— We live queer lives—and we can die queer deaths too

By Zena Sharman
At the funeral for Jamie Lee Hamilton, a trans Two-Spirit and Métis Cree activist and sex worker advocate, her community sang and danced to “Respect” and “Sisters Are Doing It for Themselves” during the church service and ate cupcakes decorated with rainbows and red umbrellas. When disabled queer Korean activist and organizer Stacey Park Milbern died, her community organized and livestreamed a 150-car caravan in Oakland and shared tributes under the hashtag #StaceyTaughtUs. Shatzi Weisberger, a Jewish dyke, death educator and activist known to many as the People’s Bubbie, died in 2022 at age 92. She got a head start on her funeral four years earlier by hosting her own FUN-eral, a death-themed party where her friends decorated a biodegradable coffin with glitter and got temporary tattoos while being serenaded by the Brooklyn Women’s Chorus.
What would you picture if I invited you to imagine your own gloriously queer funeral? Maybe it wouldn’t be a funeral at all, but a celebration of life, or a drag show, a brunch, a protest or a rave. Maybe it would be all of these things and more. Would there be sequins and glitter? Dapper suits and splendid hats? Leather and denim? Cozy onesies? No clothes at all? My ideal scenario is a cross between a potluck, a magic ritual and a dance party; I like to imagine my beloved people dressed in whatever they feel most comfortable in. I hope they sing, dance, eat, laugh and cry together, resplendent in their many expressions of queerness as they gather in remembrance and celebration.
Instead of a single event, you might want several gatherings reflecting different facets of your life: a religious service by day, followed by a raucous night at a dungeon, or an intimate ceremony for only your polycule, before a larger memorial open to all of the people who knew and loved you. For some, it might feel good for your chosen and families of origin to mourn together; for others, it will be important to create protected spaces that intentionally keep out your estranged parents or your transphobic aunt. You might choose rituals, traditions or ceremonies that are part of your cultural, spiritual or ancestral practices, or want something completely secular. Maybe you’ll want a virtual memorial so your friends and loved ones from all over can remember you together, or invite people to mourn you privately in whatever ways feel right to them. What we imagine can be as unique as we are.
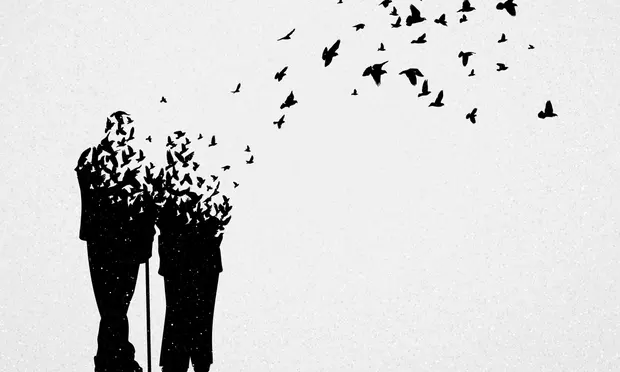
Our wildest imaginings likely differ from stereotypical depictions of funerals as formal, sombre events where black-clad mourners stand sadly around a heavy wooden coffin. Queerness offers us ways of perceiving and being in the world around us while making and remaking it through a distinctly queer lens. While the conditions of LGBTQ2S+ people’s lives often push us into unwanted proximity with death, we have the power to reimagine how we die and how we mourn. This includes active resistance to the violence and oppression that cuts short too many LGBTQ2S+ people’s lives and an invitation to subvert the beliefs and practices getting in the way of dying queerly, on our own terms. When we queer death, dying and mourning, they become sites of creativity, self-determination, collective care and resisting oppression, creating opportunities to challenge dominant ideas, practices and narratives that limit our ability to express who we are at every stage of our lives, including when we die.
As a death doula and self-identified death nerd, I talk about death a lot, and I’ve noticed that people tend to have one of two instinctive reactions when I bring it up: they recoil, regarding me strangely—or they lean in, wanting to know more. These leaning-in moments feel intimate to me. They often come with stories about a beloved person who died, questions about grief and death and the kinship of knowing it’s safe to talk about something that can feel unsayable. I’ve had these tender exchanges with friends, co-workers and strangers, which shows me how hungry many of us are for spaces where we can talk openly about death. There’s something about these interactions that feels inherently queer to me: holding space for each other while we share a raw or vulnerable truth, or reveal parts of ourselves that we’ve learned to keep hidden away.
