— ‘There’s something happening in the brain that makes no sense’

New research into the dying brain suggests the line between life and death may be less distinct than previously thought
By Alex Blasdel
Patient One was 24 years old and pregnant with her third child when she was taken off life support. It was 2014. A couple of years earlier, she had been diagnosed with a disorder that caused an irregular heartbeat, and during her two previous pregnancies she had suffered seizures and faintings. Four weeks into her third pregnancy, she collapsed on the floor of her home. Her mother, who was with her, called 911. By the time an ambulance arrived, Patient One had been unconscious for more than 10 minutes. Paramedics found that her heart had stopped.
After being driven to a hospital where she couldn’t be treated, Patient One was taken to the emergency department at the University of Michigan. There, medical staff had to shock her chest three times with a defibrillator before they could restart her heart. She was placed on an external ventilator and pacemaker, and transferred to the neurointensive care unit, where doctors monitored her brain activity. She was unresponsive to external stimuli, and had a massive swelling in her brain. After she lay in a deep coma for three days, her family decided it was best to take her off life support. It was at that point – after her oxygen was turned off and nurses pulled the breathing tube from her throat – that Patient One became one of the most intriguing scientific subjects in recent history.
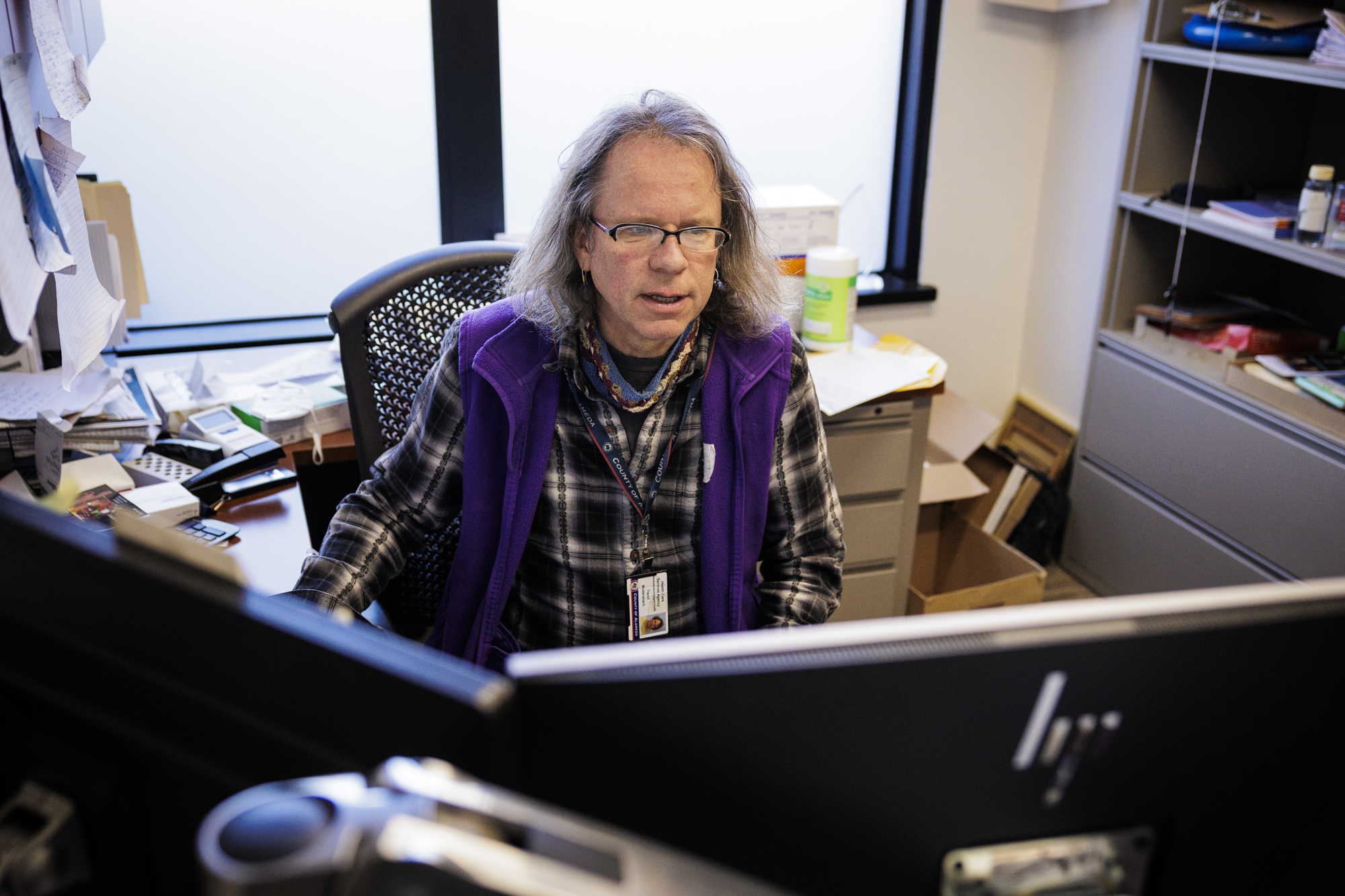
For several years, Jimo Borjigin, a professor of neurology at the University of Michigan, had been troubled by the question of what happens to us when we die. She had read about the near-death experiences of certain cardiac-arrest survivors who had undergone extraordinary psychic journeys before being resuscitated. Sometimes, these people reported travelling outside of their bodies towards overwhelming sources of light where they were greeted by dead relatives. Others spoke of coming to a new understanding of their lives, or encountering beings of profound goodness. Borjigin didn’t believe the content of those stories was true – she didn’t think the souls of dying people actually travelled to an afterworld – but she suspected something very real was happening in those patients’ brains. In her own laboratory, she had discovered that rats undergo a dramatic storm of many neurotransmitters, including serotonin and dopamine, after their hearts stop and their brains lose oxygen. She wondered if humans’ near-death experiences might spring from a similar phenomenon, and if it was occurring even in people who couldn’t be revived.
