By Nancy Walker
[D]eath anxiety is not a distinct disorder but might be connected to problems of anxiety and depression such as:
- Panic disorders
- Panic attacks
- Post-traumatic stress disorder PTSD
- Hypochondriasis
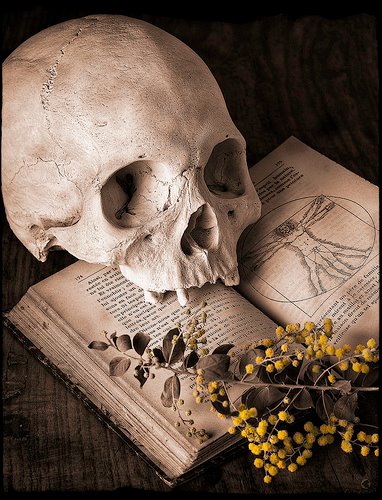
Thanatophobia is quite different from necrophobia, which refers to a general fear of the dead or dying things, or anything that is linked with death.
In this article, we will discuss thanatophobia or death anxiety, explore the signs and symptom, reasons, and treatments for this problem.
What is Thanatophobia?
The word thanatophobia has been derived from two Greek words, Thanatos meaning death, and Phobos meaning fear. Hence, thanatophobia means the fear of death.
Being anxious about death is quite normal and a part of human behavior. However, in some cases, people may suffer from an intense form of fear or anxiety when they think about their own death or the process of dying in general.
A person may feel extreme fear and anxiety when they think that their death is inevitable. Other than this, they are also likely to experience the following symptoms:
- Fear of separation
- Worry about leaving the dear ones behind
- Fear of suffering from a loss
When these fears and disruptive thoughts become so intense that they stop the sufferer from performing his daily activities, this condition is known as thanatophobia.
In the most severe forms, these feelings can hinder the patients from living their lives and performing daily activities. Their fears tend to center on things that may cause death such dangerous objects or contamination.
Diagnosing Thanatophobia
Doctors do not consider thanatophobia as a separate condition, however, it can be considered as a specific phobia.
As per the Diagnostic and Statistical Manual of Mental Disorders, a phobia refers to an anxiety disorder that relates to a specific situation or an object.
The fear of death may be considered as a phobia if it:
- Arises every time the person wonders about dying
- Continues to persist for a period of more than 6 months
- Interferes with the life and relationships of the patients
Some of the key symptoms that a person is suffering from a phobia of dying include:
- Immediate anxiety or fear when thinking about the process of dying
- Panic attacks that may lead to hot flushes, dizziness, sweating, and increased heart rate
- Avoiding situations where the concept of death or dying is discussed
- Feeling pain in stomach or general sickness when thinking about dying
- A general feeling of anxiety or depression
Phobias may lead to a person feeling extremely isolated and avoiding any contact with family and friends for long periods of time.
The symptoms may come and go throughout the entire life of an individual. Someone suffering from a mild form of death anxiety can feel their anxiety heightening when they think about their own death or the death of a loved one, particularly when he himself or any family member is seriously sick.
If the death anxiety is connected to another depressive condition, the patient is likely to suffer from the symptoms related to that particular disorder as well.
Types and Causes of Thanatophobia
While thanatophobia refers to the general fear of death, there are a lot of types of this disorder which depends on what the patient is focusing on.
Phobias are often experienced by a specific event occurred in the patient’s past, even though the person does not always remember it. Some particular triggers that lead to thanatophobia include a traumatic event related to the near death of self or a loved one.
A person who is suffering from a severe illness has a high risk of developing thanatophobia. This is because chronic patients are always anxious about dying, however, ill health is not necessary for someone to experience death anxiety.
Most of the time, thanatophobia is related to psychological illness.
The experience of thanatophobia may differ from person to person and mainly depends upon individual factors like:
- Age: A study performed in 2017 suggested that older adults are more likely to experience the process of dying as compared to the younger ones who fear death itself.
- Sex: As per a 2012 research, women are more likely to suffer from the fear of death, which may be their own or that of a loved one.
It is common for the medical professionals to connect anxiety near death to a range of different mental illnesses such as PTSD, depressive disorders, and anxiety.
How to Treat Thanatophobia
Social support networks can help protect a person from thanatophobia. Some people are likely to come to terms with their deaths with the help of their religious beliefs but this may perpetuate the anxiety related to death in others.
People enjoying a good health, high self-esteem, and a belief that they have spent a fulfilling life are less likely to fear their death as compared to others.
A doctor usually recommends a person suffering from thanatophobia to receive a treatment for phobia, anxiety, or any other problem that may be triggering this fear. The treatment involves a talking or behavioral therapy. These therapies teach the individuals to focus on their fears and work through them by expressing their concerns.
The treatment options for thanatophobia usually include:
Cognitive Behavioral Therapy
Cognitive behavioral therapy or CBT includes working with the patient in order to alter his behavioral patterns in such a way that he adopts newer ways of thinking.
In this therapy, the doctor works in collaboration with the patient to come up with practical solutions in order to overcome the anxiety and depression. This eventually leads to the development of strategies that make the patient unafraid and relatively calm when he talks or thinks about death.
Exposure Therapy
Exposure therapy works by helping someone face their fears. Instead of suppressing the feelings of death in a person, this therapy encourages the patients to expose them and acknowledge them.
A therapist will work very carefully in order to expose a person to his fears but ensuring that he is in a safe environment. This is repeated until the response of a person towards the factor causing anxiety reduces.
The person is able to confront his own thoughts and feelings without any fear.
Medicines
If a patient has been diagnosed to have a certain mental disorder such as PTSD or generalized anxiety disorder (GAD), he may be prescribed to take anti-anxiety medications such as antidepressants or beta-blockers.
Using these medications together with other psychotherapies can be extremely effective.
Relaxation Therapies
Practicing self-care can boost the overall mental health of a person. It can also help a person to cope with his fears and anxieties. Avoiding caffeine and alcohol, sleeping well, and eating a healthy diet are some of the easiest ways to practice self-care.
When a person suffers from anxiety, specific relaxation techniques can reduce the stress on their minds and reduce the fears. They may include:
- Performing deep breathing exercises
- Focusing on certain objects in a room, like counting the tiles on the floor, or meditation
Outlook
While it is completely natural to express concerns about your future and the future of your loved ones, if the death anxiety persists in your behavior or more than 6 months, it indicates that you require medical help.
The fear of death can be overcome by different ways and your mental health professional can guide you through them in a better way.
Complete Article ↪HERE↩!