A legendary design firm, a corporate executive, and a Buddhist-hospice director take on the end of life.

By Jon Mooallem
There’s an ugliness — an inelegance — to death that Paul Bennett gradually came to find unacceptable. It seems to offend him the way a clumsy, counterintuitive kitchen tool might, or a frumpy font. At first, that disgruntlement was just “a whisper in my mind,” Bennett explains. “But it’s gone from being a whisper to a roar.” The solution, when it finally occurred to him, felt obvious. “Oh,” he told himself. “You need to redesign death.”
Bennett is 51 — 30.7 years to go, if the demographic data is reliable — a blindingly energetic British man with unruly brown hair. He works as chief creative officer at Ideo, the global design firm that’s renowned for its intuitive, wizardly touch. Over its 25-year history, as Ideo has expanded from simple product design into branding, organizational design, and management consulting, it has worked in virtually every corner of our economy: A list of recent clients includes Genentech, Bank of America, the Centers for Disease Control, JetBlue, and the Today show. Ideo’s founders designed Apple’s first mouse and the stand-up toothpaste tube. Its designers have overhauled San Francisco’s public school-lunch program and helped reorganize government agencies in Singapore and Dubai. They’ve developed a toilet for low-income families in Ghana. They’ve built a better Pringle.
Often, the firm’s brilliance rests on showing clients something obvious that’s been overlooked, or cutting through buildups of false assumptions. “I think we sense-make really well,” Bennett told me. One example he likes to cite involved attaching mirrors to the gurneys at a Minnesota hospital so that patients could actually make eye contact with the doctors and nurses wheeling them around.
Bennett works out of Ideo’s stylish San Francisco office, at Pier 28 on the Embarcadero, and like others operating at the top of the Bay Area’s innovation economy, he doesn’t have a concrete job description: It can be hard for an outsider to sense-make what he does. According to his company bio, he is responsible for “cross-pollination of ideas and insights” and “traveling, learning.” As Ideo has grown, the company has delved into more abstract, conceptual work, driven not by specific clients but by Bennett and the other partners’ own evolving fascinations. Bennett’s role is to stoke the firm’s bigger ambitions, then go out and excite clients about them, too, transforming those personal obsessions into business opportunities. (When we met one morning last spring, he’d just returned from chatting about “reinventing Judaism” with some unbelievably fantastic rabbi in Los Angeles. “I love this guy,” Bennett raved.) He is quick-witted, blunt, and irrepressibly optimistic about nearly everything. In meetings you can feel junior designers’ eagerness to impress him — to electrify him — and he carries himself with a kind of fidgety, ecstatic gravitas. Imagine Don Draper played by Ricky Gervais.
Bennett’s fixation on death began with the death of his father. He was close to his dad; in a recent talk, he likened his childhood to the plot of Billy Elliot, a story “about a little nelly gay boy who twirled in the northeast of England” and the exceedingly masculine father who dared to love him. Bennett, in fact, traces his identity as a designer to the day in 1974 when his father, Jim, a former military pilot, brought home The Golden Hands Encyclopedia of Crafts. Jim Bennett then spent the next two years sitting with his son, making macramé and knitting God’s eyes, so that sensitive little kid could explore his talent and find his confidence. In 2001, Bennett’s father wound up in a hospital bed, stricken with bone cancer. Bennett was 5,000 miles away at home in San Francisco. He told his father he’d be on the next flight, but Jim ordered him not to come. Eventually, Bennett understood why. His father had painstakingly maintained his dignity his entire life. Now “he was trying to somehow control that experience,” Bennett says. “He was designing the last granule of what he had left: his death.”

So much about death is agonizingly unknowable: When. Where. Lymphoma or lightning strike. But Bennett recognized there are still dimensions of the experience under our control. He started zeroing in on all the unspoken decisions around that inevitability: the aesthetics of hospitals, the assumptions and values that inform doctors’ and families’ decisions, the ways we grieve, the tone of funerals, the sentimentality, the fear, the schlock. The entire scaffolding our culture has built around death, purportedly to make it more bearable, suddenly felt unimaginative and desperately out of date. “All those things matter tremendously,” Bennett told me, “and they’re design opportunities.” With just a little attention, it seemed — a few metaphorical mirrors affixed to our gurneys at just the right angle — he might be able to refract some of the horror and hopelessness of death into more transcendent feelings of awe and wonder and beauty.