Dying seemed like such an important area of research – we all do it, after all – that Borjigin assumed other scientists had already developed a thorough understanding of what happens to the brain in the process of death. But when she looked at the scientific literature, she found little enlightenment. “To die is such an essential part of life,” she told me recently. “But we knew almost nothing about the dying brain.” So she decided to go back and figure out what had happened inside the brains of people who died at the University of Michigan neurointensive care unit. Among them was Patient One.
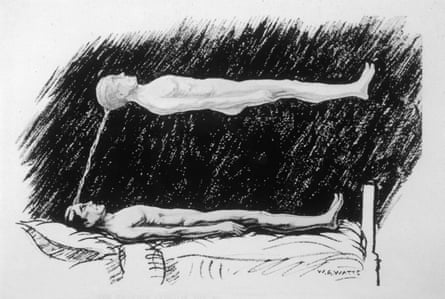
At the time Borjigin began her research into Patient One, the scientific understanding of death had reached an impasse. Since the 1960s, advances in resuscitation had helped to revive thousands of people who might otherwise have died. About 10% or 20% of those people brought with them stories of near-death experiences in which they felt their souls or selves departing from their bodies. A handful of those patients even claimed to witness, from above, doctors’ attempts to resuscitate them. According to several international surveys and studies, one in 10 people claims to have had a near-death experience involving cardiac arrest, or a similar experience in circumstances where they may have come close to death. That’s roughly 800 million souls worldwide who may have dipped a toe in the afterlife.
As remarkable as these near-death experiences sounded, they were consistent enough that some scientists began to believe there was truth to them: maybe people really did have minds or souls that existed separately from their living bodies. In the 1970s, a small network of cardiologists, psychiatrists, medical sociologists and social psychologists in North America and Europe began investigating whether near-death experiences proved that dying is not the end of being, and that consciousness can exist independently of the brain. The field of near-death studies was born.
Over the next 30 years, researchers collected thousands of case reports of people who had had near-death experiences. Meanwhile, new technologies and techniques were helping doctors revive more and more people who, in earlier periods of history, would have almost certainly been permanently deceased. “We are now at the point where we have both the tools and the means to scientifically answer the age-old question: What happens when we die?” wrote Sam Parnia, an accomplished resuscitation specialist and one of the world’s leading experts on near-death experiences, in 2006. Parnia himself was devising an international study to test whether patients could have conscious awareness even after they were found clinically dead.
But by 2015, experiments such as Parnia’s had yielded ambiguous results, and the field of near-death studies was not much closer to understanding death than it had been when it was founded four decades earlier. That’s when Borjigin, together with several colleagues, took the first close look at the record of electrical activity in the brain of Patient One after she was taken off life support. What they discovered – in results reported for the first time last year – was almost entirely unexpected, and has the potential to rewrite our understanding of death.
