The last time I saw my grandfather, he was 95 years old. He walked with a bent back. Kindness graced his watery eyes.
During dinner, he asked me how old my son was at least four times.
“Is he 2?” he inquired once again.
“Almost. He’s 21 months, Grandpa,” I answered.
He smiled and returned to eating his tilapia, mashed potatoes and squash.
At the end of our visit, I walked him to the car. As we approached the steps leading down to the garage, he mentioned his bad knee – an injury from the war.
“I can do it,” he said, gently refusing my hand. “Just one step at a time.”
As my uncle opened the car door, my grandpa suddenly stopped. He turned back to look at me. He kissed his hand and lifted it up in the air. I blew a kiss back to him. He “caught it,” then brought it to his cheek with a knowing smile.
The last time I saw my grandfather, he blew me a kiss. That is what I remember most.
Doulas and Dying
I am a doula. I am also a hospital chaplain. In holding space for birthing and dying, I’ve come to see one thing clearly. Standing with an open heart in the presence of birth is very much like standing with an open heart in the presence of death.
The word “doula” translates from Greek to mean “woman servant.” Today, doulas are known best for accompanying laboring and/or postpartum women. Doulas offer emotional, mental, spiritual and physical support during the transition of opening to new life. According to a 2013 nationwide survey conducted by Listening to Mothers, around 6 percent of expectant couples in America hire a birth doula. This number is small, but it’s growing. In 2006, only 3 percent of birthing women had doula support.
The vast majority of American women give birth in a hospital. Given this, the compassionate and consistent presence of a doula offers a healing tonic in an impersonal and medicalized obstetrical setting. Doulas focus solely on providing comfort measures, based on best practices, to ease the pain of labor and steady the heart and mind of a birthing woman. As a doula, I offer support for hours on end. I do my best to mirror back to a woman her courage, beauty and strength. Doulas believe in the power of birth and regard the process of birth as sacred.
What happens when we take the doula model described above and apply it to end-of-life care? What if we doula the dying?
Like with birth, the majority of Americans die in a hospital. While the majority of us wish to die at home, according to the National Center for Health Statistics, only 27 percent of Americans do. Most of us are born and die surrounded by medical professionals and beeping machines. Ideally, the technology associated with important medical advancements doesn’t eclipse the perennial needs of the human heart. Women birth best when they feel safe, are supported, and their bodies are allowed to open with organic wisdom. In the same way, the dying are best comforted with human touch, love, story and song.
In 2003, Henry Fersko-Weiss, a licensed clinical social worker, created the first end-of-life doula program in the U.S. He saw that there was “a gap” that hospice and medical professionals couldn’t fill when it came to supporting the dying and the bereaved. He trained with Debra Pascali-Bonaro, creator and director of Orgasmic Birth and chair of the International MotherBaby Childbirth Organization. Fersko-Weiss transferred knowledge gained about birth doula work to caring for the dying. As president of the International End of Life Doula Association (INELDA), he trains hundreds of individuals, drawing upon his studies of the intersectionality of birth and death work. Today, a small but growing number of organizations wisely build upon the doula model and offer training to support the dying and bereaved.
Fersko-Weiss is unique. Few end-of-life care professionals are trained in birth work. Few birth workers are trained in caring for the dying. Yet, uncanny similarities in best practices exist across these professions. At the October 2014 Midwives Alliance of North America annual conference, I spoke about the overlapping skill set taught in both my training as birth doula and hospital chaplain.There is much to be gained from studying what it means to hold space for both birth and death.
Holding Space
“That sure looks like my brother Darcey,” my grandpa said a few days before he died. His eyes gazed across his room. Then, he added, “Hi Mom. Will you stay close to me today?”
Will you stay close to me today?
When the veil between our visual world and the wonders beyond the physical senses thins, we seek out the hands of loved ones. Whether a mother holds these hands as she bears down to push a beloved child into our world, or whether an elderly woman holds the hands of her children as she breathes her last breath — we reach for each other. We do.
Wisdom and insight are born when we stay close to the birthing and dying. Wounds from the past can be healed. Forgiveness and perspective dawn. Our culture is currently fragmented from much of this wisdom. The training of doulas represents a healing shift. By holding compassionate and nonjudgmental space, doulas support families as they make room for the generations to enter and exit this world. As we attend to birth and death, we touch upon a great mystery and deeply benefit from being starkly reminded of our own mortality.
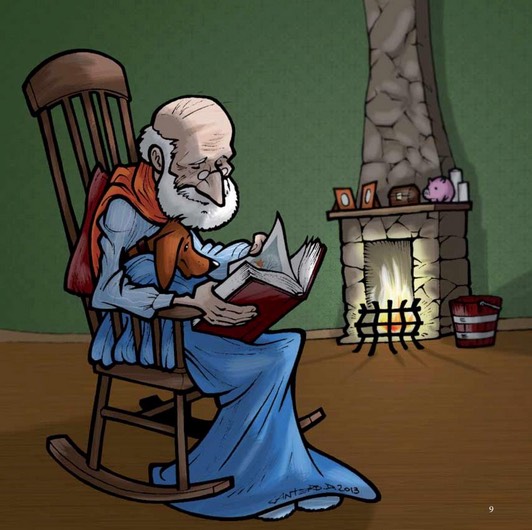
During my grandfather’s final days, his grandchildren and great-grandchildren came to his bedside. While he received quality and attentive hospice support, it was the consistent and compassionate care of his seven children that mattered most. In particular, my Aunt Colleen’s remarkable devotion to her father made it possible for him to live out his final years and eventually take his final breath in the comfort of his own home. She was his doula.
While the birth/postpartum doula movement makes important inroads in our maternity care system, great commitment and insight are needed to bring doula care to the dying. The elderly are easily disregarded in a culture that worships youthfulness, independence and productivity. Like infants, the dying remind us of our fragility, our dependency and our need for each other. When we sequester either birth or death, we lose touch with the truth of our interdependence, the nesting of generations, and what Buddhist teacher Thich Nhat Hanh calls our “interbeing.”
‘Just one step at a time’
As I work to train death doulas, hold space for the birthing and meditate on the mysteries that connect the threshold points of life, I remember my grandfather’s words: “Just one step at a time.” Yes. Just one birth, one death, one step at a time.
Slowly, steadily, the doula movement brings needed healing to how we perceive and experience both birth and death. Holding compassionate presence in our most fragile moments reminds us of what matters most. Certainly, it’s not what we possess. Even the location of birth or death is secondary. It’s the presence of love and the gentleness we bring to our mortal journey that matter most.
The last time I saw my grandfather, he blew me a kiss. I hold it close to my cheek. It inspires me to do this work.
Complete Article HERE!