In 2013, bennett started sharing his ideas with the other partners at Ideo, selling them on death as an overlooked area of the culture where the firm could make an impact. He had a very unspecific, simple goal: “I don’t want death to be such a downer,” he told me. And he was undaunted by all the dourness humanity has built up around the experience over the last 200,000 years. “It’s just another design challenge,” he said. His ambition bordered on hubris, but generally felt too child-like, too obliviously joyful, to be unlikable. One time I heard him complain that death wasn’t “alive and sunny.”
Ideo realized there was a big opportunity in death. There are currently 76 million American baby boomers inching reticently in its direction. “We’re a generation that’s used to radicalizing things,” Bennett explains. Now, as many boomers watch their parents die just as Bennett had, accepting the soulless, one-size-fits-all deaths that society deals them, they seem to be rebelling one last time. Everywhere Bennett looked — New York Times opinion pieces and Frontline specials; assisted-suicide laws; the grassroots Death Café movement, where folks get together for tea and cake and talk about their mortality; a campaign in La Crosse, Wisconsin, that got 96 percent of the entire town to fill out advance directives, spelling out their wishes for end-of-life care — he saw his generation striving to make death more palatable, more expressive. And at the far extreme is the crop of phenomenally well-capitalized biotech startups working to get around the insufferable inconvenience of death altogether, either through science-fictionesque “radical life extension” treatments or by uploading your consciousness to the cloud. (These include Calico — Google’s so-called “Immortality Project” — and J. Craig Venter’s company Human Longevity, Inc. The founder of Oracle, Larry Ellison, who set up the Ellison Medical Foundation to defeat death, has explained his motivation succinctly: “Death has never made any sense to me.”) One way or another, Bennett told me, “We’re all holding hands and saying, ‘Forget that shit. Not going to happen.’”
I followed Bennett’s work over the past year — a journey that, in the end, may reveal less about the death of people than it does about the life of ideas, particularly the brand of Big Idea that distinctly Californian institutions like Ideo send careening through the culture. Right away, Bennett understood it would take years to see the sort of wholesale shift he was imagining — a generation or more. There was so much to do, he could really start anywhere. He just needed to find a few suitable clients, to locate a few fissures through which a genuinely different conversation about death could begin to flow. And because he was looking in San Francisco, in the year 2014, the first one he found was a startup building an app.
The app was called After I Go. The president and ceo of the company building it, Paul Gaffney, had founded two other startups but had spent most of his career working near the top of large corporations such as Charles Schwab, Office Depot, Staples, and aaa, primarily helping them find their footing online. He was 47, a loose and affable guy despite being excruciatingly analytic at his core. Once, when I asked Gaffney about himself, he explained that his “personal value proposition” is “establishing a vision for a new outcome particularly in consumer-related spaces enabled by the novel use of technology” — but he managed to sound human when he said it, even warm.
Gaffney described After I Go as TurboTax for death: a straightforward app that would allow people to write wills or advance directives and, in general, preemptively smooth out the many ancillary miseries that can ripple through a family when someone dies. Bank accounts, life-insurance policy numbers, user names and passwords, what night the garbage goes out — all of it could be seamlessly passed on. Whatever fear or despair people feel about death is only heightened by the fear that, because they never got around to making the necessary preparations, their death might burden the people they love. Gaffney assumed there’d be a big market for an app that eliminated that risk. “Simply providing people with that sense of organization would be a huge emotional payoff,” he said. But he was spectacularly wrong. Bouncing his ideas off potential investors, he quickly understood that no one welcomed a chance to prepare for death. It’s thankless drudgery — plus, it reminds you you’re going to die.
Gaffney realized he couldn’t just build the right tool; he also had to build the motivation to do the job in the first place. That’s what people would pay for. Suddenly, the work After I Go needed to do was no longer rational but emotional — which is to say, far outside Gaffney’s personal value proposition. (“I learned a long time ago that I’m not a good test case for how human beings respond,” he explains.) And so he hired Ideo to help.
