By Amy Berman
To: Centers for Medicare & Medicaid Services:
News reports say you will soon make a final decision about paying doctors and other providers who talk to their patients about end-of-life planning, I have a fatal form of breast cancer, and I’d like to tell you how such conversations have allowed me to survive, and live well, in the five years since my diagnosis.
I am a nurse, a nationally recognized expert in care of the aged and senior program officer at the John A. Hartford Foundation, which is devoted to improving the care of older people in the United States. Yet my perspective is not simply professional. For, you see, I live with Stage 4 (end-stage) inflammatory breast cancer. And while this metastatic cancer will one day kill me, the advanced-care planning conversations I have had with my health-care team have been lifesaving since my diagnosis.
I use the word “lifesaving” advisedly because that is what these conversations are truly about. When done well, they can shape care in ways that give people with serious illness a chance at getting the best life possible.
This kind of conversation initially helped my care team understand what was important to me and helped clarify my goals of care. Faced with an incurable disease and a prognosis where only 11 to 20 percent survive to five years and there is no statistic for 10-year survival because it so rarely happens, I came to understand that my priority was to seek a “Niagara Falls trajectory” — to feel as well as possible for as long as possible, until I quickly go over the precipice. Quality of life is more important to me than quantity of days, if they are miserable days.
Following a discussion with my oncologist (a conversation that would be reimbursed if you in fact move ahead and change your rules), we initially decided on a palliative regime to slow the cancer’s spread with the least amount of burdensome side effects. We would not impose the most difficult curative treatments on an incurable disease.
This treatment has included a pill I take each evening to hold back the hormones that fuel my cancer, coupled with a monthly infusion to keep my bones strong. I don’t take most difficult treatments, the typical noxious cocktail of two chemotherapy drugs that 90 percent of people with inflammatory breast cancer receive, coupled with surgery to remove my breast, followed by weeks of radiation and more debilitating chemotherapy.
When I suggested a second opinion after I was diagnosed, my oncologist blessed it. Sadly, when I sat down with this esteemed expert, he didn’t ask about my goals or wishes. Instead, he suggested an aggressive, hail-Mary treatment regime — including rounds of chemotherapy, a mastectomy and radiation — that would have compromised the quality of my remaining life without any real benefit. There was no conversation. He was expert in everything but what really mattered to me. I thanked him for his time, and left.
[How I decided to live a good life with the time I have left.]
I am pleased to report that the subsequent nearly five years have rewarded my decision to seek palliative rather than more aggressive treatment. The cancer has spread a bit farther from my spine and into a couple of my ribs. But because my treatment focuses on helping me live well and feel well, I haven’t been in the hospital. I feel great. My pain has been minimal so far — with one exception.
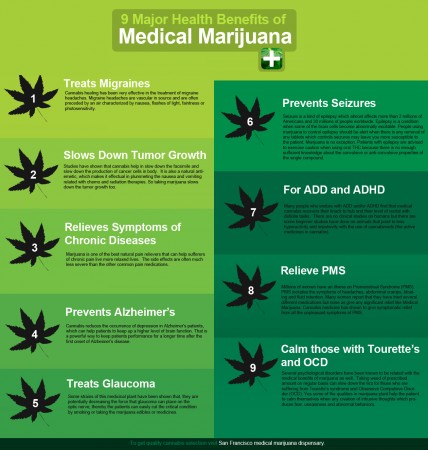
Six months ago, the cancer spread to a new spot, my fourth and fifth ribs. It was painful. The standard treatment is 10 to 20 doses of radiation to get rid of the pain. My palliative care provider, an expert in fostering discussions about goals of care, said that a recent recommendation of the Choosing Wisely Campaign, which promotes patient-physician conversations about unnecessary medical tests and procedures, suggested that I could get rid of the pain with a single, larger dose of radiation. It worked like a charm. I felt better, avoided the terrible side effects of repeated radiation, got immediate relief and avoided paying for all the unnecessary doses of radiation.
I estimate I’ve saved about a million dollars by avoiding care I do not want, which includes the cost of chemotherapy, radiation, surgery to remove the breast, at least one hospitalization for that care, and the follow-up care to the surgery. Chemotherapy alone would have cost upward of $500,000. Insurance would have covered much of this, but not all.
Meanwhile, I continue to work full time and have redoubled my efforts to improve the health-care system for older people. And I live a good life with serious illness. I have climbed the Great Wall of China, ridden a camel in the Jordanian desert and water-skied to the Statue of Liberty, and I continue to enjoy time with my family and friends.
So my original advance-care planning discussion has been lifesaving. It has also saved the health-care system a great deal of money.
All people deserve care that meets their emotional and financial needs. Unfortunately, health-care providers, including those paid by Medicare, have not had the incentives, time or training to sit down with people facing a life-threatening illness and discuss what’s important to us as our health deteriorates, things such as where we want to die (I want to be at home), what’s most important (control my pain) and what treatments we want to avoid (I don’t want to be on life support and don’t want to be resuscitated). As a result, our system provides a lot of expensive crisis care as people reach the end of life — care that people, if asked and engaged, might say they never wanted.
This does not have to happen. High-quality advance-care planning discussions help people like me understand their options and make their wishes known. They can identify a surrogate to make decisions when they are unable to, and they can document their preferences in their medical records. These discussions — which should be ongoing, not just one-time — can revisit decisions in the face of new challenges, and over time they can guide providers to deliver the care that patients and their families want.
The benefits of a rule from Medicare covering such conversations are clear: better health, better care and, in many cases, lower costs. Most important, these conversations will be lifesaving, enabling those of us with serious illness to live the way we want to, fully and deeply for as long as possible.
Thank you for your consideration.
Complete Article HERE!