
Enhancing Life Near Death

Legislation that would have allowed terminally ill patients to legally end their lives in California stalled Tuesday amid fierce opposition from religious groups.
The authors of the right-to-die bill did not present the legislation to the Assembly Health Committee as scheduled because it did not have enough votes to advance.
The panel includes multiple Democratic lawmakers from heavily Catholic districts in the Los Angeles area, where the archdiocese actively opposed the legislation.
“We continue to work with Assembly members to ensure they are comfortable with the bill,” Democratic Sens. Bill Monning of Carmel and Lois Wolk of Davis, and Assemblywoman Susan Eggman of Stockton said in a joint statement. “We remain committed to passing the End of Life Option Act for all Californians who want and need the option of medical aid in dying.”
Christian Burkin, a spokesman for Eggman, said the bill could not meet the deadline to pass committees this year while lawmakers remained uncomfortable with the bill.
Religious groups say allowing doctors to prescribe life-ending drugs is assisted suicide and goes against God’s will. Religious opposition helped defeat similar legislation in California in 2007.
Montana, Oregon, Vermont and Washington have court decisions or laws permitting doctors to prescribe life-ending drugs. A court ruling is pending in New Mexico.
Aid-in-dying advocates hoped the tide would turn after national publicity surrounding 29-year-old Brittany Maynard, who moved from California to Oregon to legally end her life in November following a diagnosis of terminal brain cancer.
In widely viewed videos and national media appearances, she said she deserved to get life-ending drugs in her home state of California. Maynard’s family members advocated for the right-to-die bill in Sacramento after her death.
The bill had advanced out of the state Senate on a mostly party-line vote, with Democrats in support and Republicans opposed.
California’s bill was modeled on Oregon’s law, which has been used in more than 750 deaths since voters approved it in 1994. Advocates for people with disabilities say terminally ill patients could be pressured to end their lives to avoid burdening their families.
The California Medical Association had dropped its decades-long opposition to aid-in-dying legislation, saying the decision should be left up to individual doctors if they want to help patients end their lives.
Legislatures in Maine and Colorado have rejected right-to-die bills this year. Similar efforts have stalled in other states.
Complete Article HERE!
When the California Medical Association removed its long-standing objection to assisted death in May, it seemed to clear a legislative path for Senate Bill 128, which would allow physicians to provide lethal drugs to patients with less than six months to live.
But the powerful doctors group’s neutral position has not quelled the controversy, either among lawmakers or in the medical community. After passing the state Senate last month, SB 128 could meet its end during a hearing Tuesday in the Assembly Health Committee, where it stalled two weeks ago over growing objections from Latino Democrats.
Nearly 18 years after Oregon enacted the country’s first assisted-death law, doctors also remain strongly divided over the ethics of the policy. Does it provide patients with a personal choice to end their suffering, or violate a physician’s oath to do no harm? The answer can be deeply personal.
Dr. Michael Amster, a pain-management specialist in Fairfield, deals with dying patients every day.
But he was unfamiliar with assisted death before last year, when a college friend who lived in Oregon came to the end of a debilitating two-year battle with gynecological cancer. As his friend considered taking advantage of the state’s law, Amster said she found a “peace of mind knowing that she could end her suffering if it got too unbearable.”
“She shared that, because of that, she was able to live her life more fully in the present moment and not worry about the future and the unknowns,” Amster said. Though his friend died too quickly to use Oregon’s law, “watching what she went through woke me up to understanding the value of having this option available in the end-of-life process.”
Amster has since become an advocate for assisted death in California, urging lawmakers to pass SB 128. He sees it as an issue of personal choice and autonomy in health care, rather than as physicians assisting patients to commit suicide, as some opponents have framed it.
“All it does is hasten a natural process,” he said.
Opponents have pointed to existing palliative care and pain management options as better ways to help dying patients in their final days. But Amster said available medications don’t work for everyone or can provide a poor quality of life, leaving people delirious and sedated.
