— A Q&A on supporting people at end of life in care homes

With more and more people expected to die in care homes over the coming years, it’s more important than ever the professionals working there get the practical and emotional support they need to provide excellent end of life care.
By Dr Julie Watson
When we think about what it means to die at home, it can be easy to jump to one idea of what this looks like. That is, a rented or owned flat, house or other dwelling. But for a growing number of people, ‘home’ at the end of life means the communal setting of a care home.
Right now, 20.5 % of all deaths and 34.6% of deaths of people over 85 happen in care homes. The number of people over 85 is set to increase by 90% by 2048, meaning this figure is only going to rise. The median length of stay in a care home is now 15 months, which means deep relationships form between staff and those in their care.
Good palliative care focuses on quality of life, and also accepts dying as a natural process. It’s vital people working in care homes get the support they need – both practical and emotional – in order to be able to give people in their care the best end of life experience possible.
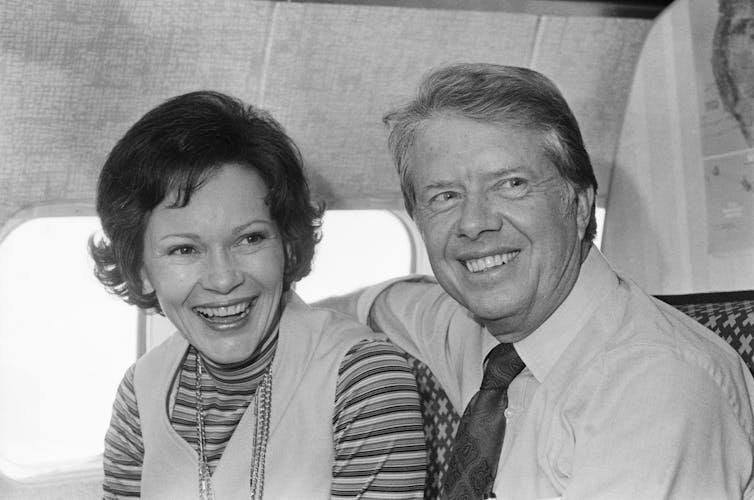
I spoke to Senior Carer, Loren Hunt, who’s worked in a care home for several years, about what this looks like for her.
Q: First things first, could you describe a typical day?
We help the residents to get up, get dressed and start their day, have breakfast and then see what activities they’d like to do. Throughout the day, we help them with things like going to the toilet and if they need assistance with eating and drinking. We check their general well-being, make sure they’re comfortable and safe.
In the evening, we help them get into their pyjamas, washed and ready for bed. It’s personal care, but also a lot of general life support and making sure they’re happy and comfortable.
As a Senior Carer, I’m responsible for delegating tasks to the team as well as caring for people directly.
Q: What’s the best thing about working in a care home?
My favourite part of my job is just getting to know the residents and building that friendship and connection with them. I enjoy helping people to get the most out of life… Having a dance and being silly, making them happy. Trying to get them to participate in things. I think there’s a perception that if you go into a care home, you just sit in a chair all day and that’s that. But it’s not like that really.
Some of the people we care for have had such interesting lives. We’ve got so many residents who have done a lot of travelling and lived abroad and have wonderful stories. So it’s really nice just having chats about that with them as well.
Q: What’s the most challenging part?
We’re taught to not get too connected to the people in our care so that we don’t get upset when they do pass away. But when you do see people deteriorating and then getting to that point in life where they’re reaching the end, I think that’s the hardest part.
It can take months and months, or it can be really, really quick. But as soon as you realise it’s coming, it’s sad. And of course, when they do ultimately pass away, it is upsetting because as much as you’re advised not to get too emotionally attached, you can’t help it really.
I feel like you wouldn’t be doing your job as well as you could if you didn’t get connected to the people you care for.
Q: What are the challenges of caring for someone who’s approaching the end of their life?
If you’ve known someone for a while, it can be hard to adjust to their new needs because you get so used to them being able and not needing as much support. You have a routine together, so when it suddenly changes you have to adapt and think: ‘Ok, how can I now best support this resident now?’
And it is a lot of learning to do, and there may not be much time. It would definitely be helpful for more training on that side of things. It’s the area where I personally feel the least knowledgeable. Because it’s so different from person to person, and there is no set of rules which say: ‘OK, when this happens, you do this’, because everyone is different.
Q: Could you give an example?
One area which is often spoken about is eating and drinking at the end of life. There’s this perception that as soon as someone’s palliative, they don’t need to eat proper food anymore. That fluids should be thickened, or food should just be things like ice cream and yoghurt.
But that’s not necessarily true for everyone. For some people it might be, but others might manage to eat and drink fine until the very last stages. Or they might just want a taste of their favourite food. There’s nothing to say that if they want a taste of salmon or a roast potato, they can’t have that. They might not have a lot, but it means they’re still able to have that pleasure.
I think carers are often scared, thinking ‘what if I give them this piece of potato and they choke?’ so it feels safest to default to the ‘safest’ option. To have some help with confidence so that, for example, if someone does ask for a bite to eat, you can use your judgement and understand how to make it as safe as possible.
Q: Do you experience the very end of someone’s life very often?
Yes, people will quite often die in the care home so that’s something I’ve experienced quite a lot. There have been a few instances where people have suddenly become really unwell and been taken to hospital and died there.
It’s not as nice when you don’t really know what happened. You don’t know if their death was nice or not because they weren’t at home. And from what we hear, I don’t think it’s usually as peaceful as it is when they die in the care home, in their home.
Q: What does giving someone a good death mean to you?
I think what really separates the really nice death experiences that I’ve had from the not so nice ones is just being able to have that personal element to it. When you’re able to do all you can to make sure they’re happy and comfortable in their last moments.
An expected death makes it a lot easier to make sure it’s a nice one. But even when it’s unexpected, I think it’s about the resident having everything they need in place, such as their medications – so they remain peaceful and not too distressed.
It’s also having people they know around them. It makes a huge difference when staff who’ve known the residents for years can be with them as they die, and can put like their favourite music on or sit and just have a chat about things if they’re still able to talk. We’re quite lucky that we have quite a low staff turnover. A lot of our staff have been there for 10 years or more.
A not so nice death would be obviously if they didn’t have all their medication in place to support them, because I think the worst thing is when a resident gets really distressed and there’s nothing you can do about it. But also, if they’ve never met the person who’s with them, and if they didn’t know their likes and preferences. If they weren’t able to sit and have a chat with them and support them in their weakest moments.
Thinking about that person as a human being who needs connection, just as we are all human and seek and build those relationships. It’s very special to be there when someone’s dying, but when you feel uncertain, unsure or like something’s not right for them, it can be very hard.
Complete Article ↪HERE↩!