A family fights to turn off a pacemaker
By Jennifer Friedlin
For the past month, my mother and I have been advocating for the deactivation of my father’s pacemaker. Yet despite my parents having taken every measure to ensure that they would control the ends of their lives, two months since a severe stroke destroyed whatever quality of life my father, who was already suffering from advanced dementia, had left, his heart continues to beat against my family’s wishes.
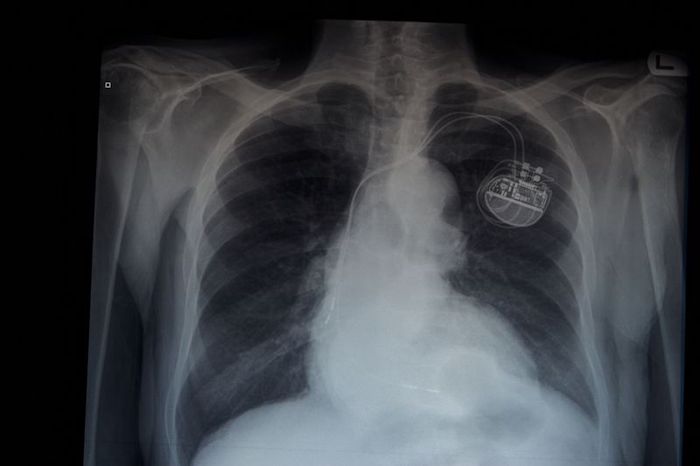
In 2010, the American Heart Association, American College of Cardiology, the American Geriatrics Society and other prominent groups issued a statement indicating that the deactivation of a pacemaker, an implantable device used to speed up slow heart beats, is ethically permissible. Reaffirmed last year, the statement says, “Legally, carrying out a request to withdraw life-sustaining treatment is neither physician-assisted suicide nor euthanasia.”
Nevertheless, the team of medical professionals at Parker Jewish Institute for Health Care and Rehabilitation has given us the runaround. Most recently, my mother and I met with my father’s team of medical professionals to discuss moving my father into hospice as well as deactivating the pacemaker so that my father could live out his days naturally. During the course of the meeting, my mother, who is my father’s proxy, made clear that this would be my father’s wish.
According to the law, the request is my mother’s prerogative. In 1990, in Cruzan vs. Director, Missouri Department of Health, the Supreme Court ruled that a competent patient could refuse life-sustaining treatments, including nutrition and hydration. This case gave rise to advance directives so that a proxy could carry out the patient’s will. In a later case, the Court affirmed the right of competent patients to refuse therapy.
The medical team agreed to hospice, but has so far refused to carry out the request to deactivate the pacemaker. We have had several long conversations with the medical team, and, while they seem to agree with our desire to give my father a dignified end, they offer confusing explanations as to why they will not carry out my dad’s wishes.
At one point, a staff member told me that because a pacemaker does not prolong life, we should leave it. But my father’s pacemaker is working 53% of the time to correct his condition, known as bradycardia, which can result in heart failure. I fail to see how this device is not prolonging my father’s life or, at the very least, interrupting the possibility for his natural demise.
We are certainly not the first family to confront the medical community’s refusal to deactivate a pacemaker. Katy Butler, author of “The Art of Dying Well,” has written extensively about her efforts to give her father the death he wanted by deactivating his pacemaker. Butler also uncovered other horrors, such as cardiologists recommending pacemakers for elderly people with advanced dementia.
Much of the motivation, Butler noted, seemed to stem from the financial rewards of treating people, even the terminally ill. Simply put there’s no money in death. And yet in its current design, at $450 a day for room and board alone, institutions like the Parker Institute rake in millions annually from people whose lives are being maintained artificially. The medical system could quite literally bankrupt healthy family members to keep a dying one alive.
Although estimates vary, each year approximately 400,000 people — half over age 75 — get implantable cardiac devices, including pacemakers. Primary care doctors, cardiologists, and elder care attorneys should inform people about how these devices can affect their end of life and encourage them to include their wishes in advance directives.
Yet, even if they do, they may hit the same wall of refusal my family has faced. It seems that despite the legal rulings and the ethicists’ writings, doctors are committed to keeping pacemakers ticking.
It’s unfair to the terminally ill and their families that this view prevails. The refusal to deactivate means the sick family member is denied a dignified death, while the need for constant advocacy leaves family members feeling like they are making an unseemly demand.
As the debate about healthcare builds in the run up to the 2020 presidential election, I hope that the candidates will discuss reforms to improve end of life care. There should be dignity in death for the terminally ill and no healthy person should be forced into bankruptcy to keep a loved one alive against his or her will. There are certain people we should spare no expense to keep alive, in our family’s opinion my father is not one of them.
Complete Article ↪HERE↩!