He draws a contrast between sick animals, who are put down when their suffering becomes too great, and people, who are left to ride out the natural course of their dying process until their bodies finally shut down.
“We treat our pets better than we treat our loved ones, is what it comes down to,” he said. “There needs to be another option for people that are really stuck and suffering greatly.”
If SB 128 becomes law, Amster would be open to prescribing the medication. He said he already has those conversations with patients who come to him seeking help in dying, but he has to be “clear with them the boundaries” about what is legal.
That hit home last year as another friend of Amster’s in Davis was dying of ovarian cancer. She explored the possibility of moving to Oregon, but didn’t have enough time left to establish residency, so she began to talk about ending her own life in a “ritual” surrounded by loved ones.
“I watched my friend and her husband horrified and scared about, you know, if she chose to take all of her hospice medication and overdose and die, like, could he be thrown in jail if he knew about this?” Amster said.
When his friend began consulting Amster about how she might overdose, he said he had to make the difficult decision to distance himself.
“As a friend and someone who loved her, I wanted to help her end her suffering,” he said. “But ethically and with my license and what I felt what was the right thing, there was nothing I could do to help her.”
Amster hopes that legalizing assisted death in California will bring those conversations about dying into the open, and get people thinking about their own wishes.
“What are our values? What do we consider humane treatment for someone who’s at the end of their life?” he said. “Is that really suicide, or is that compassion?”
Dr. Daniel Mirda, a hematology and oncology specialist in Napa, tries to take the fear out of cancer treatment.
“I can’t tell you how many times a person comes to me and they’re very afraid of their illness and they’re facing a lot of possible disasters,” he said. “Yet oftentimes having a plan simplifies their life, helps them deal with it and better understand what to do.”
He takes the same approach with SB 128, which he has testified against as president of the Association of Northern California Oncologists.
While Mirda understands why someone facing a lethal and debilitating illness might want to “head it off at the pass,” he sees his role as providing patients with the best options possible for living their “most productive life” going forward.
“I don’t think in the same sitting I can tell you how to fight your cancer and this is how you end the fight,” he said.
Mirda shares some of the ethical concerns that other opponents of assisted death have expressed: Would the socioeconomically challenged be more likely to choose this option because medical therapies are too expensive? How much sway would a patient’s family have over their decision? Would it be overused?
He also objects to cutting short the process of dying, which he believes can be an important time for patients and their families.
“When you first find out you have an illness, the last thing you want to do is kill yourself,” Mirda said. Then as time goes on and people deal with the consequences, they can assess their quality of life and decide whether to keep seeking treatment.
“This idea of getting ready for death is sometimes as valuable to people as doing therapy to avoid it,” he said. “How are you going to spend that time that you have left?”
For loved ones, there’s a chance to say goodbye.
Mirda’s mother-in-law died from acute leukemia last month. At first, he said, the family wanted her to live longer. But as she developed various complications from the cancer, everyone was integrated into her struggle and eventually understood that she could no longer keep fighting it.
He compares it to his father’s sudden death many years ago, which left him in the lurch. When his mother-in-law finally died, the family was “kind of at peace.”
“You have done everything possible to help this individual,” he said. “There are no regrets at all.”
Mirda would rather that California focus on improving hospice care, which he regards as a “totally supportive environment” for both dying patients and those they are leaving behind.
“That to me is really where the real effort would have to be exerted – respecting the individual, but then respecting who this is going to affect that moves on,” he said.
If lawmakers pass SB 128, however, Mirda said he would at least make sure that his patients are informed of their options and free to choose for themselves. Whether he could prescribe the medication himself may depend on his relationship with the patient who asks.
“Could I do that if faced with it? We’ll have to see,” he said. “It would almost have to be as individual as the decision itself.”
Complete Article HERE!
I was 25 when I flew home for my father’s last birthday. His cancer had returned and he would die three months later at the age of 57. What I remember most about that weekend was the large rectangular gift box he opened. My mother had bought him a new suitcase.

