Inside the Cafés Where People Go to Talk About Dying

By Lexi Pandell
We sat in a circle, clutching paper cups full of steaming coffee and tea. First, I said my name. “Hi, I’m Lexi.” What came next wasn’t an admission of addiction, but a statement about what I feared most about death. “I fear the unknown,” I began, but paused. That didn’t quite sum it up. My voice tight from nerves, I added, “Nothingness. Losing everything I’ve ever known. The whole thing, really.”
This is life at Death Café, an event where strangers gather to snack and chat about shuffling off this mortal coil. It sounds (literally) morbid, but in this Age of Anxiety, as people grapple with climate change, threats of violence, and political and economic instability, death lingers on many people’s minds. A fear of dying is at the root of all those stressful issues and, as Sheldon Solomon put it when speaking to The Atlantic in 2015, those things are “all malignant manifestations of death anxiety running amok.” It’s cyclical: Anxiety spiral, fear of death, bad decisions, rinse, repeat. Despite this, people rarely talk about their own mortality. Death Cafés strive to break that taboo.
That moniker—Death Café—is both the name of the organization that came up with a format for these death-discussion groups and the term for the meetings themselves. The gatherings can be hosted anywhere—community centers, living rooms, hospices, or regular old coffee shops. I attended one in a funeral home. They cost nothing to attend and, as the official website reads, “in the Death Café there are no hierarchies. We all meet simply as people who are going to die.” Though some attendees may have lost loved ones, it’s not a place for bereavement or grief counseling. It’s also not the place to attempt to convert anyone to a religion. Rather, it’s intended as an open, salon-style conversation. The experiences I’ve had varied wildly: At one of them, two people claimed to have seen ghosts. Another veered toward practical discussions of funeral and estate planning. I’ve met people who’ve had near-death experiences, who are terminally ill, who deal with death as part of their daily work, who are afraid of death (or not), and who believe in the afterlife (or, like me, don’t).
The gatherings are run like AA meetings about death (think of it as MA: “Mortals Anonymous”), but the precise format depends on the host. The greatest commonality is offering attendees something to eat or drink, typically cake or another sweet accompanied by coffee or tea. “It’s life-sustaining,” says Megan Mooney, Death Café’s social media head. “It makes people feel more comfortable talking about death.”
The concept began with “café mortels,” created in 2004 by Swiss sociologist and anthropologist Bernard Crettaz. The events were adapted and popularized as “death cafés” by Jon Underwood, who held the first one in the basement of his London home. Soon after, he and his mother, Sue Barsky Reed, started an official website with guidelines for anyone who wanted to host their own. From the beginning, the Death Café organization has been not-for-profit and run entirely by volunteers. Today, associated events are held in more than 60 countries. Though Underwood died suddenly last year at age 44, his mother and his sister, Jools Barsky, now run the organization.
Memento Mori
Death, you could say, is having a moment. Organizations like Underwood’s—as well as Death Salon and Death Over Dinner—are helping people talk about it. YouTube channels like Caitlin Doughty‘s popular “Ask a Mortician” are helping people learn about it. So, too, is Doughty’s group The Order of the Good Death, which aims to bring together funeral industry professionals, academics, artists, and others to help our death-phobic culture confront mortality. There has even been a recent spate of buzzy death-related books, like Mary Roach’s Stiff or Atul Gawande’s Being Mortal.
Yet, when it comes to appropriate cocktail party conversation, death is often put in a corner along with sex and money. Many prefer to avoid it altogether, even when faced with old age or terminal illness.
Our aversion to death is rooted, of course, in evolution. In psychology, there’s a term known as “terror management theory,” which refers to the fact that, while humans intellectually understand the inevitability of death, our survival instinct protects us from fully confronting it. Many, instead, seek a kind of immortality through their beliefs about the afterlife, their offspring, or even fame. Humans are wired to fear dying—and to be superstitious about it.
“People don’t want to talk about death because talking about it makes it real,” says Mooney, who researches mortality for the University of Missouri and is also a social worker for hospice and end-of-life care. “But there’s a saying in the Death Café world that talking about sex won’t make you pregnant and talking about death won’t make you die.”
Still, it’s scary at first. Do you remember the first time you realized you were going to die? Like, really realized it? I do. For me, it happened around age 9 during a visit to my grandparents’ home in Long Island. As I lay in a twin-sized guest bed listening to the sound of cicadas chirruping in the humid summer night, an understanding of my mortality hit me like a wave. Nothing in particular inspired this feeling, but there it was, definite and staggering. Someday, I will die. A pit grew in my stomach, the edges of my vision went dark. I cried out for my mother and when she came to me I told her, sobbing, what I’d been thinking about. Ever the realist, she brushed back my hair and said, “Of course, sweetheart. We all will. But you won’t for a very long time, so try not to worry about it.”
I worried anyway. Throughout childhood, I probably obsessed about death more than the average kid considering I kept a folder on my computer’s desktop titled “In Case I Die.” (Naturally, it was full of terrible poetry to read at my funeral, letters to friends, and directives about who should inherit my book collection in case of my untimely demise.) It was twee more than practical, but when I was a teenager, several family members died without planning much—one after a battle with terminal disease, another more suddenly—leaving the rest of the family to deal with their possessions and unclear wishes amid our grief. I vowed I wouldn’t pass as they did.
Yet seriously thinking about my own mortality still terrified me, even years later as I got my start in journalism as a crime reporter and became inured to regularly reading grisly coroner’s reports. Eventually, it was time to face the music. I forget how I first learned of Death Café, but the concept hit on something I needed to explore.
Funeral Parlor
Like me, Louvain Rees’ interest in death changed after her father passed. Today, she’s a historian who studies death and remembrance in Welsh culture. Because there were no Death Cafés hosted near her in Wales, Rees will soon be hosting one of her own at St. Fagans National Museum of History, which will include handling sessions with the museums’ “mourning collection,” such as jewelry made from human hair. “I cannot say that I have fully accepted the inevitable,” she says, “but I am in the process of doing so.”
Discussing death can feel a bit like talking about a hangover while you’re still enjoying the party, yet it can be immensely liberating and help prioritize what’s important in life. Mooney, who grew up dreaming of being a mortician, hosted her first Death Café in 2013 and, since then, has helped kick off events in Hong Kong and Austin. A pivotal moment came when her death-avoidant father attended the first café she ever hosted. Soon after, he began picking out funeral songs. “Every time I got in the car, he played Patty Loveless’ ‘How Can I Help You Say Goodbye,'” she says. “From that, he planned his funeral, made health care directives, did everything.” Death Café not only helped him confront his own mortality, she says, but made things much easier for her when he passed away nine months ago.
“I started making some big changes in my life because I didn’t feel like I was being true to myself,” Mooney says. “I felt I was just existing in certain areas of my life.”
Likewise, attending Death Cafés have loosened something in me. I haven’t gotten over all of my fears, and that’s fine. Death Café doesn’t aim to eliminate existential dread; it’s just about opening dialogue about something we’ll all have to face someday. It’s eye-opening to walk into a room full of strangers and remember that you have one essential thing in common. I’ve always been the youngest one in the room at these meetings and, several times, people have come up to me at the end of meetings to commend me for it.
“You’re so young to be thinking about death,” one older woman said to me. “I wish I had done this at your age.”
Complete Article ↪HERE↩!