Many of us have internalized a tendency to avoid talking about death, an instinct that can be accompanied by feelings of fear, anxiety or denial. When we do think about it, we may keep our thoughts to ourselves because we don’t feel ready to start a conversation about death with the people around us, or because we’ve consistently received messages that talking candidly about death or grief is risky or off-limits. For some of us—especially racialized, Mad and disabled people—talking openly about death or freely expressing grief can lead to pathologization or criminalization.
It can feel overwhelming to confront our mortality or that of the people we love, and many of us haven’t been taught the basics of what the dying process looks like, or what to do when someone dies. Before my oldest child was born, we went to a prenatal class to learn what happens during and after a birth. I wish I’d had a similar opportunity to learn about death a decade ago when I was caring for my mom at the end of her life. “We’re hungry to understand our own death and our own mortality and the death that surrounds us all the time, in a more real way,” Santa Fe, New Mexico-based death educator and host of the Death Curious podcast, Alexandra “Aries” Jo, tells me. They attribute this hunger to the stripping away of death from our everyday, mundane lives.
It hasn’t always been this way. It used to be more common in North America to experience death as a collective, community event. Deaths were more likely to happen at home, where family and community members—often women—cared for their own dead. Some communities have kept these traditions alive as part of their faith or cultural practices, and a growing number of people are accessing home hospice care. But for many of us, the past century has brought with it the increasing medicalization and professionalization of death and death care, transforming it into something that happens behind closed doors in settings such as hospitals or funeral homes. As a result, historian Katherine Arnup explains in a Vanier Institute report on death and dying in Canada, the experience of death has become “very foreign and frightening” for many people.
Yet it feels like an oversimplification to speak about death avoidance or the place of death in our everyday lives without acknowledging that many people and communities live and die in contexts saturated with death and grief, experiences that are tied to systemic oppression. “Loss is a part of life. Bereavement is natural. Grief is natural,” Oakland, California-based author and media justice activist Malkia Devich-Cyril tells me, “but mechanized loss, racialized loss, loss that comes as a result of inequality—that’s not natural. It is unnatural and it is the direct result of groups of people [in power] refusing to lose.” Devich-Cyril, author of a forthcoming book on Black grief and radical loss, points to how these forms of loss produce “an undue burden on those of us who have less power in the world. Grief becomes not only a consequence of disadvantage, but a cause of disadvantage and of disproportionate experiences of grief.”
Stefanie Lyn Kaufman-Mthimkhulu, a Providence, Rhode Island-based disability justice educator and organizer, challenges the idea that the COVID-19 pandemic prompted many people to confront death for the first time. When faced with this sentiment, Kaufman-Mthimkhulu tells me, “So many disabled folks I’m in community with are like, ‘Okay yeah, maybe for you, but not for us.’” Kaufman-Mthimkhulu’s own relationship with death and dying is shaped by being a younger disabled person who has experienced shifts in their body’s capacity and access needs while grappling with medical ableism. It’s also been influenced by their experiences of navigating chronic suicidality. When reckoning with their own mortality, Kaufman-Mthimkhulu draws on the “lessons in impermanence” that come with the “dynamics of living and dying on crip time.”
While I’ve read lots of books and taken several courses to learn more about death, dying and grief, the first people to teach me important lessons about collective care for dying people and how to come together in mourning were leatherdykes a generation older than me who’d lived through the AIDS crisis. It was they who showed me how to organize end-of-life care outside of inadequate and inaccessible state-run systems. They showed me it was possible to stop traffic to sing our beloved dead through the street into their memorial celebration. In these ways, they were part of a lineage of LGBTQ2S+ people who cared for their own dying and dead community members as part of a wider response to the state abandonment and systemic discrimination characteristic of the AIDS crisis in the 1980s and 1990s. Our lineages include experiences of immense loss and collective grief and trauma; they also include organized resistance, collective care and a refusal to abandon each other during and after death.
Today, in my own circles as a queer person, more than one friend has expressed surprise to me at having lived into their thirties or forties, ages they were convinced they’d never live to see. With waves of anti-trans legislation and fascist violence currently sweeping North America, many trans people are fearful of increased violence and risk of harm, prompting some to hold protest signs with the message: “The trans agenda is an average life expectancy.” While supportive of the larger death positive movement, Los Angeles, California-based end-of-life doula, writer and educator Vanessa Carlisle, who is queer and non-binary, tells me they prefer to think of themself as “death accepting” because “I don’t need to be death positive about how much death is happening in my community.” Carlisle, who has deep roots in LGBTQ2S+ and sex worker communities, emphasizes their commitment to fighting for community survival as part of their work in end-of-life care. They want the communities they’re part of “to survive and be happy and well in a world that seems hell bent on destroying us.”
