— An increase in a certain kind of high-frequency wave in dying brains might be associated with last-minute conscious experiences, but scientists don’t know for sure.
In their last minutes of life, some people’s brains generate a surge of surprisingly organized-looking electrical activity that may reflect consciousness — although scientists aren’t entirely sure.
According to new research, published Monday (May 1) in the journal PNAS (opens in new tab), this surge can sometimes occur after a person’s breathing stops but before the brain stops functioning. The activity pattern is somewhat similar to what is seen when people are awake or in dreamlike states, leading to speculation that perhaps these electrical surges reflect the otherworldly experiences reported by people who’ve had close brushes with death: A sense of looking at the body from the outside; a tunnel and white light; or a sense of reliving important memories.
However, since all the patients in the new study ultimately died, it’s impossible to know if they had such experiences.
“If you talk about the dying process, there is very little we know,” said Jimo Borjigin (opens in new tab), a neuroscientist at the University of Michigan Medical School who led the study. It’s rare for patients to have their brains continuously monitored as they die, Borjigin told Live Science. “This is maybe the first study to really show second-by-second how the brain dies.”
Near-death experiences
Some people who are brought back from the brink of death report seeing or hearing unexplained things during resuscitation or when they seem to be unconscious. The reason for these near-death experiences is unknown, and it’s not clear if they’re even specific to death.
International surveys suggest that only about half of what people call “near-death experiences” actually occur in life-threatening situations, said Daniel Kondziella (opens in new tab), a neurologist at the University of Copenhagen who was not involved in the new research. The other half occur during meditation or in scary situations that don’t endanger one’s health or impact the brain’s metabolism, Kondiziella told Live Science.
“The thing is, from the experience itself you cannot say if someone has had a cardiac arrest or syncope [a brief loss of consciousness] or near-miss traffic accident,” Kondiziella said.
Because the people who survive to report a near-death experience are inherently different from the people who die — their brains don’t permanently lose function, for one thing — it’s hard to determine whether those who actually die also have these subjective experiences.
In 2013, Borjigin and her colleagues measured electrical activity in the brains of rats (opens in new tab) that they euthanized via cardiac arrest. They found that for about 30 seconds after the heart stopped, the brain showed a surge in what are called gamma waves, which are the highest-frequency electrical oscillations in the brain. Gamma waves are correlated with conscious experience, but don’t necessarily prove that someone is conscious; they’re just one of many indicators that someone might be aware and alert.
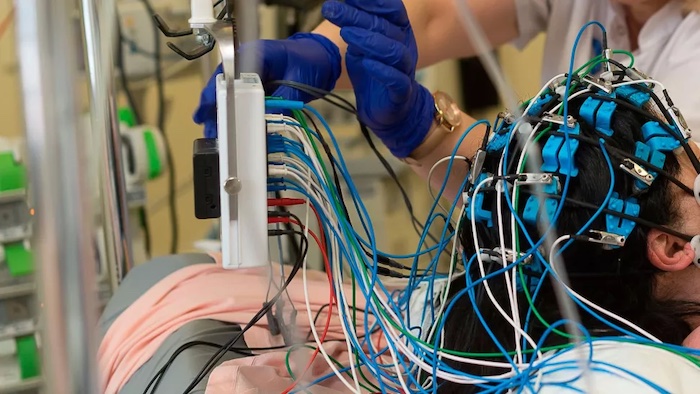
In 2022, a separate group of doctors happened to be monitoring the brain of an 87-year-old man with an electroencephalogram (EEG), which detects electrical activity on the surface of the brain, when the man unexpectedly died. Similar to Borjigin’s rats, the man’s brain showed a surge in gamma activity in the 30 seconds before and after his heart stopped.
‘Reading’ the dying brain
In their new paper, Borjigin and her team made a deliberate effort to use EEG to capture what the brain looks like during death.
The researchers got permission to monitor dying patients in intensive care whose breathing support had been removed after treatment proved futile. The study included four patients total, all of whom were comatose after cardiac arrest.
In the 30 seconds to two minutes after their ventilators were removed, two of the four patients’ brains showed surges in gamma waves. Interestingly, this gamma activity seemed organized, in that the gamma waves in one portion of the brain were associated with predictable activity patterns in other regions.
The temporoparietal junction, a brain region where the temporal and parietal lobes meet, toward the back of the brain behind the ear, was particularly active with gamma waves. This region is known to be activated when people have out-of-body experiences or dreams, Borjigin said.
The new findings echo what was seen in the 87-year-old patient who unexpectedly died, said Raul Vicente (opens in new tab), a neuroscientist and data scientist at the University of Tartu who co-authored the 2022 study but was not involved in Borjigin’s work. “It’s very nice to see a confirmation,” he told Live Science.
“The more consistent findings we have, the more evidence it is that this likely is a mechanism happening at the time of death and if we can pinpoint this down to one location, even better,” said Ajmal Zemmar (opens in new tab), a neurosurgeon at the University of Louisville Health who also co-authored the 2022 study.
Zemmar and Vicente are optimistic that these signals could be signs of conscious experience at the moment of death. But reflecting the debate in the field, Kondziella is more skeptical.
“We know when you die a cardiac death as opposed to a brain death, that takes time,” he said. Minutes pass between the heart stopping and brain cells dying, he said. “It shouldn’t be a big surprise during those minutes, you will see aberrant electrophysiological activity in the brain.”
Some people may experience something like near-death experiences in these moments, Kondziella said, but we may never know for sure. And again, these experiences may not be unique to death — a more likely explanation for near-death experiences that encompasses both life-threatening experiences and non-life-threatening experiences, he said, may be “REM sleep intrusion into wakefulness,” a situation in which the brain blends waking and dreaming states. (REM sleep is marked by dreaming and brain activity patterns that are very similar to waking, including gamma waves and other, lower-frequency waves.)
Borjigin’s team is still collecting end-of-life data, hoping to add to the evidence that the dying brain may generate predictable gamma-wave patterns. Already, other research groups have attempted to use artificial intelligence to identify objects that people saw in their dreams (opens in new tab) based on their brain activity — similar mind-reading may be possible with unconscious and dying patients, Vicente said.
“This opens an opportunity at some point, if we gather enough data, to be able to decode what people in different coma states are thinking,” Vicente said.
Complete Article ↪HERE↩!