The Convening, as everyone called the first After I Go strategy session, happened early last April, not long into Gaffney’s three-month residency at Ideo. About 25 people gathered in the large studio of the firm’s San Francisco office, arrayed on colorful armchairs and couches.
“How can death be designed?” Paul Bennett said, rising to set the tone. He explained that he’d grown up in Singapore, where it’s customary to burn intricate paper sculptures at funerals: paper televisions, paper houses, paper Cadillacs — all kinds of gorgeous extravagances that would, via their rising smoke, accompany the deceased into the beyond. As Bennett put it, “They wanted the dead person to go into the afterlife with all this awesome shit!” But Bennett’s family eventually returned to England, he went on, a place where even the joyful parts of life were muted by the gray and cold. And he was shocked by how different funerals were there, how leaden and awful. It was proof, he explained to the Convening, that how we feel about death is up to us. Then he looked at everyone and, with great earnestness, asked: “Why can’t death feel more like life?”
From there, the Convening broke into four smaller circles to think through the possibilities for After I Go. Bennett assumed the role of facilitator and secretary in his group, manically scribbling notes with a Sharpie. When one woman shared a clip on her laptop of a New Orleans jazz band marching behind a casket, Bennett told her, “I love it. I’m writing ‘jazz death.’” He scribbled jazz death on a pink Post-it and slapped it against the wall.
Paul Gaffney was seated in Bennett’s circle and explained that, like Bennett, his interest in death had been stoked by recent personal experience. His wife and her siblings were now organizing their parents’ affairs after their father had been diagnosed with dementia. It sharpened Gaffney’s understanding of just how much disarray survivors can be left to organize, and how much can get lost. Still, Gaffney confessed, while he’s filed his own important information in an orange folder at home, and periodically reminds his wife it’s there, he rarely gets around to updating it. “What’s your folder called?” Bennett asked him, Sharpie at the ready. “It’s called the Orange Folder,” Gaffney said.
From there, Bennett started posing a series of “how-might-we’s” to the group — Ideo-speak, it seemed, for questions. The first was, How might we get people to start using After I Go? Ideas started firing — “death Tupperware parties,” “will weekends” for couples in Napa, commandeering Groundhog Day as a national “Death Preparedness Day” — until someone brought the conversation back to Gaffney’s orange folder. Maybe After I Go needed to sell a physical object like that in stores, with instructions and a download code inside; it would be a kind of totem, committing you symbolically to starting the preparation process. This idea felt promising until one woman asked, “But if it’s in the consumer space, what’s the draw?”
And there was the underlying tension. In short, why would anyone buy death? Consumer culture is always aspirational: We’re lured along by desire and joy, chasing ever-receding rewards. Gaffney’s challenge seemed to be convincing consumers to step off that rapturous treadmill and think hard about the very thing it was arguably designed to distract us from. That’s why, in part, the business excited Paul Bennett: The app could help reintegrate death into our lives. It could encourage us to start making peace with the inevitability of dying and start making decisions to shape its other aspects — here and now, and not only at the last moment, like Bennett’s father had, when there are few decisions left to make. The question, really, was how to lure ordinary, preoccupied people into contemplating big, transcendent ideas like mortality, continuity, legacy. Once, religion had cleared that space in our lives. Now it was up to Ideo to whiteboard it out.
Eventually the group moved on to another exercise using a handout about Bob and Sherry Alvi, a fictional couple outside Boston. There was even a photo of the Alvis with their two daughters: They looked cornfed and chipper, grinning in front of a fireplace. Bob, the handout explained, was an After I Go user. He was also almost dead; he’d been in a car accident and was in critical condition. And so the Alvis found themselves on the cusp of one of After I Go’s Key Brand Moments — which is to say, death. The question was, How should After I Go make contact with the newly widowed Sherrys of the world?
The circle was quiet. This one was trickier. You can’t just email her, right? The consensus was no, though the idea seemed to hang there momentarily until Bennett finally concurred. (“Death feels very analog,” he explained.) Someone proposed sending Sherry a “condolence kit”: a courier could bring all of Bob’s passwords and information along with a nice bottle of wine. Then, quietly, one man asked, Why not deliver the information to Sherry in a letter, handwritten in advance by Bob?
