Now I measure time in distinct chunks, focusing on events – a holiday or a party. Although it has been an intense few months, I’ve tried not to dwell on it
By Max Edwards

Five months ago, I was diagnosed with terminal cancer aged 16. It was rather as I’d pictured GCSE results day to be: a lot of stress waiting for potentially awful results, although, as it happened, GCSE results day was a pleasant surprise. But, like many whose grades came as a disappointment, I got over it soon enough. I think it’s surprisingly easy to adapt to this kind of news. After all, while I’m not going to deny its personal significance, it doesn’t really change anything important.
In the past, I have imagined terminal illness as the short and depressing period before a person’s premature death, but it somehow doesn’t feel nearly as dramatic or upsetting. I don’t feel as though normal life has ceased, or that my perception of it has changed drastically. In fact, if it weren’t for my loss of mobility following an operation, my life would have probably settled back to normal long before now. The assumed tide of unimaginable suffering that rests hand in hand with these kinds of situations is rather less dramatic in reality.
Being told you are going to die is a shock, but I was largely over it in a week, and as for breaking the news to friends and family around me, the guesswork on my part of trying to assess the other person’s emotional fragility, their guesswork at trying to assess mine, and the background danger – perhaps felt by both of us – that your partner in conversation is about to break down in tears, made the experience not so much sad as really quite awkward.
This isn’t to say that it hasn’t been an intense few months, but I can’t say that this experience has truly changed me as a person. People have told me how well I’m coping and how they couldn’t have done the same in this situation, as though I’ve faced an unimaginably horrendous set of circumstances and managed to do the impossible (remain positive), but I don’t see it that way.
While I understand why it may feel like that to those looking in from the outside, dying of cancer, in my experience, has been a succession of hospital visits, a lot of pills, and one or two pieces of bad news. But after that, there is an inevitable return to the way you were previously living. Pretty soon I came to realise that it doesn’t make any difference if you’ll be dead in 10 years or two months; you still get up, have a shower and make a cup of tea.
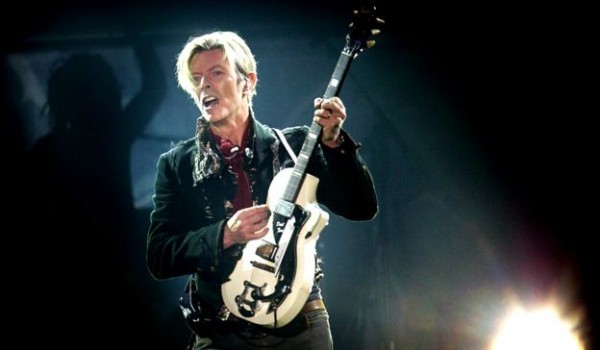
OK, so there are drawbacks – in my case, largely a lack of movement. After the operation on my spine, I was all but paralysed in my dominant hand, movement was compromised in the other and I could barely move my legs, all of which meant I could no longer write, walk, or play the guitar and clarinet. These limitations didn’t seem to matter when I was still in hospital, but as I left bed eight, ward 27 and returned home, I was confronted by all I could no longer do. At first, when the seriousness of my illness was still a new and shocking discovery, the issue of not being able to walk to the toilet seemed dwarfed by this drama, and it was only later that these kinds of problems started to irk me.
Nonetheless, I’ve found that these problems start to sort themselves after a while. For example, I was at first stretchered around the hospital. As my mobility improved, I spent more time in a wheelchair, which at least gave me the luxury of seeing where I was going. Currently, I walk with a stick, which of course resolves many difficulties, and I can now eat at a restaurant without having to sit half a mile from the table because the wheelchair won’t fit underneath.
Where there hasn’t been a significant improvement, such as in my right hand, I’ve tried to make up for the problem. Unable to play any instruments that require two hands, I’ve begun learning the blues harmonica (which only requires one – at least it does the way I play it) and, while practising writing left-handed, I now type on a touchscreen phone, this being how I continued to write my weekly blog and my recently published book. In addition to this, I’ve continued to write songs and music by composing on the computer. I suppose I can at least be glad to live in an era when technology makes this possible.