“I believe what we found is only the tip of a vast iceberg,” Borjigin told me. “What’s still beneath the surface is a full account of how dying actually takes place. Because there’s something happening in there, in the brain, that makes no sense.”
For all that science has learned about the workings of life, death remains among the most intractable of mysteries. “At times I have been tempted to believe that the creator has eternally intended this department of nature to remain baffling, to prompt our curiosities and hopes and suspicions all in equal measure,” the philosopher William James wrote in 1909.
The first time that the question Borjigin began asking in 2015 was posed – about what happens to the brain during death – was a quarter of a millennium earlier. Around 1740, a French military physician reviewed the case of a famous apothecary who, after a “malign fever” and several blood-lettings, fell unconscious and thought he had travelled to the Kingdom of the Blessed. The physician speculated that the apothecary’s experience had been caused by a surge of blood to the brain. But between that early report and the mid-20th century, scientific interest in near-death experiences remained sporadic.
In 1892, the Swiss climber and geologist Albert Heim collected the first systematic accounts of near-death experiences from 30 fellow climbers who had suffered near-fatal falls. In many cases, the climbers underwent a sudden review of their entire past, heard beautiful music, and “fell in a superbly blue heaven containing roseate cloudlets”, Heim wrote. “Then consciousness was painlessly extinguished, usually at the moment of impact.” There were a few more attempts to do research in the early 20th century, but little progress was made in understanding near-death experiences scientifically. Then, in 1975, an American medical student named Raymond Moody published a book called Life After Life.

In his book, Moody distilled the reports of 150 people who had had intense, life-altering experiences in the moments surrounding a cardiac arrest. Although the reports varied, he found that they often shared one or more common features or themes. The narrative arc of the most detailed of those reports – departing the body and travelling through a long tunnel, having an out-of-body experience, encountering spirits and a being of light, one’s whole life flashing before one’s eyes, and returning to the body from some outer limit – became so canonical that the art critic Robert Hughes could refer to it years later as “the familiar kitsch of near-death experience”. Moody’s book became an international bestseller.
In 1976, the New York Times reported on the burgeoning scientific interest in “life after death” and the “emerging field of thanatology”. The following year, Moody and several fellow thanatologists founded an organisation that became the International Association for Near-Death Studies. In 1981, they printed the inaugural issue of Vital Signs, a magazine for the general reader that was largely devoted to stories of near-death experiences. The following year they began producing the field’s first peer-reviewed journal, which became the Journal of Near-Death Studies. The field was growing, and taking on the trappings of scientific respectability. Reviewing its rise in 1988, the British Journal of Psychiatry captured the field’s animating spirit: “A grand hope has been expressed that, through NDE research, new insights can be gained into the ageless mystery of human mortality and its ultimate significance, and that, for the first time, empirical perspectives on the nature of death may be achieved.”
But near-death studies was already splitting into several schools of belief, whose tensions continue to this day. One influential camp was made up of spiritualists, some of them evangelical Christians, who were convinced that near-death experiences were genuine sojourns in the land of the dead and divine. As researchers, the spiritualists’ aim was to collect as many reports of near-death experience as possible, and to proselytise society about the reality of life after death. Moody was their most important spokesman; he eventually claimed to have had multiple past lives and built a “psychomanteum” in rural Alabama where people could attempt to summon the spirits of the dead by gazing into a dimly lit mirror.
The second, and largest, faction of near-death researchers were the parapsychologists, those interested in phenomena that seemed to undermine the scientific orthodoxy that the mind could not exist independently of the brain. These researchers, who were by and large trained scientists following well established research methods, tended to believe that near-death experiences offered evidence that consciousness could persist after the death of the individual. Many of them were physicians and psychiatrists who had been deeply affected after hearing the near-death stories of patients they had treated in the ICU. Their aim was to find ways to test their theories of consciousness empirically, and to turn near-death studies into a legitimate scientific endeavour.