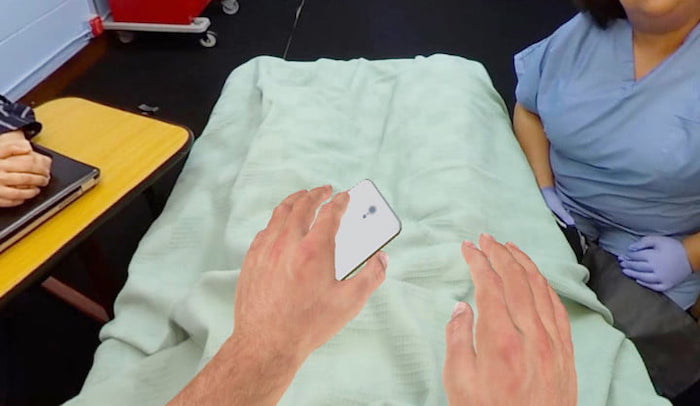



 Through its painstakingly created and very human VR experiences, the company has cornered the market on a type of next-generation training tool. It provides an experience that caregivers or clinicians cannot get simply by reading textbooks.
Through its painstakingly created and very human VR experiences, the company has cornered the market on a type of next-generation training tool. It provides an experience that caregivers or clinicians cannot get simply by reading textbooks. Of course, there are problematic aspects with the idea of building empathy through VR. A 30-minute simulation about end-of-life conversations is not the same thing as experiencing it for real. A person really experiencing the effects of homelessness or discriminatory activity cannot simply take off their headset when they decide they’ve had enough of their life circumstances. Attempts to “gamify” complex scenarios risk inadvertently diminishing them, and carry the chance of turning something intended for good into something exploitative.
Of course, there are problematic aspects with the idea of building empathy through VR. A 30-minute simulation about end-of-life conversations is not the same thing as experiencing it for real. A person really experiencing the effects of homelessness or discriminatory activity cannot simply take off their headset when they decide they’ve had enough of their life circumstances. Attempts to “gamify” complex scenarios risk inadvertently diminishing them, and carry the chance of turning something intended for good into something exploitative.