I don’t know if that suitcase qualifies my family for the Denial Hall of Fame. There are so many contenders for that honor. But I’ve carried the psychic baggage over the years. I have never forgotten that image and how we lost a chance to say goodbye. I still wonder if my father was lonely in the silence that surrounded our inability to talk about what we all knew.
Decades later my mother began a long slow decline. By then, I was a newspaper columnist, a job that I often described as “telling people what you think.” I was professionally outspoken. But little had changed since my father’s death.
Yes, my mother and I talked about everything — but we didn’t talk about how she wanted to live toward the end. The closest we ever came to discussing her wishes was when she would see someone in dire straits and say, “If I’m ever like that, pull the plug.” But most of the time there is no plug to pull.
Gradually and painfully, my mother lost what the doctors call “executive function,” as if she were a C.E.O. fumbling with Excel spreadsheets, not a 92-year-old who couldn’t turn on the television or make a phone call. Eventually, she couldn’t decide what she wanted for lunch, let alone for medical care.
In some recess of my mind, I still assumed that death came in the way we used to think of as “natural.” I thought that doctors were the ones who would tell us what needed to be done. I was strangely unprepared, blindsided by the cascading number of decisions that fell to me in her last years.
I had to say no to one procedure and yes to another, no to the bone marrow test, yes and yes again to antibiotics. How often I wished I could hear her voice in my ear telling me what she wanted. And what she didn’t want.
When my mother died from heart failure and dementia, I began to talk with others. It was extraordinary. Everyone seemed to have a piercing memory of a good death or a hard death. Some of these stories had been kept below the surface for decades, and yet were as deep and vivid as if they’d just happened.
Too many people we love had not died in the way they would choose. Too many survivors were left feeling depressed, guilty, uncertain whether they’d done the right thing.
The difference between a good death and a hard death often seemed to hinge essentially on whether someone’s wishes were expressed and respected. Whether they’d had a conversation about how they wanted to live toward the end.
So, a small group of us — each with his or her own story — started the Conversation Project, a nonprofit, out of the belief that surely we could make this easier. Our partners at the Institute for Healthcare Improvement gathered experts frustrated at the pace of change who believed that the health care system wouldn’t change until the culture changed. So we are trying to change the culture.
There is now, finally, a real momentum for improving end-of-life care. The signs range from the Institute of Medicine’s report, “Dying in America,” to the success of Atul Gawande’s book “Being Mortal.”
There is also a growing public awareness of the need to break through the reluctance that has kept us tongue-tied for so long. A survey we did last year showed that 90 percent of Americans now think it’s important to have the conversation. But the same survey showed something else: Only 30 percent of us have actually had these conversations. So the gap remains huge.
We still need to transform the cultural norm from not talking about how we want to live at the end of life to talking about it. The real work to close the gap is not just for doctors and patients. It’s for mothers and daughters, husbands and wives, families and friends. We have to bring people to the kitchen table to talk with those they love to have the conversation. And to do this before there is a crisis. Not in the I.C.U.
In our survey, the primary reason people gave for not talking to their loved ones was “It’s too soon.” But it’s always too soon … until it’s too late. Half of all elderly people in hospitals cannot make decisions for themselves at the end of life. Far too many health care providers are uncomfortable and untrained in these conversations.
From all the stories shared with us, we know that what people need most is help getting started. They need a travel guide to take the first steps down an unfamiliar and difficult road. So we created a Conversation Starter Kit, which deliberately avoids being a technical medical checklist for the dying in favor of a careful discussion guide for the living.
Our starter kit asks what matters to you, not what’s the matter with you. It asks what’s most important to you in the last phase of your life? Who do you want to make decisions for you? Where do you want to be? Do you worry that you won’t get enough care? Do you worry that you’ll get overly aggressive care?
About two-thirds of the nearly 300,000 people who have come to our website download the starter kit, which is free. We’ve been told repeatedly that conversations that had loomed as frightening and overwhelming repeatedly turned into the most intimate and rewarding moments.