Finally, there emerged the smallest contingent of near-death researchers, who could be labelled the physicalists. These were scientists, many of whom studied the brain, who were committed to a strictly biological account of near-death experiences. Like dreams, the physicalists argued, near-death experiences might reveal psychological truths, but they did so through hallucinatory fictions that emerged from the workings of the body and the brain. (Indeed, many of the states reported by near-death experiencers can apparently be achieved by taking a hero’s dose of ketamine.) Their basic premise was: no functioning brain means no consciousness, and certainly no life after death. Their task, which Borjigin took up in 2015, was to discover what was happening during near-death experiences on a fundamentally physical level.
Slowly, the spiritualists left the field of research for the loftier domains of Christian talk radio, and the parapsychologists and physicalists started bringing near-death studies closer to the scientific mainstream. Between 1975, when Moody published Life After Life, and 1984, only 17 articles in the PubMed database of scientific publications mentioned near-death experiences. In the following decade, there were 62. In the most recent 10-year span, there were 221. Those articles have appeared everywhere from the Canadian Urological Association Journal to the esteemed pages of The Lancet.
Today, there is a widespread sense throughout the community of near-death researchers that we are on the verge of great discoveries. Charlotte Martial, a neuroscientist at the University of Liège in Belgium who has done some of the best physicalist work on near-death experiences, hopes we will soon develop a new understanding of the relationship between the internal experience of consciousness and its outward manifestations, for example in coma patients. “We really are in a crucial moment where we have to disentangle consciousness from responsiveness, and maybe question every state that we consider unconscious,” she told me. Parnia, the resuscitation specialist, who studies the physical processes of dying but is also sympathetic to a parapsychological theory of consciousness, has a radically different take on what we are poised to find out. “I think in 50 or 100 years time we will have discovered the entity that is consciousness,” he told me. “It will be taken for granted that it wasn’t produced by the brain, and it doesn’t die when you die.”
If the field of near-death studies is at the threshold of new discoveries about consciousness and death, it is in large part because of a revolution in our ability to resuscitate people who have suffered cardiac arrest. Lance Becker has been a leader in resuscitation science for more than 30 years. As a young doctor attempting to revive people through CPR in the mid-1980s, senior physicians would often step in to declare patients dead. “At a certain point, they would just say, ‘OK, that’s enough. Let’s stop. This is unsuccessful. Time of death: 1.37pm,’” he recalled recently. “And that would be the last thing. And one of the things running through my head as a young doctor was, ‘Well, what really happened at 1.37?’”
In a medical setting, “clinical death” is said to occur at the moment the heart stops pumping blood, and the pulse stops. This is widely known as cardiac arrest. (It is different from a heart attack, in which there is a blockage in a heart that’s still pumping.) Loss of oxygen to the brain and other organs generally follows within seconds or minutes, although the complete cessation of activity in the heart and brain – which is often called “flatlining” or, in the case of the latter, “brain death” – may not occur for many minutes or even hours.
For almost all people at all times in history, cardiac arrest was basically the end of the line. That began to change in 1960, when the combination of mouth-to-mouth ventilation, chest compressions and external defibrillation known as cardiopulmonary resuscitation, or CPR, was formalised. Shortly thereafter, a massive campaign was launched to educate clinicians and the public on CPR’s basic techniques, and soon people were being revived in previously unthinkable, if still modest, numbers.
As more and more people were resuscitated, scientists learned that, even in its acute final stages, death is not a point, but a process. After cardiac arrest, blood and oxygen stop circulating through the body, cells begin to break down, and normal electrical activity in the brain gets disrupted. But the organs don’t fail irreversibly right away, and the brain doesn’t necessarily cease functioning altogether. There is often still the possibility of a return to life. In some cases, cell death can be stopped or significantly slowed, the heart can be restarted, and brain function can be restored. In other words, the process of death can be reversed.
It is no longer unheard of for people to be revived even six hours after being declared clinically dead. In 2011, Japanese doctors reported the case of a young woman who was found in a forest one morning after an overdose stopped her heart the previous night; using advanced technology to circulate blood and oxygen through her body, the doctors were able to revive her more than six hours later, and she was able to walk out of the hospital after three weeks of care. In 2019, a British woman named Audrey Schoeman who was caught in a snowstorm spent six hours in cardiac arrest before doctors brought her back to life with no evident brain damage.
“I don’t think there’s ever been a more exciting time for the field,” Becker told me. “We’re discovering new drugs, we’re discovering new devices, and we’re discovering new things about the brain.”
