Coloradans will decide whether to allow doctors to write life-ending prescriptions for terminally ill people
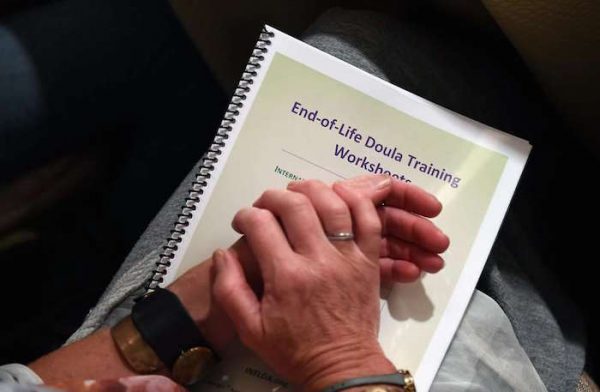
In November Coloradans will decide whether to allow doctors to write life-ending prescriptions for terminally ill people who have less than six months to live and want to die on their own terms. Whether the initiative is called “doctor-assisted suicide,” “dying with dignity” or “medical aid in dying,” though, will depend on who is paying for the campaign ad.
The language behind the fight is becoming almost as impassioned as the years-long battle over “pro-choice” and “pro-life” that morphed into “abortion rights supporters” and “abortion rights opponents.”
People in favor of the initiative use the terms “dying with dignity” and “right to die” but named their Colorado ballot measure the more neutral “end-of-life options,” although the secretary of state’s office calls it the Medical Aid in Dying initiative. The campaign also uses “medical aid in dying,” which is what proponents predict doctors will call the procedure if it becomes legal in Colorado, as it is in five other states.
Opponents of the proposed law — including many for religious reasons and others who fear it would target people with disabilities — call it “physician-assisted suicide.”
The loaded words on both sides are a case study in the power of language, and how rhetoric — or the art of public persuasion — can shape political debate.
“To communicate and attach ourselves to language is a very natural thing for a human to do, to the point that people will come to blows over ‘physician-assisted suicide’ or ‘dying with dignity,’” said Dr. Christina Foust, chair of the communication studies department at the University of Denver.
“When I think of the word suicide, I think of the words that sound just like it — homicide, infanticide. It has such a negative connotation,” she said. On the other side, “dying with dignity” connotes the ability to choose one’s own death, which is an affront to somebody who “might rest that power in God or a higher power.”
Coloradans probably will get tired of both terms by the election, after they are bombarded with TV and radio ads. But Foust and Dr. Jeff Motter, who teaches political rhetoric at the University of Colorado at Boulder, find it fascinating.
A similar linguistics battle exists over greenhouse gases: Is it “global warming” or “climate change”? There is the intense division over the #blacklivesmatter versus #alllivesmatter, a matter of a single word. And for more proof that language is powerful, consider that the words “date rape” and “spousal rape” weren’t part of the lexicon until the 1970s or 1980s, and their mere existence effected change, Foust said.
Motter, who recently moved to Colorado from North Carolina, has picked up on the way the cannabis industry is “very careful to always use the term cannabis and not pot or marijuana.”
“They are trying to reinvent the story, and the story of cannabis is the story of medical, clothing, the fiber of it, and it’s not about the recreation of it,” he said.
In Colorado’s latest social debate, “death with dignity” and “doctor-assisted suicide” tell two “very different stories,” Motter said. “Is it a story of human compassion or a story of murder?”
“Medical aid in dying” is a more neutral term because it sounds clinical, like most of the vocabulary used in medicine, Faust said. Motter agreed but questioned whether the word “aid” is innocuous because it implies “it’s not just optional; aid is essential.”
Opponents of the measure say the campaign is attempting to “sanitize” the act, in which a doctor writes a prescription for secobarbital that is later self-administered.
“If I was on their side, I’d want to sanitize it too,” said John Stonestreet, who is with the Chuck Colson Center for Christian Worldview. “It’s a hard thing to swallow. But some things are hard to swallow because they should be hard to swallow.”
“Dying with dignity” is a “euphemism for killing elderly and terminally ill patients by giving them a cocktail of toxic drugs,” Stonestreet wrote on his blog. He told The Denver Post “medical aid in dying” doesn’t convey the reality of what’s at stake. The phrase makes it sound as if doctors are only making their patient comfortable as they die, not providing the prescription that ends their life, he said. “A doctor should never do anything to cause death or harm,” Stonestreet said.
But proponents of the measure said “suicide” is a pejorative, shame-inducing word that implies someone has a mental illness and is choosing to die. “People who use medical aid in dying are victims of a terminal illness,” said Barbara Coombs Lee, president of the national Compassion & Choices organization and a board member for the Colorado end-of-life options campaign.
She compared the “choice” that terminally ill patients have to the one made by people who jumped out of buildings on Sept. 11, 2001, to avoid burning to death.
The political movement initially used the term “dying with dignity” in the late 1980s and 1990s, and was successful in passing a law by the same name in Oregon. “We knew the term was biased in our favor — it was our term,” Coombs Lee said.
The term “medical aid in dying” arose because the medical community needed language to distinguish the new practice from the crime of aiding and abetting a suicide — coercing someone to jump from a building or persuading them to overdose. “Those are heinous crimes,” she said. “They should be clearly disassociated from a legitimate and authorized medical practice. Doctors stab people with knives, and we call it surgery. They inject people with poisonous toxins and we call it chemotherapy.”
The ballot measure says two physicians must agree that a person — who must be at least 18 years old — is terminally ill and has six months or less to live and is mentally competent. It also requires that the person self-administer the secobarbital, which historically has been used in low doses as a sleeping aid.
The divisive language has left news organizations considering what is the most objective term to describe the procedure. KUSA-Channel 9 recently informed viewers the station will call it “assisted suicide,” going by the Oxford definition of “the action of killing oneself intentionally.” Others, including The Denver Post, use “medical aid in dying,” noting that the word suicide carries meaning beyond the dictionary definition.
“Language does matter,” Motter said. “Both sides want their frame, and that’s because both sides are creating their story.”
Complete Article HERE!