Instantly, the circle felt electric. Bennett was vibrating; he loved it. Others chimed in, building off the idea, and Bennett began writing madly across multiple Post-its, not coming up for air. (An awkward disclosure: The person who suggested the handwritten-letter idea was me; Ideo strongly encouraged me to participate in the Convening, so I did.) Bennett kept on scribbling. When he finally turned around, a chain of Post-Its behind him read: “Selling a service → Delivering a Message → Executing A Wish → Providing Comfort.” This was the magnificent evolution that Gaffney’s company had just hurtled through in his mind. After I Go could carry back so much more than passwords and legal information from beyond; it could transmit memories, messages, love. That was the emotional payoff, the only way to entice people into filling out all those tedious, frightening forms. Bennett tapped at the word comfort. Then he circled it. “That’s our big idea,” he said. “Comfort is the product. That’s the genius of it. You sell that.”

They had started somewhere practical — living wills, checking accounts, who should cancel the gardener — and landed somewhere metaphysical: an opportunity to comfort your widow from the grave. It was break time. Gaffney and the Ideo designers got up for coffee and snacks, but Bennett stayed at the wall, writing more Post-its, shuffling and collating them, preparing a little presentation so that, when all four circles reconvened, he could unveil these insights for the group.
“We’re moving from estate planning to story building,” he said, to no one in particular. Then he sat cross-legged on the carpet and waited, twirling his Sharpie by the bent clip on its cap.
In the weeks after the Convening, Gaffney and a handful of Ideo designers got to work in a small windowless room at the southern edge of Ideo’s office. Gradually, they covered the walls in sketches, clippings, and printouts, teasing out the tone and aesthetic of the app and imagining all possible features they might build and test.
Some of the drier mock-ups included pages to help users draft a will or designate power of attorney, or offered portals into a network of vetted legal professionals who could help. But most took bigger, more inventive leaps forward, such as allowing users to curate shareable collections of “funeral inspirations” like a Pinterest page or Amazon wish list; samples were pinned with photos of blood-orange spritzers, Japanese lanterns, and succulents. (“For my sunset party, I want deviled eggs,” one read.) The team’s most mind-bending innovation was something it called After-Gifting, whereby a person could arrange to dispense preselected birthday gifts to family members for years after his or her death. Baby booties made from your favorite jacket could be delivered to a newborn child you’d never meet. The dead might also send time-delayed text messages on special occasions, or just to say hi. After I Go could even digitize your handwriting into a font so that fresh, personalized content could continue to be generated on your behalf.
In other words, After I Go wasn’t only a tool for mundane, administrative death prep anymore. It had inflated into something far bigger — even if, in this freewheeling brainstorming phase, it wasn’t always 100 percent intelligible what that was. There was also a strange shortsightedness to some of the team’s ideas. Ginning up years’ worth of texts for your widow might comfort the person who is dying, for example, but would an actual widow want to keep receiving them? (Imagine if one landed three years later while she was on a date.) Another write-up, meanwhile, explained an alternate brand concept the team had worked up called Bon Voyage. Bon Voyage was all about celebrating “our aspirational desire for richness, beauty and simplicity in this life and whatever comes next.” To illustrate that theme, designers had mocked up the Bon Voyage account of a hypothetical user named Wilfredo.
The screen caps looked like a Madewell catalog — spare and white, with old childhood photos of the deceased arranged around quotes from loved ones and floating images of his cherished possessions. It was gorgeous, but also jarring; essentially, they’d built a luxury brand for death. And yet any feeling of elitism or superficiality was also undercut, albeit a little awkwardly, by their choice of Wilfredo. “He was the best Midas muffler manager we ever had,” one testimonial read. Nearby was a photo of the canteen Wilfredo carried “while serving as a Sandinista.”
That spring, Gaffney’s original, strait-laced vision of the app began to recede into a cloud of more emotionally indulgent features and evocative marketing copy. This was fine with Gaffney, even thrilling: Investors, he found, were responding to the app in an entirely new way. (At one meeting, Gaffney says, a prominent venture capitalist interrupted his pitch and shouted, approvingly: “I want my mother’s damn frittata recipe!”) Gaffney told me, “We now have to pivot and operate exactly like any other startup would.” All he wanted was to build a product that people would use.
One afternoon at the end of April, in the middle of that pivot, Gaffney and Paul Bennett gave a short tour of the project to a man named BJ Miller.