The brain – that’s the tricky part. In January 2021, as the Covid-19 pandemic was surging toward what would become its deadliest week on record, Netflix released a documentary series called Surviving Death. In the first episode, some of near-death studies’ most prominent parapsychologists presented the core of their arguments for why they believe near-death experiences show that consciousness exists independently of the brain. “When the heart stops, within 20 seconds or so, you get flatlining, which means no brain activity,” Bruce Greyson, an emeritus professor of psychiatry at the University of Virginia and one of the founding members of the International Association for Near-Death Studies, says in the documentary. “And yet,” he goes on to claim, “people have near-death experiences when they’ve been (quote) ‘flatlined’ for longer than that.”
That is a key tenet of the parapsychologists’ arguments: if there is consciousness without brain activity, then consciousness must dwell somewhere beyond the brain. Some of the parapsychologists speculate that it is a “non-local” force that pervades the universe, like electromagnetism. This force is received by the brain, but is not generated by it, the way a television receives a broadcast.
In order for this argument to hold, something else has to be true: near-death experiences have to happen during death, after the brain shuts down. To prove this, parapsychologists point to a number of rare but astounding cases known as “veridical” near-death experiences, in which patients seem to report details from the operating room that they might have known only if they had conscious awareness during the time that they were clinically dead. Dozens of such reports exist. One of the most famous is about a woman who apparently travelled so far outside her body that she was able to spot a shoe on a window ledge in another part of the hospital where she went into cardiac arrest; the shoe was later reportedly found by a nurse.
At the very least, Parnia and his colleagues have written, such phenomena are “inexplicable through current neuroscientific models”. Unfortunately for the parapsychologists, however, none of the reports of post-death awareness holds up to strict scientific scrutiny. “There are many claims of this kind, but in my long decades of research into out-of-body and near-death experiences I never met any convincing evidence that this is true,” Sue Blackmore, a well-known researcher into parapsychology who had her own near-death experience as a young woman in 1970, has written.
The case of the shoe, Blackmore pointed out, relied solely on the report of the nurse who claimed to have found it. That’s far from the standard of proof the scientific community would require to accept a result as radical as that consciousness can travel beyond the body and exist after death. In other cases, there’s not enough evidence to prove that the experiences reported by cardiac arrest survivors happened when their brains were shut down, as opposed to in the period before or after they supposedly “flatlined”. “So far, there is no sufficiently rigorous, convincing empirical evidence that people can observe their surroundings during a near-death experience,” Charlotte Martial, the University of Liège neuroscientist, told me.
The parapsychologists tend to push back by arguing that even if each of the cases of veridical near-death experiences leaves room for scientific doubt, surely the accumulation of dozens of these reports must count for something. But that argument can be turned on its head: if there are so many genuine instances of consciousness surviving death, then why should it have so far proven impossible to catch one empirically?
Perhaps the story to be written about near-death experiences is not that they prove consciousness is radically different from what we thought it was. Instead, it is that the process of dying is far stranger than scientists ever suspected. The spiritualists and parapsychologists are right to insist that something deeply weird is happening to people when they die, but they are wrong to assume it is happening in the next life rather than this one. At least, that is the implication of what Jimo Borjigin found when she investigated the case of Patient One.
