by Jeff Nagel

More than 65 B.C. residents have legally ended their lives with the help of a doctor since federal assisted death legislation took effect June 17.
Fraser Health officials confirm some of those deaths have been within this region, but referred requests for detailed numbers to the B.C. Coroners Service.
“Our first request was two days after the federal legislation was put in place,” said Lisa Zetes-Zanatta, Fraser Health’s executive director for palliative care, home care and residential care.
“A number of requests have come in and some have completed the service.”
Coroner Barb McLintock said it’s too soon to provide a regional or other breakdown on B.C.’s assisted deaths, which she said stood at 66 as of Wednesday.
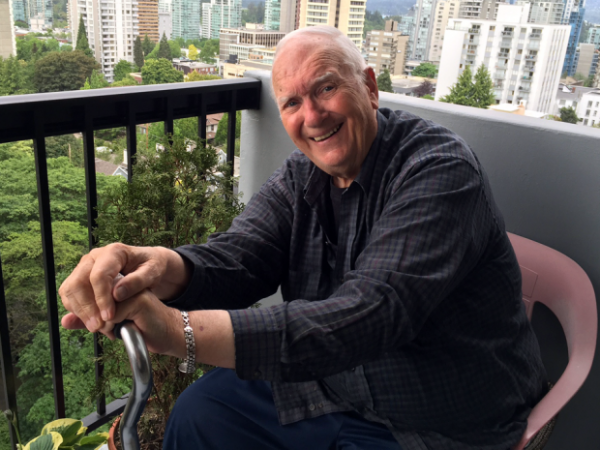
The most high profile case so far made public has been that of author W.P. Kinsella, who lived in Yale and invoked Bill C-14’s assisted dying provisions Sept. 16 at Fraser Canyon Hospital.
The Catholic Church’s Vancouver Archbishop Mark Miller urged Fraser Health in an open letter not to mandate assisted dying as an option in palliative care wards, calling it a “cruel dilemma” for those vulnerable patients.
And Miller said it’s a “terrible conflict of interest” for palliative caregivers who may be compelled to offer “an economically expedient shortcut in the form of lethal injection” contrary to their ethical principles.
Zetes-Zanatta acknowledged that not all doctors or nurses are willing to participate, but said that has not been a barrier to finding sufficient volunteers.
“We’re very clear, as is the provincial and federal legislation, that conscientious objection is absolutely respected,” she said. “I would never force any of our staff into doing anything not consistent with their own moral, ethical or spiritual beliefs.”
Doctors can perform the assisted death injection independently if nursing staff who would normally assist are unwilling, she said.
Zetes-Zanatta noted the World Health Organization definition of palliative care is to protect and alleviate the suffering of patients until they reach a natural death.
“The number of palliative care physicians providing this service is less than other disciplines because it’s not aligned with their philosophy of care. That being said, there are palliative care physicians who are providing this service.”
More of the requests for assisted death come from people in the community than in hospices or palliative care settings, she added.
“We try to give the service where the patient is,” Zetes-Zanatta said. “They’re usually in intolerable suffering and so to move them is really difficult. We try to make this very much about the patient.”
Under the federal legislation, patients must be at end of life with death expected within the next six months to a year.
Only they – and specifically not youth or psychiatric patients – can make an initial request leading to more information on the assisted death option.
Usually those requests go through a family doctor, Zetes-Zanatta said, but Fraser Health will assign physicians to respond to patients who don’t have one.
“We ensure that they have had access to palliative care services and pain management services to see if we can alleviate their suffering prior to them making a formalized request for this.”
After the information provision stage, two doctors must conduct independent assessments, after which there is a 10-day waiting period before the patient can finally make the choice to die.
She said Fraser Health is now legally required to comply when patients qualify.
“Regardless of where people sit on this we have to recognize that there are patients requesting this. And we have to understand what that patient must be going through to put in a request like this.”
The legislation passed by the Justin Trudeau government came after the Supreme Court declared it unconstitutional to prevent suffering Canadians from getting medical assistance to hasten death.
Complete Article HERE!