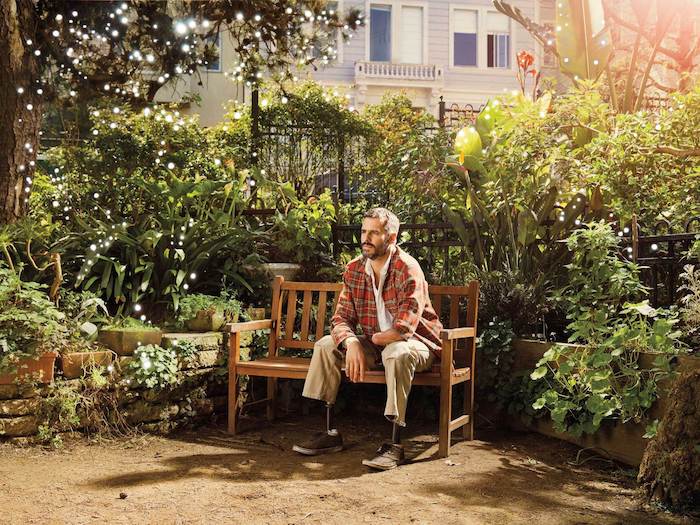
Miller is the executive director of San Francisco’s Zen Hospice Project, which since 1987 has quietly helped pioneer the field of palliative care. Loosely defined, palliative care is an empathic approach to medicine and end-of-life care that considers the many nuanced emotional, spiritual, and physical experiences of the patient and his or her overall well-being, rather than formulaically treating a medical condition. Zen Hospice deploys a corps of more than a hundred trained volunteers into homes and at a city hospital, but its centerpiece is a tranquil six-bedroom Victorian home in Hayes Valley known as the Guest House.
The Guest House has an extraordinary feel to it, deeply spiritual without being overbearing or mushy. Residents are invited to meditate with staff and often gather in the kitchen to casually enjoy the rituals and smells of cooking, even if they’re unable to eat. Miller told me he recently supported the decision of a woman at the Guest House with terminal cancer to start smoking again — as he explained it, it was worth it for her to feel and use the very lungs she was losing; it deepened her experience of letting go. In short, Miller explained, Zen Hospice’s power comes from recognizing that “dying is a human act, not just a medical one.”
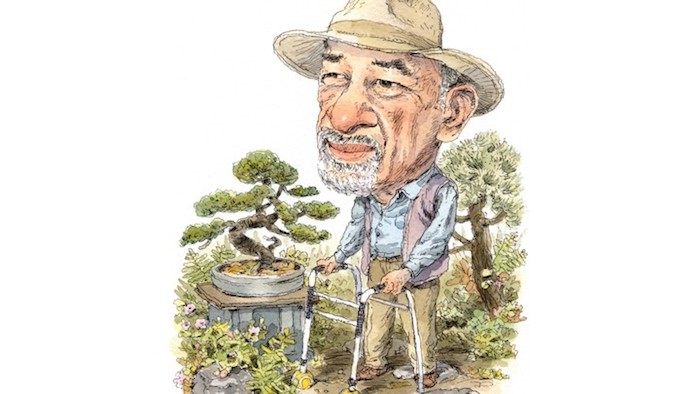
Miller had been introduced to Ideo about a year earlier, and quickly achieved a kind of guru status among many at the firm. (“He came in and everyone instantly fell in love with him,” one Ideo staffer told me.) He is 44 and preternaturally poised, the sort of person who, after speaking about death and dying on a public-radio call-in show last year, not only read the comments that poured onto the show’s site later, but responded, compassionately, to each one. In person he is blessed with a blazing magnetism that can’t be overstated — a recent acquaintance described him to me, only half jokingly, as “the most magnificent human in the world” — and could pass easily as a Hollywood leading man, with tousled, slightly silvering dark hair and a dimpled grin. He is also missing half of his left arm and has two prosthetic legs.
In 1990, while an undergraduate at Princeton, Miller was out late with some friends and decided, for the fun of it, to climb atop an electric train car. The electrical current arced from a piece of equipment into his wristwatch, sending 11,000 volts through his arm and out his feet, nearly killing him. (Miller still wears the watch occasionally; it works.)