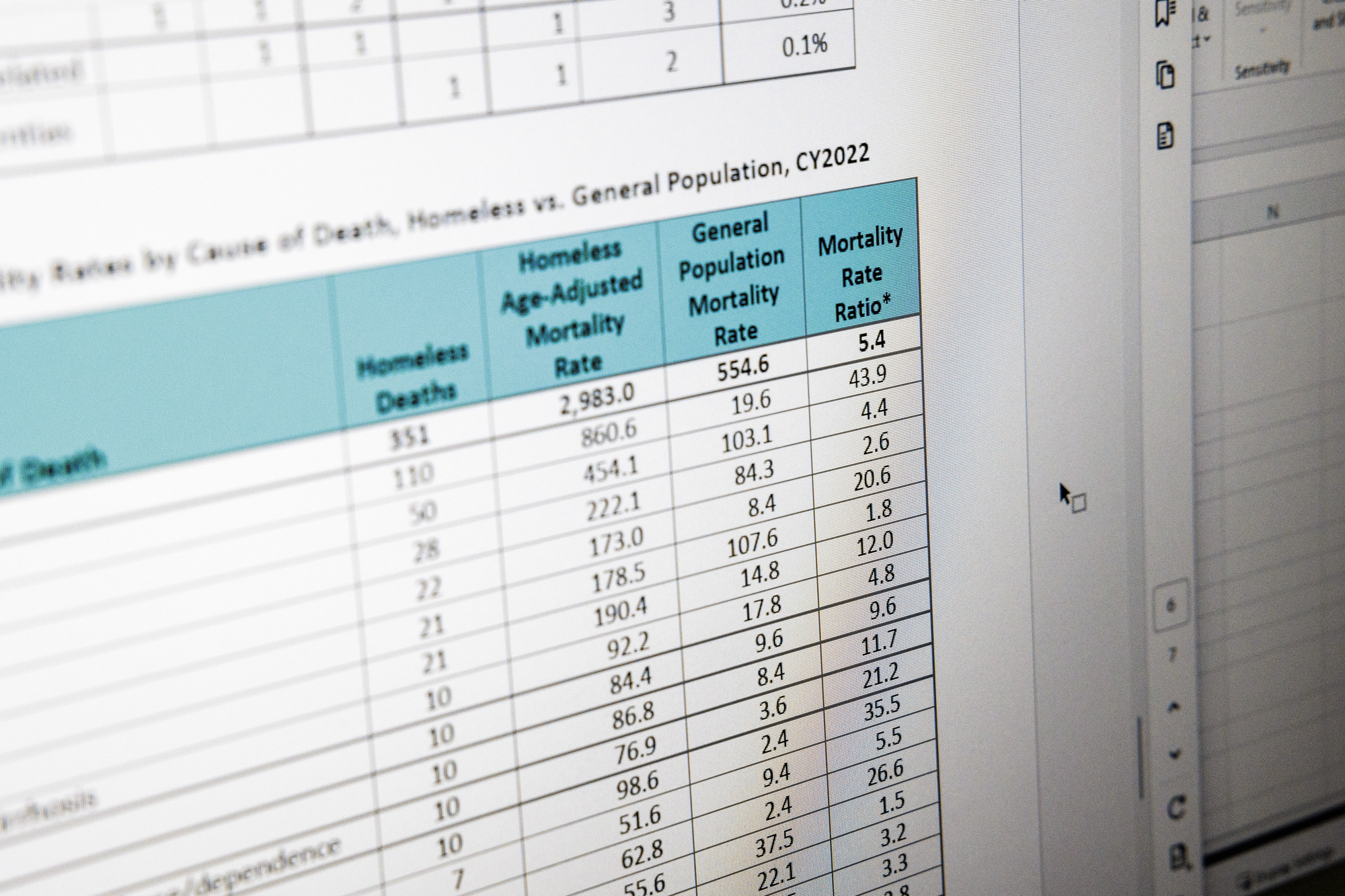
In the moments after Patient One was taken off oxygen, there was a surge of activity in her dying brain. Areas that had been nearly silent while she was on life support suddenly thrummed with high-frequency electrical signals called gamma waves. In particular, the parts of the brain that scientists consider a “hot zone” for consciousness became dramatically alive. In one section, the signals remained detectable for more than six minutes. In another, they were 11 to 12 times higher than they had been before Patient One’s ventilator was removed.
“As she died, Patient One’s brain was functioning in a kind of hyperdrive,” Borjigin told me. For about two minutes after her oxygen was cut off, there was an intense synchronisation of her brain waves, a state associated with many cognitive functions, including heightened attention and memory. The synchronisation dampened for about 18 seconds, then intensified again for more than four minutes. It faded for a minute, then came back for a third time.
In those same periods of dying, different parts of Patient One’s brain were suddenly in close communication with each other. The most intense connections started immediately after her oxygen stopped, and lasted for nearly four minutes. There was another burst of connectivity more than five minutes and 20 seconds after she was taken off life support. In particular, areas of her brain associated with processing conscious experience – areas that are active when we move through the waking world, and when we have vivid dreams – were communicating with those involved in memory formation. So were parts of the brain associated with empathy. Even as she slipped irrevocably deeper into death, something that looked astonishingly like life was taking place over several minutes in Patient One’s brain.

Those glimmers and flashes of something like life contradict the expectations of almost everyone working in the field of resuscitation science and near-death studies. The predominant belief – expressed by Greyson, the psychiatrist and co-founder of the International Association of Near Death Studies, in the Netflix series Surviving Death – was that as soon as oxygen stops going to the brain, neurological activity falls precipitously. Although a few earlier instances of brain waves had been reported in dying human brains, nothing as detailed and complex as what occurred in Patient One had ever been detected.
