— Prolonged grief is normal—and even necessary.

By
When the pandemic dawned on our shores in early 2020, I neither panicked nor despaired. There was something eerily familiar about how quiet and still the world suddenly felt—how we were all living in a groundless, uncertain reality.
I’d had countless experiences with personal losses in recent years, so I knew how isolating grief could feel. Though this time, we were all sitting in a darkened room, the heaviness of loss wrapped around us like a cloak and bonding us together in more ways than one.
Over time, we’ve developed the language to describe this shared experience—collective grief. This mourning is neither an individual expression nor an experience, but can be felt as an entity that impacts a group of people all at once. For Black people, collective grief has a particular shape, feeling, and shade.

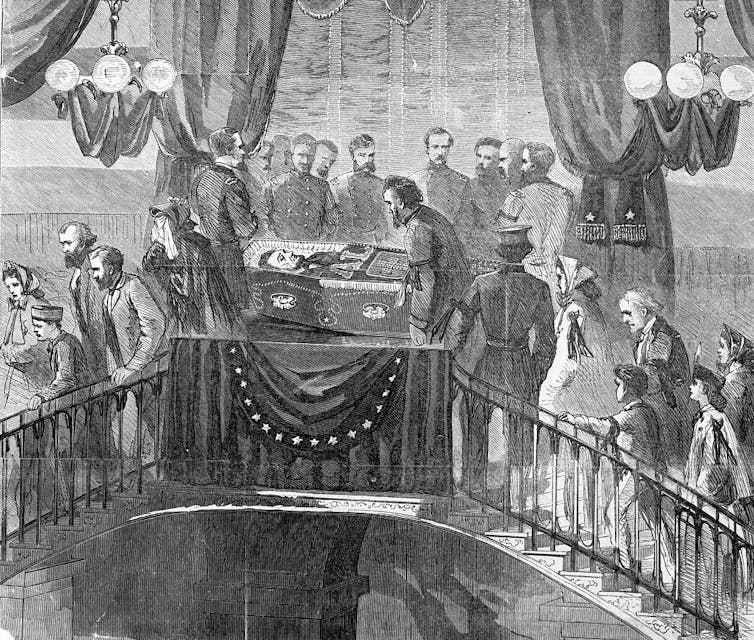
For Black people in the United States, grief and loss are intertwined with our very being. Our ancestors knew the trauma of loss intimately; many of us, myself included, are descendants of those enslaved. The institution of chattel slavery throughout this country—not just in the Southern states—depended upon breaking up families in order to use our Black bodies for labor. We lost so much then. Though we’re generations removed from it now, those losses remain within us, embedded in our consciousness and our psyche, lying dormant in our bodies.
As a result, Black people have experienced the pandemic differently, beginning with the fact that we were disproportionately impacted by this deadly virus. And we have grieved deeply as a result. I released my debut book, Self-Care for Grief, on Aug. 3, 2021. I began writing it in September 2020 when life still felt uncertain, but I wanted to give readers a soft place to land as they grieved. I wanted to remind people that they can grieve in their own way and that there aren’t any rules for how that should look. But that was hard to do knowing the state of the world outside my front door. The seasons were changing, which meant another spike in COVID-19 cases, hospitalizations, and deaths. The hope of a vaccine seemed like a pipe dream at best.
While official messaging encouraged everyone to continue being cautious, many Black people knew this to mean that, once again, we had to save ourselves. Misinformation was high. There wasn’t consistent or accurate reporting about how many people had contracted COVID-19. Guidance on how to protect ourselves—with masks, wiping down groceries, keeping a 6-foot distance—varied depending on the day. We had to bind together to get through, something Black people have always done. If we were going to survive, we needed to grieve, process, and make meaning of our losses. We inherently knew these things, even if many of us couldn’t recognize them at the time.
Grief requires tenderness. Demands it, even. As Black people, being rough or careless with our grief is more of the same indoctrination from Western culture and society. Trying to survive in this capitalistic society teaches us that we should not value stillness or rest. And racism always gives us a reason to be aggrieved and to fight for our humanity to be acknowledged and validated. Honoring our losses—and the grief that follows—means bowing to stillness. It then becomes necessary to have the courage to look at our grief and recognize it for what it is—not a nuisance to be gotten over as quickly as possible, but a force that will forever change us. Grief calls us to bend, to evolve, to integrate the losses that we’re reeling from.