His recovery was long and taxing, but the injury intensified his intellectual curiosity about death and suffering. When Miller returned to school, he began studying art history, fascinated by how artists make sense of the darkness and pain of the human experience. Then, after playing volleyball in the Paralympic Games and founding a tea company, he went to medical school and eventually found his calling in palliative care, especially for terminal patients. (He still practices medicine part-time at ucsf.) Miller felt he was uniquely qualified. “A lot of physicians will work their whole life on a disease that they’ll never have,” he says. Miller, at least, had come as close to dying as anyone could
Paul Bennett was drawn to Miller immediately. Miller was a physician, intimately familiar with how bodies fail and shut down, but he’d also spent the two decades since his accident attuning himself to the same aesthetic dimensions and deficiencies of the dying process that Bennett was now obsessed with. That is, Miller had a profound head start when it came to redesigning death, and he and Bennett quickly fell into a wide-ranging dialogue. In an email to Bennett early last year, for example, Miller wrote: “I’d say that humans have thrived by turning every need — every vulnerability — into something in its own right.” Shelter becomes architecture, he noted. Reproduction gets wrapped in romance and love. And “think of all the cultural significance and artistry and labor that goes into [eating].” Miller wanted to bring that same creative power and meaning-making to death, but he had trouble finding a sounding board for those ideas in the medical community. He was as grateful to find Bennett as Bennett was to find him
Last February, Bennett invited Miller to an orientation for a small team of Ideo designers on the work he was hoping to undertake. Because it felt wrong to talk about death in a conference room, some junior designers took it upon themselves to build a Death Yurt at the center of Ideo’s studio — a black, candlelit enclosure reachable only by crawling through a long, dark tunnel. (“It was like a sweat lodge,” Bennett says.) As homework, Bennett had asked everyone to design their own funeral, and he kicked off the discussion. He explained he’s always been terrified by the knowledge that he’ll die alone. (Bennett’s partner is 15 years older than he is, and they have no children.) But lately he had been reshaping the image in his mind. If he was going to die alone, he said, he’d like to do it outside, in Iceland, under the quivering brilliance of the Northern Lights.
Huddled in the Death Yurt, Miller felt simultaneously invigorated and dubious. On the one hand, this was precisely the sort of more joyous conversation he wanted to encourage people to have long in advance of their own deaths. (“I felt like I was watching Paul be converted to the possibilities,” he says.) Miller had seen firsthand that, because we spend our entire lives avoiding thinking about death, when it finally comes into view, there’s a thicket of panic, denial, or disbelief to cut through before people can focus, more mindfully, on the experience and begin to make decisions to improve their last days. Then, of course, you still have to reconcile those hopes with the exigencies of the health care system, which can be torturously inflexible. When you sit with a dying person, Miller says, “Time is always in the room. … At best, you’re able to salvage some peace or comfort for a moment.”
And yet Miller also knew that these more imaginative conversations about death needed to be channeled in just the right way. In the Death Yurt, Bennett and his team seemed to be caught up in what Miller recognized as the “endocrine rush” of finally facing death head-on. That exuberance, while helpful, needs to be moved past; otherwise, it can wind up derailing more practical conversations, or alienating people on aesthetic or socioeconomic grounds. For one thing, Miller later told me, “Paul’s Iceland idea presupposes you can time all that” — that you could fly him over and wheel him out at just the right moment, then cue the Lights. “You don’t want to shit on somebody’s beautiful idea,” Miller said, but “if you start talking about dying well or dying a ‘good death,’ then you also set people up to fail at death
Miller seemed to bring that same sobering perspective to his tour of the After I Go workshop. At one point, the lead Ideo designer on the project, Denise Burchell, was talking him through a potential After-Gifting feature the team would eventually call Remembrance Maps: walking tours of sentimental locations, left to loved ones either as actual maps or location-based software. For example, your deceased grandfather could ping you to suggest you go sit on a particular park bench where he and your grandmother used to enjoy the view, 300 yards from where you’re standing. The power of features like this, Burchell explained, was that you wouldn’t be showering your loved ones with “generic memories” but “personally relevant ones.” “These,” she said, “are your memories.”