Is it important to have the health care system ready to respect and record our wishes, to have health care providers become more comfortable beginning these talks? Of course. But the hard truth is that we have to begin ourselves — by thinking about our own values, by sharing them, by bringing our own beliefs into the center of the room when decisions will be made.
In my own adulthood, the culture of birth changed. It wasn’t doctors who first tossed out the stirrups and ushered in fathers and video cameras and “birthing rooms.” It was parents who said, birth is not just a medical experience, it’s a human experience. Now we are finally saying that dying, too, is not just a medical experience, it is also a deeply human experience.
Last winter we held a national dinner party to break bread and taboos, to eat comfort food and talk about dying. I shared the table with Nancy Frates, who is known for starting the A.L.S. ice bucket challenge to honor her son Pete. “Now I understand,” she told me. “The conversation is a gift to your family.”
When I helped found the Conversation Project, I thought we were doing this for people who were dying. I thought of my parents. I thought of “executive function” and “baggage.” What I have learned is that the conversation is also a legacy. This is the gift, maybe the last gift, we can give one another.
Complete Article HERE!
BY KAREN OCAMB
In 1996, on the cusp of the lifesaving three-drug HIV cocktail, Eric Roberts starred inIt’s My Party by director Randal Kleiser, one of the first films to feature a gay man who not only insists on dying with dignity but doing so with a festive, emotional flare.
Roberts’ character had been diagnosed with an aggressive disease that would rob him of his mental acuity months before he would actually die, so he wants a goodbye party while he can still recognize the ones he loves. The film was Kleiser’s tribute to his own ex-lover, who died of AIDS in 1992.
In the film Roberts had a brain disease, so he still looked young, fit and beautiful. Most gays with AIDS surrendered vanity early on as their once-worshipped bodies were ravaged by the wasting syndrome or the purple lesions of Kaposi’s Sarcoma. They were rendered helpless and unrecognizable to themselves, an agony sometimes worse than the unrelenting physical pain. Death was a welcome blessing, and many were quietly helped to that end by bereft loving friends, lovers and family, despite the pall of illegality.
It was in this context that efforts to legalize physician-assisted suicide in California were launched in 1992, 1995 and 1999. But the prospect of a dying person choosing a good death became highly politicized by the religious right with the Florida case of Terri Schiavo, where Gov. Jeb Bush sided with the family and ordered her life prolonged, despite the wishes of her husband who said his wife expressly said she wouldn’t want to be kept alive in a vegetative state.
Today there is another effort underway in the California Legislature to pass a well-crafted bill—modeled on the successful death-with-dignity bill in Oregon—that even won the support of conservative Democrat U.S. Sen. Dianne Feinstein and the California Medical Association, which ended its opposition after 28 years. On June 4, the State Senate passed the End of Life Option Act, SB 128, by 23 to 14, buoyed by a poll last year showing that nearly two-thirds of Californians favor giving a terminally ill patient the option to die peacefully. Currently Washington, Montana, Vermont and New Mexico also have medical-aid-in-dying laws.
Co-authors Senate Majority Leader Bill Monning and Senate Majority Whip Lois Wolk, with support from the Compassion & Choices Coalition, introduced SB 128 last January. The bill has a “checklist” of safeguards to prohibit the possibility of abuse. Essentially the bill would allow a mentally competent, terminally ill adult (18 or over) the option of requesting (both orally and in writing) a doctor’s prescription for medication to shorten the inevitable dying process so they might die peacefully, without pain.
“I’m doing everything I can to extend my life. No one should have the right to extend my death,” out State Sen. Mark Leno recalls one woman dying of lung cancer saying during a Senate hearing on the bill. Leno is a principal co-author of SB 128.
“I happen to be of the philosophical belief that government should not come between an individual and a decision he or she may make with a physician,” Leno says during a phone interview with Frontiers. “There is nothing more personal and of greater importance than our end-of-life choices. I don’t think government should be in the way. That’s what this bill does. It provides a choice for someone in a very specific situation.”