Religion has featured a lot in discussions since the diagnosis. I am told that many people are praying for me and I have prayed myself, though I never thought it would make a difference (I only did it on the off chance that something positive might happen – what’s to lose?). I don’t believe in God; I didn’t before my diagnosis and I don’t now. I can see how some in my position may want to turn to religion as a comfort, and I can also see how many may become disillusioned or even angry with the God they thought they believed in. But I have done neither. Most of my frustration has fallen on nurses and medical staff for the most trivial of reasons.

As for comfort, I don’t feel I need comforting. The initial shock wears off very quickly, and after that, life seems to become quite ordinary. The satisfaction of daily routines is enough in the way of comfort.
One thing I have started to do is measure time in distinct chunks. Ordinarily, I would allow days to blur into weeks, weeks into months and months into years. After my operation, however, I’ve found myself focusing on certain events. A holiday, for example, or a day trip, or a party. Perhaps my perception of time has changed, or maybe it comes from a lack of ways to fill the day, although that’s becoming less of a problem now that I’m more mobile and have been able to get more done, such as schoolwork (AS-level history), which I’ve just restarted.
In terms of where I want to be, my main hopes for the future are life-expectancy-related. This is one thing that still gets to me: I’ve more or less made peace with the idea of death, but it’s the question of when that is still a daunting thought. The (almost) inevitable growth of my cancer means it is likely to come some time soon, but I still don’t know when exactly, and I’m not sure I want to.
Regular MRI scans will probably give me an indication of how bad the situation is as and when that becomes the case, which means there is more bad news in store for me. I considered not having any further scans, but then I’m sure I’d panic with every slight pain or possible symptom of tumour growth, and given that I already interpret a headache as, “OH MY GOD, IT’S SPREAD TO THE BRAIN AND I’LL BE DEAD WITHIN A WEEK!”, I’d rather not venture any further down this route.
I am sure the expectation of death is worse than death itself. True, they say death is the worst single thing that can happen to you, and given that I can’t trick myself into believing there is an afterlife, I imagine it leads only to an empty void, but I’ve found ways to accept such an idea. First, I look on my life, which I believe has been a modest success, and remember that it could not have occurred in any other way. The only possible way I could have had my unique set of experiences is by living my life as it is, and that means dying when I die. Even if I’m wrong, and there has been more unhappiness than I care to remember (rendering my life “unsuccessful”), death – the absence of pain or pleasure – should then logically be seen as an improvement.
I also remind myself that the experience of dying is not unique to me. Whether it happens aged 16 or 95, experiencing the end of everything you know is the same process – it’s just that I and those around me are forced to come to terms with this fact prematurely.
Finally, I feel it has helped to process the whole issue selflessly. Some people might find it helpful to know that they are loved, that people care about them and that they won’t be forgotten when they die. I can understand this and I see how it’s comforting, but I also find it consoling to take the opposing view: stop dwelling on personal suffering and carry on as before.
This approach seems to help deflate the hype that terminal diagnoses carry. Pity, grief and sympathy are all natural emotions, and they certainly have their place, but I’ve found the message of “Stop whining and get on with it” far more effective. Stoicism, I feel, is more effective than grief: a simple reality-check helps to set my perspectives in place.
It helps to remind myself that even if I’m dying, it’s not all about me. At the end of the day I’m one in seven billion, a number that – like my cancer – will continue to grow and multiply over the coming months and years. While my life may be all I know, I’m nothing more than a dot on this planet. When you take into account the dozens of people I know, the billions I don’t, the thousands of miles that separate us, and the ever running river of time on which we all finitely float, you may come to the inevitable and strangely comforting realisation that we are all going to die: me, you and everyone else. Get over it.
Complete Article HERE!