— How hope shapes patients’ awareness of their advanced cancer prognosis

Hope is defined as the expectation of achieving a future good. Patients with cancer, whether it is curable or not, prioritize cure as their highest hope.
Patients with incurable cancer wish to be informed about their disease and its treatment, but also need to maintain hope. This inner conflict can impact how they process information about their prognosis.
Prognostic awareness
Physicians are ethically obligated to inform patients about their prognosis so that patients can make cancer treatment decisions that are consistent with their values. When oncologists talk to patients about prognosis, they tend to talk about the extent of the disease (localized or metastatic), the goal of the treatment (curative or palliative) and the estimated survival (short months or many years).
Communication about prognosis can be challenging due to physician factors such as skill in discussing bad news, and patient factors such as denial. Some patients with incurable cancer, who are aware of their prognosis but haven’t accepted it, will say the treatment goal is cure.
Previous research indicates that less than half of patients with incurable cancer are aware of their prognosis. This is often attributed to a failure of communication.
But are patients truly unaware, or are they aware and not accepting of their prognosis? If inaccurate prognostic awareness is due to denial in spite of adequate communication from the oncologist, then interventions to improve communication may be ineffective, misguided or even harmful.
Patients with incurable cancer are more likely to receive end-of-life care concordant with their preferences when they have accurate prognostic awareness. Inaccurate prognostic awareness can lead to conflicting treatment decision-making between patients and oncologists, delayed referral to palliative care and more aggressive care at the end of life.
In a study of patients with advanced lung cancer, those who received early palliative care and had accurate prognostic awareness were more likely not to choose intravenous chemotherapy in the last two months of life, which would have been futile and worsened the quality of their end-of-life care.
How prognostic awareness is measured
Measuring prognostic awareness in patients is challenging because their responses may reflect their hopes rather than their true beliefs. In a recent publication in the Journal of the National Cancer Institute, our research team synthesized data from 52 studies measuring prognostic awareness in patients with advanced cancer.
In the majority of studies, prognostic awareness was conceptualized as a binary entity: patients were asked if their cancer was curable, and their responses were coded as either accurate prognostic awareness (patients knew their cancer was incurable and responded that it was incurable) or inaccurate prognostic awareness (they thought it was curable and responded that it was curable).
A few studies included in our review improved upon the binary conceptualization by incorporating hope in the assessment of prognostic awareness.
These studies asked patients about their belief and their doctor’s belief about prognosis and found that about a third of patients will hold onto hope for a cure (responding that they believe their cancer is curable), even when acknowledging that their doctors were treating them with palliative intent. This discordance was attributed to poor coping.
The role of hope
Hope is a recognized coping strategy in patients with cancer. However, “false” hope may have detrimental effects. Patients may refuse to believe their prognosis and demand aggressive treatments that may cause more harm than benefit.
In the context of advanced cancer, the relationship between hope and hopelessness is balanced by acceptance, which can re-direct hope to new goals beyond cure, such as hope for connection with others and enjoyment of daily pleasures.
Nurturing hope among patients with cancer and their caregivers is possible and includes coping strategies focusing on what can be done (such as control of symptoms) and exploring realistic goals such as dignity and intimacy. Family and spirituality play an important role in supporting patient hope.
Incorporating patient hope into prognostic awareness
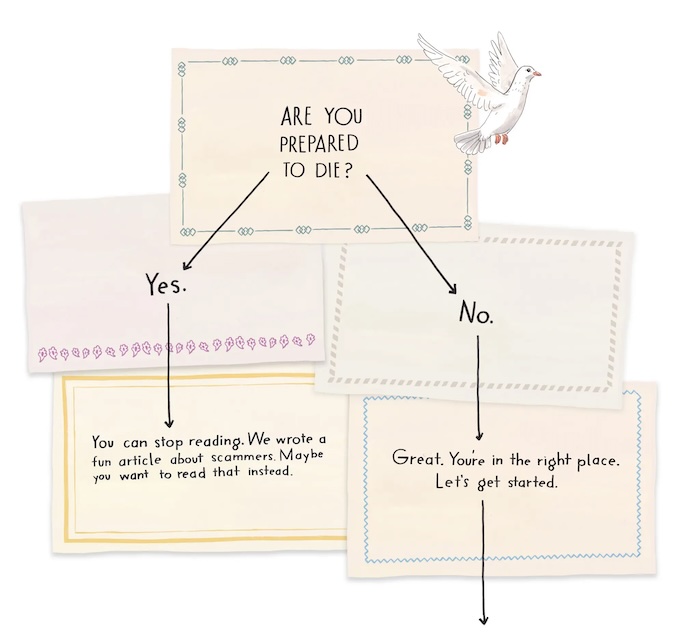
We improved upon the binary conceptualization of measuring prognostic awareness by incorporating patient hope, creating a trinary concept: patients who are aware and accepting of their prognosis; aware and not accepting; or truly unaware.
We propose that patients who are aware and accepting should be offered psychological supports to address any negative effects on mood; those who are aware and not accepting should be offered adaptive coping strategies to support their evolving prognostic awareness; and those who are truly unaware will benefit from interventions such as decision-aids and communication training. Early palliative care consultation may be beneficial at each stage of prognostic awareness.
This trinary conceptualization may guide future research to improve our understanding of the impact of hope in the setting of serious illness and help patients receive the right supports in their cancer journey.
Complete Article ↪HERE↩!