Americans are living longer with heart disease, managing it as a chronic condition. But there are few rules for these patients as they near the end of life.
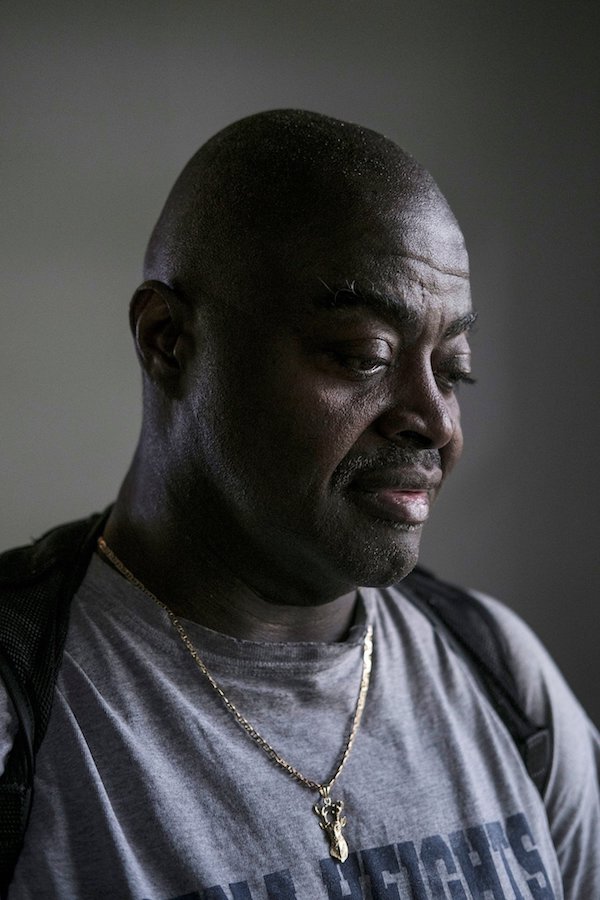
[R]icky Hurst’s doctors told him last year that there was nothing more they could do. His heart was failing and he should get his affairs in order. The end was coming.
His family gathered. He spoke to his pastor and resigned himself to death. “If it was meant to be, it was meant to be,” he said.
But. Mr. Hurst, 56, a former ranger and school football coach in Jackson, Mich., is still alive, although his heart continues to weaken. And patients like him are raising a new dilemma for doctors.
Heart disease once killed ruthlessly and quickly; patients like Mr. Hurst succumbed to heart attacks and sudden death from cardiac arrest. But with improved medical care and implanted devices that bolster the heart, a growing number of heart patients survive for years, even decades, coping with a chronic, progressive condition punctuated by crises and hospitalizations.
Their disease at that point is called heart failure — their weakened heart cannot pump enough blood to supply the body’s needs. The number of Americans with heart failure increased to 6.5 million in 2011-2014 from 5.7 million in 2009-2012, according to the American Heart Association.
More than 10 percent of those over age 80 have heart failure, and more patients are living longer with advanced disease. Even as the death rate from heart attacks is falling, the figure for heart failure is rising.
Yet there are no widely accepted guidelines for dealing with these patients as they near death. Cancer specialists regularly move their patients to hospice at the end of life, for instance, but few cardiologists even think of it. Heart patients account for just 15 percent of hospice deaths, while cancer patients make up half, according to a recent study.

That paper, published in the Journal of the American College of Cardiology, reviewed a number of ways in which heart patients are let down at the end of life. Implanted defibrillators often remain activated until the very end, for example, even for those in hospice.
A fifth of heart patients with defibrillators get shocked by them in the last few weeks of life, and 8 percent get shocked minutes before dying. Most patients are never told that they can ask that the defibrillators be turned off.
“Getting shocks at the end of life is not really helping patients live longer or better,” said Dr. Larry Allen, a heart failure specialist at the University of Colorado and an author of the study.
“We shouldn’t have a single one of these cases happening,” said Dr. Haider Warraich, a cardiology fellow at Duke University and first author of the study.
Experts often focus on the strides made in preventing and treating heart disease. Its incidence has declined by 70 percent in the past 50 years. People have heart attacks later in life than they used to, are more likely to survive them, and often live for years afterward with few or no symptoms.
“We are very proud” of that progress, said Dr. Patrice Desvigne-Nickens, a medical officer at the National Heart, Lung and Blood Institute.
Still, she added, cardiologists and their patients should be discussing end-of-life options and palliative care earlier in the course of heart failure.
“Everyone is uncomfortable with end-of-life discussions,” she said. “The field of cancer may be ahead of us. We should learn from looking at their example.”
But cardiologists thrive on the dramatic saving of lives, said Dr. Michael Bristow, a cardiologist at the University of Colorado Denver. They devote their professional lives to rescuing patients having heart attacks and bringing them back from the brink.
End-of-life care is not typically their focus; neither do they spend much time pondering what some of their patients may experience in the future. “Those who go into cardiology are not necessarily ones who want to deal with death and dying,” Dr. Bristow said.
The very nature of end-stage heart failure makes it all the more difficult to prepare.
“Very few patients understand the trajectory of the disease,” said Dr. Lynne Warner Stevenson, a heart failure specialist at Vanderbilt University. The path has peaks and valleys, but as the patient declines, each peak is a little lower than the one before.
And often doctors do not tell patients what to expect.
“Unfortunately, when you have patients with a chronic illness like heart failure, everyone thinks someone else will talk about it,” Dr. Stevenson said. “Too often, no one takes ownership of the last stage of the journey with the patient.”
Dr. Ellen Hummel of the University of Michigan, one of a small number of doctors specializing in cardiology palliative care, said the typical patient with cancer will usually experience a “fairly predictable” decline.
“They will be less able to take care of themselves,” she said. “They will be more symptomatic and come back to the hospital more frequently. And once this starts, it will probably continue until they die. Most people can see the end coming.”
But patients with end-stage heart failure are more likely to have wild swings, Dr. Hummel said, veering from feeling better to being terribly ill.
“It is confusing to both the patient and provider. Are they actually dying, or can we rescue them from a particular episode of worsening?”
Dr. Harlan Krumholz, a cardiologist at Yale University, agreed: “The issue is knowing who is really at the end of life.” For patients with heart failure, seesawing between good periods and bad, it can be very difficult to make the call.
Dr. Allen recently discussed all this with a patient, Ed Harvey.
Mr. Harvey, 75, has an implanted defibrillator, and his heart is weakening, pumping progressively less blood. Dr. Allen gave him medications that helped for a while, but, Dr. Allen said, “we have maxed out on what can be done.”
He can’t say with any certainty how long Mr. Harvey has. But now is the time, Dr. Allen told him, to talk about the end of life.
Mr. Harvey still feels pretty good, but “when you have congestive heart failure and it is not getting any better, you know that day is going to come,” he said.
He has been living with heart failure for more than a decade, and fears becoming a burden as his heart gets worse. It is now so weak that the only medical option left is an implantable pump. He knows that soon he will need full-time care.
“I have elected that if it got to that point,” he said, “put me in a hospice and let me go.”
Complete Article ↪HERE↩!