Leno knows something about this. He lost his partner Doug in 1990 and Doug’s younger brother in 1986. “Those of us of a certain age,” Leno says, “saw the tortured deaths of hundreds of friends” at a time when there was no hope of surviving. “So I’ve seen firsthand how cruel that can be.” And with aging parents and siblings approaching their last years, “it becomes a very real issue all over again.”
Leno says he found it “astounding” that a Republican colleague described his opposition to the bill by suggesting a terminally ill patient could drive over a cliff or shoot themselves in the temple instead. “The level of insensitivity is so extreme,” he says.
Michael Saum, a 35-year-old transgender man who is dying from brain cancer (pictured in photo above with best friend Julia), wishes he had that option. Saum’s doctors think he will die in the next few months, before the bill reaches Gov. Jerry Brown’s desk.
“It’s not that I want to die; I don’t want to die,” Michael tells Frontiers. “I love life, but I don’t want to live like this.”
Saum was battling cancer for 14 years before going into remission—an 18-month respite during which he took the opportunity to become the man he always felt himself to be. His mother, who had been fine when then-Heidi came out as a lesbian, could not handle his transition. When he was diagnosed with Stage IV brain cancer that had spread throughout his body, he turned to his lesbian friends, most importantly his best friend Julia, whom he had once dated, to provide him refuge in her El Monte home and to take care of him. “It’s the kind of love I can’t even describe. She’s selfless,” he says.
Saum is currently at the strongest dose of painkiller allowed, but it’s not working. He has severe headaches, nausea, unregulated body temperature, short-term memory loss, unfiltered speech—“so many things go wrong” having big tumors in both the left and right frontal lobes.
“I’m in terrible pain every day, to the point that I’m crying nearly every day,” he says. “I’ve been told by my doctor that there is no chance for change, no miracle; no treatment is going to heal me.
“I think I’m going to pass before this bill is enacted,” Saum says, “but if it’s not there for me, I’m grateful I’m able to help others in my situation.”
Out Assemblymember Susan Eggman, Chair of the LGBT Legislative Caucus, is the lead principal co-author in the Assembly. A former hospice social worker who also lost friends in the ‘80s and ‘90s and cared for family members as they lay dying, she is uniquely positioned to understand the significance of SB 128.
“I come at this from a lot of different perspectives,” Eggman tells Frontiers. I believe—and I think polling shows—that Californians are ready for this.” Additionally, 17 years of research out of Oregon show that there is virtually no coercion or abuse.
“We know that oftentimes people don’t even go through with it. They just know that they have that option,” Eggman says. The bill is not for people who are depressed or seniors or disabled. “This is for somebody with a terminal illness, for which no cure is expected, and their end-of-life trajectory is within six months to a year.”
And, she notes, the End of Life Option Act is “for those who have had a certain degree of control in their life—this is something that is important to them.”
Perhaps more people than the dying and their loves ones are beginning to grasp the moral and ethical urgency of this bill. In a sharp contrast to the political and religious-based Schiavo controversy, a bipartisan poll conducted June 16-21 shows that nearly seven out of 10 Californians (69%) support SB 128, and that includes Catholics (60%), non-evangelical Protestants (65%) and evangelical Christians (57%).
Eggman is holding a hearing on the bill on July 7. The deadline to pass SB 128 in the Assembly is September 11.
Complete Article HERE!
“I am a widower.”
Those are four words I never imagined myself saying at my age. Maybe at 70 or 80. Mid-60s, if something terrible, like a plane crash or a terrorist attack, took one of us. Or never, if I was the first to go.
None of those scenarios took place.
I lost my partner, Gary Lussier, to liver disease two years ago. He was a wonderful man — a former dancer, handsome with a wicked sense of humor and a way of embracing the world that would shame most people. He didn’t get to embrace the world for long enough, though. He was 52 and I was 53 on the day I walked out of NY Presbyterian Hospital/Cornell Medical Center, dazed, confused and alone.