“Can I ask you a question?” Miller interjected politely. “The quest for immortality in general is very problematic,” he began. He seemed to be feeling the same mix of hopefulness and ambivalence he’d experienced in the Death Yurt. He wanted to know if they’d thought through the implications of catering to what, essentially, is our narcissism. Fundamentally, Miller’s work is about helping people let go of that fierce attachment to the self — the urge to hang on to it at all costs. Was Gaffney’s team finding they could tap into that impulse in a purely positive way? “Is there something good in that compulsion?” he asked.
Burchell seemed taken aback by the question. They hadn’t launched the app yet, not even in beta. “At this point,” she said, “we just have hunches.”

By the end of the summer, After I Go was effectively dead.
There had been remarkable progress before then, however. Gaffney’s vision of the app had sharpened. What they were building, he realized, was a “private social network,” a lockbox where families could collaboratively collect and curate their memories. It was as much a place for living people as for dead ones. Just as sites like Ancestry.com allowed people to discover the identities of their ancestors, he told me, uploading material to Gaffney’s product would allow people to one day discover the stories of their ancestors. All the functionality of the app — they had renamed it Keeps by this point — started to snap into place around that insight; it felt full of promise. But even as Keeps started humming along conceptually, Gaffney’s belief in it was crumbling.
For one thing, there was uncertainty about how Keeps could ever be monetized. And it was proving impossible to hire the prototypical gang of slavish, single-minded twenty-something coders to work for the company. (Young people, it turned out, weren’t enthusiastic about building a digital lockbox for baby boomers to stuff their memories into; unlike apps that called you a car or delivered food to your door at 2 a.m., its mission was totally unrelatable.) Meanwhile, Gaffney was realizing it could take another year of development, maybe more, to build this new, sprawling incarnation of the app he was imagining — and that he would need to raise the money to fund that process. He told me, “I started to feel like I’d probably feel miserable trying to make that work, rather than feeling confident that we would make it work.”
Then, just as all these unnerving roadblocks came into view, Gaffney was offered a job as senior vice president of information technology at Home Depot in Atlanta. He took it, putting Keeps on hold indefinitely. And by September, there he was: smiling on Home Depot’s senior-leadership web page, wearing one of those orange aprons over his dress shirt.
“You can imagine how disappointed people here are,” one Ideo staffer told me when I first heard the news. Paul Bennett had been imagining a massive cultural shift and had invested at least a share of that ambition in Gaffney’s app. But for Gaffney, closing down Keeps had been a simple, unemotional calculation: He’d sized up the obstacles, decided it wasn’t worth it, and walked away. He wasn’t on a quest to confront some metaphysical dilemma, after all; he was building a consumer product in Silicon Valley. Keeps was just a startup, and a seed-stage one at that. Startups collapse every day.
From a business standpoint, Keeps had arguably done everything right. The app kept pivoting, as apps must. It feverishly chased what it thought we wanted most, until satisfying those desires seemed too difficult, at which point it suddenly pivoted into oblivion.
And that trajectory felt familiar. It’s hard for any of us to face down what’s difficult, frightening, or fragile in life, no matter how earnestly we may want to internalize and reimagine it. Gradually, we get distracted; we drift away from what we suspect might really matter.
Bennett hoped the app could lead us out of that problem. And it might have. It did, however, wind up illustrating the problem exquisitely.

Bennett moved on quickly. He was proud of the work Ideo did for Paul Gaffney and harbored no hard feelings. “Paul had other things he wanted to do,” Bennett told me. “The lesson was, you can’t just go into death lightly.”
That fall and winter, Bennett continued to proselytize about death and design. He talked to Ideo’s health care clients. He talked to philanthropists. He spoke at the launch event for a “healthtech incubator” in Chicago, for a crowd of 200 people. He talked to a “mortician in Los Angeles who wants to do groovy, Six Feet Under rock ’n’ roll funerals” and to a visual artist who’d designed a bodysuit made of fungi as an alternative means of burial. (“You become this organic sculpture at the end!” Bennett explained.) For the most part, these conversations were casual, but in January Bennett told me his goal for 2015 was to convert several of them into actual business propositions. Already he’d landed what might have been his ideal client all along: BJ Miller and the Zen Hospice Project.
