] is probably the most difficult thing that any of us will ever have to do, and it’s probably the most important thing one can do for someone else — witnessing someone dying, accompanying them, and taking responsibility for their legacy and their memory,” Dr Banki said.
“You can’t experience death as such, so you need art — it helps us bear witness to it, even if it doesn’t save us from it.”
Mainstream Australia distanced from death
Before modern medical breakthroughs like vaccines and penicillin, it was more common to die at home, meaning most people had firsthand experience of human death.
Traditional funeral rites were also largely a family affair — a far cry from today’s funeral industry, which Dr Banki thinks has “commodified” the personal experience and expression of grief.
“We don’t see death, it’s hidden from us,” he said.
“You have a funeral and you might have a get together afterwards but that’s about it, there’s nothing within the culture that’s there or any type of ritual or ceremonial way to mourn our dead.”
One project helping people create ritual around death is a fashion designer making garments for the grave.
Pia Interlandi combines skills in fashion and funeral celebrancy, working with individuals and families to create bio-degradable clothing to be buried in.
“It neither denies nor flirts with death, but presents it in a way that invites observers to view it as natural, undeniable, inevitable and at times, beautiful,” said Ms Interlandi.
Rituals and mourning

There is another older way of thinking about death close to home too: the complex mourning rituals of Australia’s Indigenous cultures.
Artist Maree Clarke builds an understanding of grief from an Indigenous cultural perspective, by guiding people through the experience of wearing Kopi mourning caps, or widow’s caps.
“In different areas some women would cut off their hair, weave a net of emu sinews, place it on their head and then plaster their head with gypsum, a very heavy river clay.
“They represented the weight of your grief, so the heavier it was, the bigger connection to the person that had passed.”
Dr Banki said mainstream Australia, which had “completely missed out on these ways of mourning”, had a lot to learn from Aboriginal cultures about dealing with death — and that getting “hands-on” helped in the process.
“There are other people in Australia also working to promote people to learn and have conversations about death and dying, but it’s always within the realm of speech and lectures and talks,” he said.
“We think deep learning happens when people feel something, when people experience something, and for that you have to get them to try on a garment or have to get them to try on a hat, or go into a coffin.”

Complete Article HERE!