He died less than 24 hours before he might have had a successful liver transplant, slightly more than three days after I rushed him to the hospital, over a year since his illness began to manifest itself and about a quarter-century since we had joined our lives. Even though I was well past 50, I found myself in the “he’s too young for this to happen” category.

And, of course, there was another complication: I was not married to Gary, even though we had been together 24.5 years. Though we had no legal document, ours was as true a union as any other. Emotionally supported by our two good families and a phalanx of friends, having the benefit of treatment in New York City’s best hospital and embraced by the staff of my company, St. Martin’s Press, I had the rare luxury of being able to consider my place in the world free from legal battles and financial concerns that can be real, threatening and, occasionally, life-shattering for the one left behind.
In the days after his death I began to ask myself, “What am I now?” I was no longer “partner.” I searched and searched for a word that defined me. Finally, I settled on the most obvious and yet, for me, most problematic word: widower. In choosing it I set myself the task of understanding its meaning.
I was also trying to find the courage to say it out loud.
Of course, “widower” implies “marriage,” “husband,” “deceased wife” and — in our world — “heterosexual.” We weren’t married. We referred to each other as “partners.” I am gay. The first time I said it out loud — “I am a widower” — I was alone in my apartment. The silence was so loud it threatened to crush me.
When that sentence broke the isolation I’d been living in. I knew I had found a word that would take me forward, but one that would provoke surprise in others. “Did he say ‘widower’?” I imagined people thinking to themselves at cocktail parties. “I didn’t know they were married…” they might say, in private, when they took off their pearls or undid their ties. Worse might come from hate mongers I didn’t even know. The question obsessed me: How could I call myself “Gary’s widower” and be true about it?
For me, the ability to say “widower” came down to the question of what the word “marriage” means. We’ve all been taught “marriage” refers to the moment when two people profess vows of love before a governmental or religious authority, rings are exchanged, documents are signed and the couple runs off to Happily Ever After. They are “married.”
There is, though, a deeper meaning, I think, of the verb “to marry,” a more private one concerning itself less with ceremony and legality than with the intimacy and commitment between two people: “to take as an intimate life partner by a formal exchange of promises in the manner of a traditional marriage ceremony.” Had Gary and I done that over the years? Did we have some formal exchange of promises?
Stephen Sondheim has a song about marriage describing it as “…the little things you do together…” We certainly had our fill of them throughout the years: Not just Thanksgivings and Christmases and Easters or trips abroad or weeks on the Ogunquit beach. No, we had more than that. We had almost a quarter century of eating pizza while watching television, having dinners with friends, arguing about how best to do the laundry, having a bang-up row in public, commiserating over each other’s daily work woes and celebrating each other’s triumphs. So, in that way, we did indeed have a marriage. Through millions of small acts, private and public, we were intimate life partners.
But, did we have a “formal exchange of promises” I wondered? Over the years, every night, we said “I love you” to each other before falling asleep. Were those not exchanges of a mutual promise renewed each day? I think they were. But, were they enough to pronounce us “married”? Did we have some deeper and more formal promise? In looking back, we did, though no clergy or justice of the peace was present.
We met when a legal marriage between two men was unthinkable. We also heard the revolutionary roar of “We’ll live together unmarried!” from both straight and gay couples. Now that marriage was actually possible, I had begun to think about how wonderful it would be to have a “husband,” someone to call my own, someone defined by a word that could not be mistaken for a business associate: “husband,” not “partner.” Just thinking of those words made me feel different: stronger, safer and — in a corny way — a man-in-love.
When the New York State gay marriage law was finally passed in 2011, we were at our house in Massachusetts where gay marriage was already legal. It was a beautiful day and we were in the garden, weeding. Gary seemed to be on the mend after his initial diagnosis and treatment. I had felt a strong “are we going to get married?” vibe from him since we heard the news. There in the garden, down on one knee as I was weeding around the boxwoods, I said, “Gary, will you marry me?” He was shocked. So was I. He said, in a typically Gary way, “Well, I don’t see a ring…” And, then, to my surprise, he said “No … not until you get me a ring …” as much with shock that I had asked as he was by the need to answer. I was crushed. I had never asked anyone to marry me before, but there it was. “No.”