Loss encompasses more than the death of a loved one. We may need to grieve former states of being, old routines, a neighborhood or city we moved away from, a dream we have outgrown or had to let go of, a sense of safety or inner peace, or the end of a relationship with someone who is still alive. The list is nearly as endless as the ways that we can honor our grief.

A Black Story of Grief
In modern times, there are new things to grieve. Rather than only hearing about the violence of white-supremacist police brutality on news stations or seeing it splattered on the front page of the newspaper each morning, we have the ability to witness it happening in real time via social media. We now have more awareness and more investment in taking a stand against racial injustice, but seeing these old wounds with even older origins so often, so graphically, comes at a cost.
The murder of George Floyd in Minneapolis on the evening of May 25, 2020, was a catalyst for the anger bubbling underneath the surface for most Black Americans to emerge with power and force. We were so tired of soldiering on even when little losses constantly surrounded us; of having to be OK with the unwarranted deaths of our brothers, sisters, cousins, aunts, uncles, mothers, and fathers. We were so tired that “tired” no longer sufficed; we needed another word to encapsulate the full breadth of all it means to hold, all it means to live as a Black person. We wanted to feel safe and to not fall prey to the potential lethality of driving while Black, walking while Black, eating while Black, traveling while Black.
We wanted Blackness in this country to stop equating to a death sentence.
Living with this knowledge is not only heavy but tortuous. It impacts mental health, the ability to build and maintain interpersonal relationships, holding onto employment and performing well. As much as one might think it’s possible to compartmentalize how structural and systemic racism affects Black people, that’s not the case. Robert T. Carter, professor emeritus of psychology and education at Teachers College of Columbia University, pioneered research on the relationship between racial trauma and mental health.
In a 2007 study, Carter found that, as a result of racial discrimination, Black people can develop racial trauma profound enough to be considered a psychological trauma comparable to PTSD, according to the criteria in the Diagnostic and Statistical Manual of Mental Disorders (DSM-5). “Racism can and does create damage to one’s psyche and personality in the same way that being subjected to community violence, being held captive, or being psychologically tortured can create emotional damage,” Carter writes.
Though Carter was one of the first to codify the mental health impacts of racism, five years earlier, psychiatrist and psychoanalyst Hugh F. Butts used the term “racial trauma” to ground further research, study, and understanding in the topic. In a 2002 article, Butts notes that “responses to racial discrimination by African-Americans are often not viewed as severe enough to indicate that these blacks may have post-traumatic stress disorder.”
PTSD from racial trauma can cause hypervigilance, depression, anxiety, and chronic stress, which forces our nervous systems to roar into overdrive.
And yet, more than two decades later, it’s reported that 71% of Black Americans experience some form of racial discrimination in their lives. This number seems low, especially considering how racial trauma actively changes us and the way we live. PTSD from racial trauma can cause hypervigilance, depression, anxiety, and chronic stress, which forces our nervous systems to roar into overdrive. New research from the University of Arizona takes this one step further. In a study published in April 2022, researchers Da’Mere T. Wilson and Mary-Frances O’Connor explored grief and bereavement implicit in the racial trauma Black people live with.
Wilson and O’Connor assert that solely associating grief with the loss of a loved one makes the definition “too narrow in scope.” Per the study, “This lack of representation, plus the prevalent universalist research framework in psychology, has led to a lack of understanding of how the specific contextual factors of living as a Black person, in a Western country like the United States, may differentially impact the experience of grief.” Like Carter, the two also research how grief and loss can catalyze political and social action. They illustrate that the racial trauma, grief, loss, and bereavement that follow are interconnected in an interdependent web.
So, how can we care for ourselves in a world that doesn’t recognize our pain and suffering—and doesn’t want us to be well?

How We Rebuild
Black Americans have created moving rituals to help us honor and process those losses. We are a communal people. The strength of the village, not just the heteronormative and very white nuclear family model, is what we lean upon.