Given the levels of activity and connectivity in particular regions of her dying brain, Borjigin believes it’s likely that Patient One had a profound near-death experience with many of its major features: out-of-body sensations, visions of light, feelings of joy or serenity, and moral re-evaluations of one’s life. Of course, Patient One did not recover, so no one can prove that the extraordinary happenings in her dying brain had experiential counterparts. Greyson and one of the other grandees of near-death studies, a Dutch cardiologist named Pim van Lommel, have asserted that Patient One’s brain activity can shed no light on near-death experiences because her heart hadn’t fully flatlined, but that is a self-defeating argument: there is no rigorous empirical evidence that near-death experiences occur in people whose hearts have completely stopped.
At the very least, Patient One’s brain activity – and the activity in the dying brain of another patient Borjigin studied, a 77-year-old woman known as Patient Three – seems to close the door on the argument that the brain always and nearly immediately ceases to function in a coherent manner in the moments after clinical death. “The brain, contrary to everybody’s belief, is actually super active during cardiac arrest,” Borjigin said. Death may be far more alive than we ever thought possible.
Borjigin believes that understanding the dying brain is one of the “holy grails” of neuroscience. “The brain is so resilient, the heart is so resilient, that it takes years of abuse to kill them,” she pointed out. “Why then, without oxygen, can a perfectly healthy person die within 30 minutes, irreversibly?” Although most people would take that result for granted, Borjigin thinks that, on a physical level, it actually makes little sense.
Borjigin hopes that understanding the neurophysiology of death can help us to reverse it. She already has brain activity data from dozens of deceased patients that she is waiting to analyse. But because of the paranormal stigma associated with near-death studies, she says, few research agencies want to grant her funding. “Consciousness is almost a dirty word amongst funders,” she added. “Hardcore scientists think research into it should belong to maybe theology, philosophy, but not in hardcore science. Other people ask, ‘What’s the use? The patients are gonna die anyway, so why study that process? There’s nothing you can do about it.’”
Evidence is already emerging that even total brain death may someday be reversible. In 2019, scientists at Yale University harvested the brains of pigs that had been decapitated in a commercial slaughterhouse four hours earlier. Then they perfused the brains for six hours with a special cocktail of drugs and synthetic blood. Astoundingly, some of the cells in the brains began to show metabolic activity again, and some of the synapses even began firing. The pigs’ brain scans didn’t show the widespread electrical activity that we typically associate with sentience or consciousness. But the fact that there was any activity at all suggests the frontiers of life may one day extend much, much farther into the realms of death than most scientists currently imagine.
Other serious avenues of research into near-death experience are ongoing. Martial and her colleagues at the University of Liège are working on many issues relating to near-death experiences. One is whether people with a history of trauma, or with more creative minds, tend to have such experiences at higher rates than the general population. Another is on the evolutionary biology of near-death experiences. Why, evolutionarily speaking, should we have such experiences at all? Martial and her colleagues speculate that it may be a form of the phenomenon known as thanatosis, in which creatures throughout the animal kingdom feign death to escape mortal dangers. Other researchers have proposed that the surge of electrical activity in the moments after cardiac arrest is just the final seizure of a dying brain, or have hypothesised that it’s a last-ditch attempt by the brain to restart itself, like jump-starting the engine on a car.
Meanwhile, in parts of the culture where enthusiasm is reserved not for scientific discovery in this world, but for absolution or benediction in the next, the spiritualists, along with sundry other kooks and grifters, are busily peddling their tales of the afterlife. Forget the proverbial tunnel of light: in America in particular, a pipeline of money has been discovered from death’s door, through Christian media, to the New York Times bestseller list and thence to the fawning, gullible armchairs of the nation’s daytime talk shows. First stop, paradise; next stop, Dr Oz.
But there is something that binds many of these people – the physicalists, the parapsychologists, the spiritualists – together. It is the hope that by transcending the current limits of science and of our bodies, we will achieve not a deeper understanding of death, but a longer and more profound experience of life. That, perhaps, is the real attraction of the near-death experience: it shows us what is possible not in the next world, but in this one.
Complete Article ↪HERE↩!