Sarah Chavez, the Los Angeles, California-based executive director of the death education and advocacy non-profit The Order of the Good Death and a founding member of The Collective for Radical Death Studies, affirms that this spirit of resistance and solidarity is integral to death positivity. Chavez, who co-founded the modern death positive movement in 2011, tells me that death positivity is fundamentally “about engaging and talking about death in an honest and open way, without shame.” She emphasizes that we cannot do this “without engaging with the systems and conditions that lead to unacceptable or bad deaths that result from violence, a lack of care, and all forms of systemic oppression.”
“Queering death is also an opportunity to challenge narrow and limiting understandings of what constitutes a good death.”
How we die is intimately interwoven with how we live, Chavez points out, and “the exact same experiences and barriers that individuals encounter in life typically follow them right into death,” shaping our end-of-life experiences and what happens to our bodies after we die. She cites the example of the added stressors a dying person who is undocumented and their loved ones might face at end of life, like fear of deportation, family separation, language barriers, lack of access to cultural practices and the added costs associated with repatriation of someone’s body to their home or ancestral country. These barriers are systemic: a third of U.S. hospice programs limit access or outright refuse to care for undocumented people at end of life. This is why, for me, queering death demands the transformation of our health and end-of-life care systems and is wholly aligned with an abolitionist politic that includes border abolition.
Queering death is also an opportunity to challenge narrow and limiting understandings of what constitutes a good death. As researchers Cindy L. Cain and Sara McLesky write in an academic article on expanding definitions of the “good death,” qualities often associated with a “good” death—like not being a burden to others or mending familial relationships—“de-individualize the experience of death and disregard diversity within definitions of what is good.” These mainstream understandings, which shape the design of everything from our end-of-life care systems to the laws and policies governing death and dying to the training of hospice and palliative care providers, prioritize “a vision of dying that may not be achievable” or desirable to all patients and function as “a form of social control that seeks to discipline patients and their family members.”
An example of this is the ableism often inherent in stereotypical ideas of a good death. Kaufman-Mthimkhulu tells me they’ve often heard people describe a good death as “someone who’s died silently in their sleep at night, who’s a burden on no one and nothing.” They connect this to the “tremendous amount of fear” many of us internalize about “losing capacity, becoming more interdependent or more reliant on other people, or entering into new kinds of relationship dynamics where power might be shifting.” This is a very real fear for the disabled Canadians being systemically denied the supports they need to live while the government expands their access to medical aid in dying. At the same time, the ability to maintain our independence shouldn’t be the foundation on which we build our ideas of a good death. As in all facets of our lives, death is an opportunity to embrace interdependence as a foundational principle of disability justice. That’s why Kaufman-Mthimkhulu’s idea of a good death is “somebody who is able to move through the process of dying in a way that adheres to their values and beliefs and is met with compassionate, competent, self-determined care.”
In a blog post on what the death positive movement isn’t, Caitlin Doughty, the mortician and advocate who founded The Order of the Good Death, writes that it’s imperative to support communities to define “what a ‘good death’ means to them” and to work alongside each other to dismantle the barriers that get in the way of such deaths. When I think of how I might define what a good death means to me, I’m reminded of the consent practices I’ve learned from being part of sex-positive queer communities for the past twenty years. What feels good in the context of my embodied experiences, my identities, my relationships and my history might not feel good to you, and vice versa. When I contemplate this more broadly in relation to queering death and dying, I return to the themes of creativity, self-determination, collective care and resisting oppression.
To me, queering death is part of a larger liberatory project encompassing our efforts to fight for the survival and thriving of all communities experiencing systemic oppression. As a longtime LGBTQ2S+ health advocate, the more I look at death, the more I think about how we live our lives, what enables our individual and collective flourishing, and what gets in the way, at every stage of our lives. Queering death is about when, where and how we die, the care, support and options we have access to during this process, and what happens to us and our loved ones after our deaths. It’s also about actively working for a world where all LGBTQ2S+ people—especially those who experience the most significant and harmful impacts of systemic oppression, like people who are trans, racialized, Indigenous, disabled, Mad, poor, incarcerated, unhoused and/or undocumented—have what they need to live long, full, joyful lives free from violence and harm. Queering death is not about hastening the inevitable; it’s about fighting for us all to live and die in ways that respect, honour and celebrate every aspect of who we are.
Complete Article ↪HERE↩!