By Jane Peterson
[M]y mother’s last words were “It’s not working.” She slurred them before she fell into a deep sleep. Just prior to that, after ingesting medication mixed with applesauce, she had placed a plastic bag over her head and secured it. According to her meticulous research, this would hasten her passing.
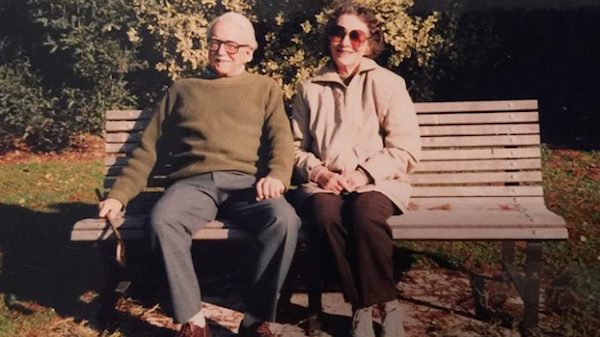
Her death had been planned for months, if not years. Both my parents were members of The Voluntary Euthanasia Society in New Zealand, where they had retired from England to be close to my eldest sister and her children. Even though I had married an American and moved to rural Colorado, I was fortunate enough to be able to visit them every year and stay maybe two or three months.
Contemplating end of life
Our end-of-life discussions had been ongoing for many years, and both my parents were determined to die with dignity at a time of their choosing and before any needless and expensive medical procedures. Their wish was to pass away at home, as peacefully and as inexpensively as possible. As a family we agreed, with no hesitation. Now I pray that my sister and I can end our lives, legally, with the help of an enlightened physician, when quality of life is no longer an option.
My parents generally were in good health until my mother was diagnosed with rheumatoid arthritis at 82. This horrible disease was rampant on her side of the family—her beloved sister became ill in her 20s. She suffered mightily, without today’s wonder drugs that can alleviate some of the unpleasant symptoms, and died in her early 50s.
My mother had obtained a supply of Seconal from her doctor in London and had guarded her “stash,” with a mind to her eventual death. Despite the capsules being several years old, Mother did valuable research, including obtaining a prescription for anti-nausea pills, as well as taking six 10-mg Valium, with a glass of wine, before ingesting the lethal dose of Seconal. She had written separate goodbye notes to my father and to my sister and me. This was necessary to exonerate her family members in aiding and abetting her demise.
The final weeks of her life were filled with joy and laughter, and the planning took on a military aspect that my father, a lieutenant colonel in India during World War II, reluctantly took part in. I can honestly say that we had never laughed so much, despite the looming event that was ever present.
My mother’s pain was becoming increasingly unbearable and even sitting up in bed caused her appalling agony. The family doctor (they still made house calls in New Zealand) had given her Prednisone and Methotrexate. However, throughout her life, my mother had been unable to tolerate strong medications and she was terrified that the Prednisone was making her blind. The Methotrexate, on the other hand, messed with her mind. To our horror, a few weeks before, we found her lying outside in the driveway, in the pouring rain at 3 a.m., crying softly for help.
Goodness knows how long she had been there, and thank God I needed to use the bathroom in the middle of the night. When I checked her room and she was not in bed, I alerted my father. She was taken by ambulance to the nearest hospital and she remained there to be stabilized for a week.
Dying with dignity
Trying to keep on an even keel the morning of her death, I heard her speaking with my father who was asking her (again) if this was what she really wanted. I was cleaning up in the kitchen, and I am not ashamed to say that I lost it. I was privileged to have exceptional doctors in America and was prescribed suitable medication to help me through difficult times. This was definitely one of those occasions and I make apologies to no one.
Darling, darling Mother! So adamant that she could leave my sister and me as much money as she was able. She needed relief from her torture and, thanks to a long relationship with her family doctor in England, she was able to obtain it, in her own bed, surrounded by loving family. My sister and I monitored her pulse. It became weaker and weaker, until it was apparent that she had passed. The whole process took less than one hour.
It remains the most spiritual experience of my life, and I was similarly affected when my father died at home, just over a year later. Desolate after my mother’s death, he lost the will to live and had even asked my sister about getting a gun.
He passed away a week after being placed in a morphine-induced coma by his physician, so there was no verbal contact in his last days. Although he did not have to resort to my mother’s method, he succumbed to an illness that had no name since any diagnosis, advice or procedures that might have prolonged his life were adamantly refused. I suspect it was pancreatic cancer that prevailed.
He died around 11 a.m. on September 1, 1996, with me by his side, holding his hand and professing my love.
The right to make our own choices
As before, with my mother’s death, the funeral director who came to the house was incredibly disappointed when my sister and I firmly rejected his top of the line caskets. My parents always said that they wished to be cremated in matchboxes, a standing joke in our family for many years.
I give thanks every day for my parents’ decisions. My friends are coping with family members suffering from Alzheimer’s, dementia and worse. Their loved ones die in hospitals and nursing homes, lives needlessly prolonged. It results in loss of dignity, immeasurable suffering and devastating financial consequences.
I am so encouraged that more states have passed laws enabling physician-assisted dying (end-of-life options). To those of a similar persuasion, I urge you to become members of Compassion and Choices, based in Denver and available at 800-247-7421 or www.CompassionAndChoices.org. This progressive organization endorses Death With Dignity, and was instrumental in the Colorado voters passing the End-of-Life Options Act, now legalizing medical aid in dying. They continue their efforts in all states.
We should all be so fortunate to have the legal right to pass as we wish, and I say no state or federal agencies have any right to dictate how we make personal medical decisions.
Complete Article ↪HERE↩!