— Easier said than done
By Michael Cook
The central goal of right-to-die organisations has not changed much over the past 150 years. In 1872 a British writer, Samuel D. Williams, wrote a book advocating the use of the novel anaesthetic chloroform to give patients “a quick and painless death”. In 1931 the British eugenicist Dr Killick Millard proposed legalisation of euthanasia “to substitute for the slow and painful death a quick and painless one”.
Now that legalisation has arrived, however, doctors have realised that a Q&P death is easier said than done.
Writing in a recent issue of The Spectator (UK) Dr Joel Zivot, a Georgia physician, expresses his doubts about whether lethal medications are the way forward. He studied the autopsy reports of more than 200 prisoners executed with lethal injections and found that many may have died in great pain.
“The death penalty is not the same as assisted dying, of course. Executions are meant to be punishment; euthanasia is about relief from suffering. Yet for both euthanasia and executions, paralytic drugs are used. These drugs, given in high enough doses, mean that a patient cannot move a muscle, cannot express any outward or visible sign of pain. But that doesn’t mean that he or she is free from suffering.”
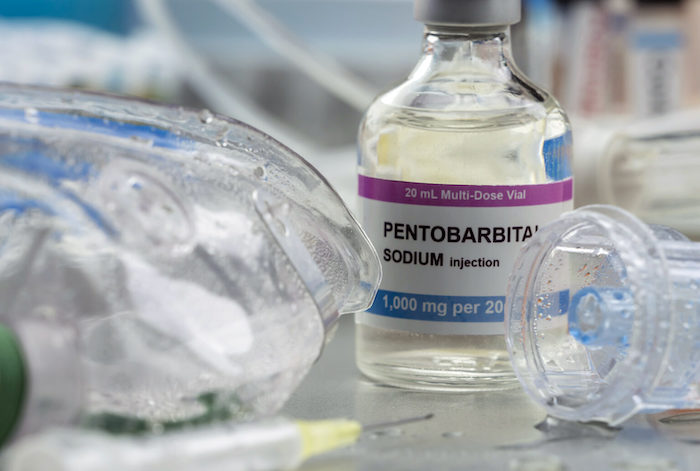
Dr Zivot believes that pentobarbital, which, it seems, is used in Oregon in 4 out of 5 assisted suicides, caused pulmonary oedema – the lungs fill with liquid secretions and the person can die in agony. “Advocates of assisted dying owe a duty to the public to be truthful about the details of killing and dying. People who want to die deserve to know that they may end up drowning, not just falling asleep,” he writes.
Nor is death necessarily quick.
In Oregon, where statistics are gathered about the mode of death, the median time to death throughout the 23 years of the Act is 30 minutes but the maximum time is 4 days and 8 hours. The median time for people to fall unconscious is 5 minutes, the maximum is 6 hours.
At least in the United States, doctors who participate in assisted suicides are aware of these issues. Dr Lonny Shavelson, a California physician who specialises in this novel field, has helped to organise the American Clinicians Academy on Medical Aid in Dying. This provides a forum for doctors to establish a best-practice for helping people to die.
It turns out that the very diseases from which the patients suffer can make the drugs less effective. Dr Shavelson spoke with Medical Xpress last year about some of the difficulties:
“Shavelson and [his colleague retired anesthesiologist Dr Carol] Parrot have identified which patients are more likely to linger, and can recommend adjustments. People with gastrointestinal cancer, for example, don’t absorb the drugs as well. Former opiate users often have resistance to some of the drugs. Young people and athletes tend to have stronger hearts and can survive longer with low respiration rates.
“We’re learning. Hypothesis, data and confirmation. This is what science is,” he said. “Our job is to stop the heart; that’s what they want us to do.”
Complete Article ↪HERE↩!
