Ensuring that the care you get reflects your wishes and values
[W]hen someone you love is hospitalized with a grave illness or injury, you may face decisions about their care.
Cardiopulmonary resuscitation (CPR), mechanical ventilation, tube feedings, surgery, chemotherapy or other interventions may add weeks, months or years to their life.
If your loved one has an advance directive (living will), it will spell out which interventions they want and don’t want. If they don’t have one and can’t speak for themselves, how should you proceed?
To help families learn to make good choices in this situation, Silvia Perez Protto, MD, Director of our Center for End of Life Care, answers key questions below.
Q: What’s the first thing families should consider?
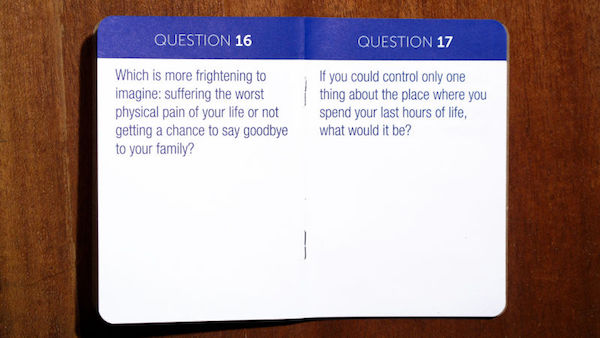
A: First, determine whether the patient is capable of making a decision about treatment. If so, your best option is to explore their wishes and values:
- What are they expecting and hoping from treatment?
- What are the trade-offs of treating versus not treating?
- What risks are acceptable and not acceptable to them?
- Which do they value more: quality of life or quantity of days?
Depending on their age, situation and views, answers will vary.
One paralyzed patient may be happy sitting with family and watching TV. Another may not.
One patient may want doctors to extend her life despite pain, nausea, or loss of mobility to see her son graduate from college. Another may be unwilling to experience serious side effects from a treatment that isn’t 100 percent effective.
We want to honor the patient’s wishes. When patients can’t communicate and have no advance directive, we look to families for guidance.
Q: What’s the best way to start the conversation?
A: I encourage families to talk to loved ones about end-of-life wishes and values before they get sick or develop a serious condition. You won’t go wrong trying to explore someone’s wishes and values.
When I asked my own mother what she wanted at the end of her life, I learned she wanted to be around her five children, to be able to communicate with us and to be independent. This led me to understand that if she became terminally ill and couldn’t recognize us, she wouldn’t want to live like that.
Some people wouldn’t mind being on a feeding tube or a ventilator, unaware of their environment. Others wouldn’t want to live in a vegetative state.
These questions are tough and emotionally difficult to ask mom or dad. Even I got stuck talking to my mom. But we can always ask for help. A spiritual care advisor or palliative care doctor at your hospital can facilitate these discussions.
(And remember to tell loved ones about your wishes and values, too.)
Q: Do larger issues get in the way of these discussions?
A: I think not talking about death is cultural. It’s how we see life, it’s our spiritual background, it’s our own fear of dying.
I’ve heard patients say, “I feel like I’m dying, but my kids don’t want to talk about it.” This isolates them at the end of life. Pain and isolation or abandonment are our main fears when we’re dying.
But the more we talk, the less fear we’ll have. Everybody’s going to die. Avoiding the topic won’t decrease the chances of dying. As a society, we need to normalize death. Being born, growing up, having kids, dying – these are all part of the life cycle.
Q: What questions should you ask about end-of-life care?
A: If you’re worried how an illness may impact the end of your life, talk to your family doctor, primary care doctor or specialist. Ask, “What are the side effects, risks and benefits of the treatment you’ve recommended?” Once you have that information, see how it lines up with your wishes and values.
If you want your doctor to keep trying to treat the disease, we can provide palliative care along with the treatment, controlling your symptoms and minimizing your pain. If you choose to end treatment, it doesn’t mean we’re giving up. We’ll still provide palliative care right up until the end.
Our goal in the ICU is always to get patients better and back to a functional life at home. But that’s not always possible. We can aim either to extend life or to offer the best quality of life in the time the patient has left.
These conversations and advance directives show us how to proceed and help us allow patients to die with dignity.
Q: Are there proven benefits to end-of-life planning?
A: Yes. Studies show that when advance care planning is done, the family’s experience and the patient’s experience are better. In the United States, autonomy is very important. Advance directives help you maintain your autonomy at the end of life.
Healthcare providers are encouraged to obtain advance directives and document patient’s wishes in their chart for all caregivers to see.
Q: Any final word for families?
A: I encourage families to see death as a natural act and to understand the value of a natural death. We can do many things to extend life, but sometimes the price we pay is having no quality of life.
Complete Article HERE!