Not long after that day, Gary began to spiral downward again and the incident was pushed aside by multiple hospital stays, the imperfect weekly calculation of his place on the liver transplant list, the day-to-day monitoring of weight, at-home visits from medical workers, frantic expeditions to specialty pharmacies and, most wrenchingly, the ups-and-downs of watching the person you love most in the world become increasingly and dangerously ill.
My marriage proposal remained buried in our garden until about an hour before Gary began to die. He was in the ICU, his liver failing (unbeknownst to me). He was drifting in and out of consciousness. During one lucid moment, he grabbed my hand, pulled me to him, eyes wide-open staring straight into mine, and said, “I do!” with such vehemence that it startled me.
I was speechless; but, since I was his chief cheerleader on the road to transplant, I said “Oh, no you don’t… we’ll do this right once you get your liver …” He laughed a little. If God or The Idea of God has to do with love, I like to think that He or She was present when that vow was made because, if true love has ever made itself manifest, it was in that moment. We finally had our formal ceremony and I clasped his hands tightly. An hour later, the massive hemorrhage that ended his life began and he lost all consciousness. Months later, I told a friend that I wished I’d said “I do, too!” and he said, “You did, on that day in your garden.”
I now understand that we were, indeed, married in so many ways that I have come to say, “I am a widower” with confidence, if with little joy. It’s not a nice thing to have to say. It puts people off, or — even worse — makes them want to take care of you when you least need it. That statement’s message is “I lost my spouse, but I am still alive. I’m standing on my own two feet and intend to go on living for as long as I can.” It means you freely have given a significant part of your life to someone who is now gone and that you are alone. It means, “I remain while he has moved on.” It also now, thankfully, has less relationship to gender preference. As Wendy Wasserstein wrote: “Love is love. Gender is just spare parts.”
How, then, do you say, “I am a widower”? It has nothing to do with age. Young or old, you say it plainly, like saying “armor,” knowing that nothing else can ever hurt you as much as your spouse’s death. You say it in the full knowledge that the union you had with your deceased spouse was as deep and as rich and as true as any other. You say it with remembrance and, most of all, you say it with love and pride for the spouse who has passed on — that singular, unforgettable human being who taught you, truly, how to love and to be loved.
“I am a widower.”
Complete Article HERE!
By Rochelle Rietow

So, you’re a funeral professional, and you’ve got a pretty good idea of what makes your products and services valuable to your families. And if you’re really good at what you do, you’ve probably memorized the value statements for all of your products and know how to pitch your families on just about everything.
But did you know that there are valuable products out there that can actually inspire and help your families, even when you’re not around? For example, funeral products that can bring light to the darkness, not just for family, but for friends and loved ones all over the world. This is something I’ve spent some time thinking about, particularly when it comes to the value behind social memorial pages.
Since releasing our own social memorial websites over a decade ago, I’ve spent a great deal of time observing the true meaning and value that they bring to families – both during and after the funeral service. I’ve seen them turned into books that families keep on their coffee table. Heck, I’ve even seen them printed and kept on people’s desks as a reminder that they can get through their grief. And through all of these observations, I’ve come up with a few foundational ways that social memorial websites have added value to families’ lives over the years, and ways they can add value to yours, too.
If you’ve ever lost someone, you may have had an experience like this before: You’re doing something that reminds you of your loved one and really want to tell them about it, but you can’t… who do you share it with? That’s where social memorial websites come in. They give you a space to write these thoughts, experiences and messages down. And when it comes to grieving, we all know the only way to heal is to speak your heart.
Another great feature of social memorial pages? People will see the message you wrote to your loved one and recognize it, respond to it, or maybe even share a new memory that they, themselves, created with your loved one. And they will be able to do this on your website for days, weeks, and even years to come, as f1Connect’s social memorial pages are hosted online forever. After all, the healing process is never really over, and we believe your family should be able to always come back to their loved one’s memorial page to reflect and share memories whenever they need to. It’s an ongoing conversation, and a really important one.