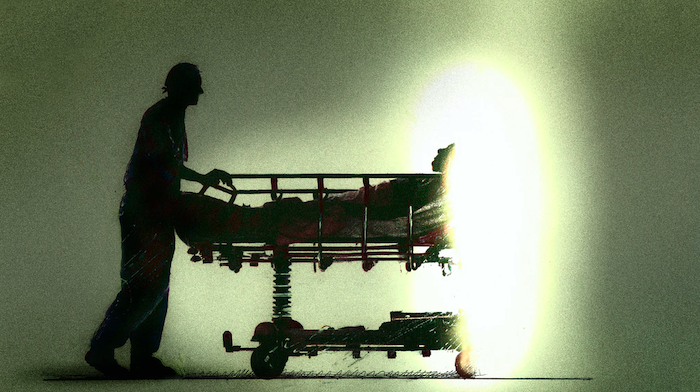
When someone dies, Black Americans gather at funeral homes, at churches, at banquet halls. We gather in love. We cry, we eat, we honor their lives. Yet, during much of the pandemic, these beautiful grief rituals have been disrupted. Instead we had to grieve alone in our homes, isolated from our communities, behind a computer screen. Zoom funerals became the norm, shaky cell phones and iPads capturing our grief in unprecedented ways. Within the grief space, there are Black folks meeting the evolving needs of their communities. Breathworker and grief guide Naomi Edmondson lost her grandmother, whom she considered a mother figure, in 2019. “When I lost her, in a way I lost the center of my universe,” she says. “Then having to handle that loss with COVID and the grief surrounding the pandemic, there were so many layers of grief that I was dealing with.”
As a result, Edmondson created a virtual space called Black Folks Grieve as a safe container for both herself and others who look like her to discuss their losses and grief. Every Monday evening, she facilitates a sharing circle for anyone who signs up via her website. “Before I started the group, I was looking for places where I could be in and not only feel like my grief was validated, but I didn’t have to do this intense labor to explain myself,” she says. “The last thing you want to have to do is the work of trying to make someone understand where you’re coming from.”
Fellow grief guide Alica Forneret came into the grief space after unexpectedly losing her mother in October 2016. Submerged in grief, Forneret channeled all she was feeling into Instagram missives about every aspect of grief. She also began consulting with companies on bereavement policies designed to make it easier for employees to cope with grief in the workplace. “How people treat you and your pain, the processing of pain, and your vocalization of that pain, I have found is the most interesting to talk to people about,” Forneret says. “The difference between me showing up to work every day in June of last year and everyone else is very different. The way that we are supported and need care is very different too.”
Now, she sees her work evolving. She’s working on her first book and is building a nonprofit called Pause that will help Black people formalize (and, in some cases, professionalize) their grief work to support those who need it most. Edmondson and Forneret are part of a legion of Black people—many of them Black women—revolutionizing how grief can be tended to. There’s Oceana Sawyer, a former transition guide, who uses Patreon to offer conversations and grief circles about honoring death as a rite of passage. She went from talking about grief on an individual level, before summer 2020, to now talking about collective grief.
She says she started looking at Resmaa Menakem’s work on somatic abolitionism and applying it to grief. “That led me to a deep exploration around how bodies, specifically bodies of the African Diaspora, are metabolizing grief alongside all the other losses that we incur on a daily basis.” This newfound curiosity fueled an expansion of Sawyer’s offerings: In addition to the virtual death cafes she’s led for Black and Brown people, she’s also hosted joy-mapping workshops on Afrofuturism, womanism, the end of the world, and more.
In the realm of academia, Kami Fletcher, associate professor of American and African American history at Albright College, refers to herself as a death scholar. She found her way into death studies during graduate school when her chair told her about an opportunity to act as a researcher for Mount Auburn Cemetery, Baltimore’s oldest African American burial ground. She spent years researching and writing about Mount Auburn and says, “It helped me to learn a lot about cemeteries, the records [that] this space keeps, and what that means to people who are supposed to be invisible in history.”
“I don’t think I realized that folks were using death studies—death, dying, bereavement, and grief—to mobilize and organize in really interesting ways,” she says. In 2018, she co-founded the nonprofit Collective for Radical Death Studies with the implicit aim to decolonize death studies and radicalize death practice. Death work, the Collective’s website states, is anti-racism work. It provides resources and information on death studies, death practices, and deathways, such as the Radical Death Studies Canon, which spans topics ranging from queer death and capitalism to colonialism and genocide. “Our mission is to decolonize death studies, and for us [that] really means to decenter whiteness,” Fletcher says.
There’s also author and end-of-life caregiver Breeshia Wade, who recently penned Grieving While Black: An Antiracist Take on Oppression and Sorrow, about living with racial trauma. And Sundari Malcolm, who hosts the BIPOC Dinner Party, an organization created with the goal of bringing people around (virtual) tables to talk about grief. Of course, there are countless others. The wide-ranging approaches to facing our grief and sitting with it, according to Forneret, is truly something to behold. It’s also something that gives her hope. “The diversity of people doing this work, the different ways they approach their work, and the complexities are so different and deep,” Forneret says. “It feels so rooted. And that’s why I want to support the people in our community.”
Complete Article ↪HERE↩!