Zen Hospice had hired Ideo for the better part of a year to work on several ambitious fronts at once. Miller told me Ideo would first help them “better articulate ourselves to ourselves” — zero in on what makes Zen Hospice’s philosophy and style of care valuable, and enhance it even further. A team of designers was already prototyping ways to improve the experience of residents and staff at Zen Hospice, including dreaming up new, more imaginative physical spaces designed specifically for dying. Then Ideo would help Zen Hospice to step into the public sphere as a potential model for reforming end-of-life care. Zen Hospice wanted to enlarge the public’s appreciation for how much more meaningful death could be. It wanted to build a coalition of similarly minded palliative-care workers and organizations, lobby for more enlightened health care policies, and get insurers to cover care at facilities like its Guest House, laying the economic groundwork for more of them to arise. “I think,” Miller told me modestly, “we’re interested in gestating something like a movement.”
By mid-January, the company had dispatched two researchers to the Guest House, where they’d spend two weeks observing and interviewing staff and volunteers and speaking with families of former residents. Zen Hospice was a small, bootstrapping organization that had never had the luxury of stepping back and codifying its organizational identity, much less a strategy for explaining its mission to outsiders. And so the two women from Ideo — an anthropologist and a “business designer” — were working up an ethnography of the place, allowing Ideo to key into the essence of Zen Hospice and then build out its brand. Dana Cho, an Ideo partner who oversaw the research, told me it’s always a challenge to hew through the stale vernacular that builds up inside any field and get people to loosen up and truly reflect on the work they do every day. And so the researchers came armed with props. In one exercise, Guest House staffers were shown pictures of celebrities — Julia Roberts, Oprah, Dame Judi Dench — and asked to describe what qualities Zen Hospice shared with each.
Ideo, meanwhile, had encouraged Miller to reach out to ted, and he was soon invited to speak on the final day of the ted conference in Vancouver in March. This was a tremendous opportunity: Bennett and Miller both sensed that the scattered but intensifying conversation about death in the culture was searching for some center of gravity. To become a genuine movement, it needed some stake to wrap around and grow — an ambassador like Miller, or an organization like Zen Hospice, or even an entire community, like San Francisco. “San Francisco feels like a very logical place to me for death to be normed,” Bennett told me. “It’s a place where radicalism was born. Why can’t the radicalism of death be something we help build here?” It’s a clumsy analogy, maybe, but it was easy to imagine Zen Hospice emerging as a kind of Chez Panisse of death, and Miller as death’s Alice Waters.
The firm’s partnership with Paul Gaffney had fizzled because Gaffney’s startup was a business with no ideological center. He wasn’t married to any particular idea; as Gaffney once told me, he was only “married to delivering real value.” Miller, on the other hand, was delivering compassion. His whole life seemed to cling to a certain hard-to-articulate ideal — a determination since his accident, as he put it, to live a full life and stay rooted in real things. Even as he opened his organization to Ideo’s efforts, in fact, he felt conflicted about being cast as a spokesman. He still considered himself a relative newcomer to palliative care and was too introspective, and too humble, to crave any celebrity. In short, what made him reticent was his integrity. It was also what convinced Bennett this could work
An encouraging push and pull seemed to have developed between the two men. A year earlier, Bennett’s crusade against death seemed to be motivated entirely by his frustration with the way his father died. But over time it was evolving into something more nuanced, inclusive, and humane. When I asked what Bennett hoped to accomplish with Zen Hospice, he told me, simply: “Best-case scenario is that more people in more places talk about death in a design-rich way.” Miller, meanwhile, confessed he’d previously dismissed branding as “some kind of trickery,” but that since starting work with Ideo, he had begun “to appreciate it as its own craft” — a clarifying process, and a tool for doing good. He was fine-tuning his ted talk, committing himself to his place on that stage.
In mid-February, Miller and a few of his board members arrived at Ideo’s San Francisco office for the same species of strategy session that Bennett had held to launch the work with After I Go. The tone of this meeting was much less rambunctious, though, and it was held in a smaller, more minimalist room around a loosely arranged circle of bare metal chairs. (I noticed no one used the word convening, either; everyone just called it a workshop.) Wooden boxes of Sharpies and brightly colored Post-its waited on a table at the back of the room. This time, it felt like something might stick
Complete Article ↪HERE↩!