While going through a few social memorial websites, I read a message that someone wrote on their co-worker’s social memorial page when they heard the news of his passing. Once they came across the memorial page, they decided to share their own story of the co-worker, and what he meant to them. This gave the loved one’s mother, Cindi, a glimpse into a new story about her son that she had never heard before.
The situation might not have played out like this if it had happened any other way, or on any other platform. The co-worker may have been alone in his grief, because he wouldn’t have had this healing outlet to share his story and he may not have known about the funeral. And the mother may have never heard the heart-warming, caring story about her son if his co-worker wouldn’t have shared his sympathy online.
Social memorial pages allow us to do things a bit differently than we did before. Maybe we can even grieve in a more complete way because we have access to more memories, more people, and more support. In this case, I think it’s especially true.
One of the biggest advantages of a social memorial page is that they allow family and friends to share their own stories and memories of how a loved one affected their lives. This process is not only healing for the people who are sharing these moments, but also for the family of the loved one who may be hearing these stories for the first time. After all, it’s powerful to read just how many lives have been touched and changed just from the impact of one person.
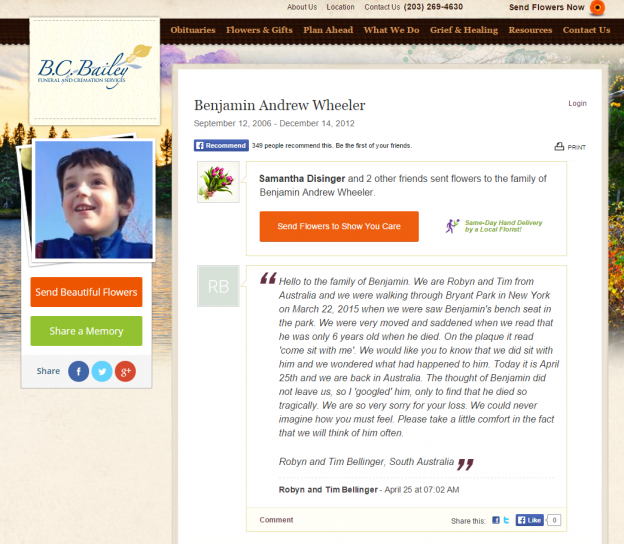
One great example of this is the social memorial page for Benjamin Wheeler, a six-year-old who passed away in the Sandy Hook Elementary School tragedy that made national headlines. Even though his death occurred back in 2012, many people are still leaving stories and memories of how his life and his story have touched them on his social memorial page.
Just read the following message written on Benjamin’s social memorial page, from a family in Australia who heard about Benjamin’s tale and felt compelled to share their own story with those closest to him.
I’ll never forget the day that one of funeralOne’s employees ran up to me in tears and said, “Come quick, you have to see this!” She just witnessed a powerful moment that, through a twist of fate, could have only happened because of the existence of the social memorial websites our team created.
What had happened was, a man had been searching for a friend who he hadn’t seen in years (maybe even decades) and thought he had disappeared. After long hours spent on Google, he came across his friend’s social memorial page on a funeral home’s website. Finding out that his friend had passed away was sad news, but ultimately, it gave him closure to an unclosed chapter in his life. And through reading all the wonderful messages friends and family wrote on his tribute wall, he was able to feel close to his friend one last time.
This story goes to show that, when you introduce a new way to grieve and share memories, unexpected things will occur that help your families heal and remember, long after they step out of your funeral home.
As you can see, social memorial websites can play a pretty amazing part in families’ lives. And the great thing is, they’re only just beginning to change the way we deal with life, death and grief. In the future, social memorial websites could become an important, if not essential, part of our stages of grief. And with an ever-growing integration between our lives and technology, it’s pretty amazing to think about all the possibilities.
If you’d like to see the value of f1Connect’s social memorial websites first hand, be sure to click here and find out more about the website features your families are craving.
Complete Article HERE!