— Advice from the Cancer Wars
The emotional and physical toll on both of us during our last year together
By Leida Snow
Everybody has a sell-by date, but some folks know theirs in advance. About a year ago, my husband and I had a meeting with a doctor who was new to us. Nice looking man with an open face. He saw our expectant looks and stopped mid-sentence. Looking at Lou he said, “Has no one mentioned that you have stage 4 cancer?”
No one had. We knew there was an issue. Lou has one kidney from birth, and at his yearly checkup, the kidney specialist said to talk to a cancer doctor. But he didn’t seem overly anxious.
I was grateful that finally someone was speaking truth. The hardest to hear was that Lou had, probably, about a year to live. It was as though someone had taken a very sharp knife and plunged it into my stomach.
The oncologist explained that Lou had cancer cells in his liver, but they were not those expected to be there. They were squamish cells, usually associated with other locations. That meant they had spread (metastasized) from somewhere else. But they didn’t know where they had come from.
A Rare Form of Cancer
Lou has cancer with unknown primary (CUP). It affects 2% to 5% of diagnosed cancers. The doctor’s next words tore at my gut: Because the primary source is unknown, there are no data-based, targeted treatments. In other words, for those with CUP, treatment is a guessing game.
I was grateful that finally someone was speaking truth. The hardest to hear was that Lou had, probably, about a year to live.
We had gotten the news at NYU Langone, a top-flight institution where we see our specialists. The overwhelming advice was to go to Memorial Sloan Kettering (MSK) in New York, the Gold Standard, we were told.
Given the restricted time frame, we expected MSK to build on NYU’s findings. But they had to re-do tests, to validate the results. Over the following months, I swallowed my anger and frustration, as the days filled with tests, biopsies, CT scans, MRIs, x-rays and hours spent waiting. The immunotherapy and chemotherapy had zero effect on killing any disease. I hugged Lou close as he comforted me when I couldn’t control the tears.
Lou suffered all the side effects — extreme fatigue, drug induced lung infection, steroids to deal with that, removal of huge amounts of fluid from his lungs, and, best/worst of all, the loss of over 30 pounds. Lou has never been fat. Now he is emaciated. I try not to show him how scared I am.
Not long ago, I heard a crash in the bedroom to find my 6’2″ formerly strong darling dazed on the floor.
There was the offer of one clinical trial. A hope glimmer. But it had mind-blowing side effects and wasn’t aimed at cancer with unknown primary. Lou decided to pass. I steeled myself to be strong for him.
So now we’ve enrolled in what’s called Home Hospice. It’s basically a space where there is no treatment, but you still hope for a magic bullet. Where I watch my husband become less every day.
Not long ago, I heard a crash in the bedroom to find my 6’2″ formerly strong darling dazed on the floor. Lou said he’d bent over to get his shoes and then started to fall without being able to control what was happening. The wall behind him was blood smeared. He had hit his head.
Feelings of Helplessness
Panic. Heart racing. Cloths to press on his head. An ice pack. The hospice said to do what I was doing. Asked if Lou wanted to go to the hospital. No. Didn’t know if I could get him up. But I did. The cut wasn’t deep, but I thought the bleeding would never stop. On his physician’s advice, Lou is no longer taking Eliquis, a blood thinner.
Last year I wrote an article for Next Avenue that flagged that falls can be the beginning of the end. Now it is shattering, personal knowledge.
I’ve cancelled almost everything. Since hospice, there’s minimal interaction with MSK and the long waits. We had to scrub our last session at MSK’s Center for Integrative Medicine. The acupuncture helped Lou to relax, but he was too exhausted to attempt to go.
A Lonely Road
It didn’t feel right to phone and cancel. I went to the appointment and spoke to the doctor. He counseled me to take care of myself. He asked me to keep in touch. His caring for Lou, and for us as a couple, is something I will always remember.
Lou doesn’t want to spend whatever is left of his life in a hospital, and I want to respect his wishes. My insides churn with helplessness.

My own NYU internist has scheduled a monthly video visit to check up on me, especially since I’ve lost more than 15 pounds unintentionally. And the local rabbi calls this agnostic at least once a week. Some friends have disappeared, but there are those who keep in touch. And, yes, I do have someone I can talk to. But it is a lonely road.
Over a year later, my 87-year-old husband has outlived his prognosis and is a shadow of what he was. But he is here. And I want him here.
Some people get inspired after a diagnosis. They reach for a goal or get everything in order. Lou is frustrated and bored, but he is too worn out to do much of anything. I want things however he wants them.
Mostly, he wants to sleep or read the newspaper or hug me. That’s what I cling to. That he’ll be there to cradle me in his arms me as long as possible. Sometimes we go to the sofa and lie with my head in his lap. Lou believes his job is to take care of me, and some of his distress is that he can’t anymore.
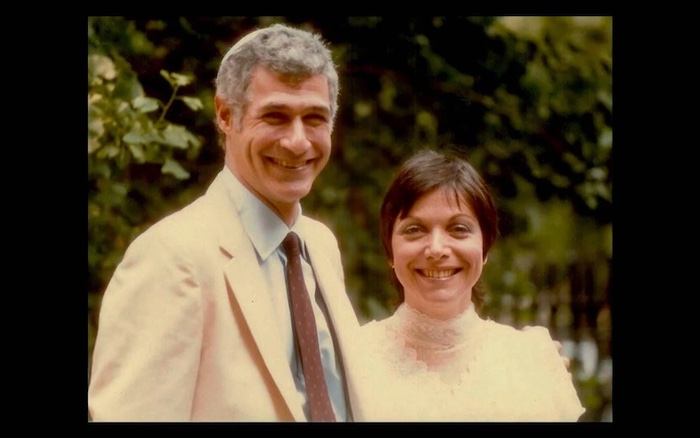
Sleep? Not so much. Exhausted. Deeply. What to do? Besides cry. Besides wish I could do more for this man who’s been my life for over 41 years. Because I can’t imagine my world without him. He’s my rock and my biggest fan, the one whose faith in me is stronger than my own. His all-embracing love is where I am home. Whatever I want to do, wherever I want to go, I want to share those experiences with Lou.
That’s the hardest part of Now. Because I’m with him in this no-man’s land, where we can only cling to each other and wait for the inevitable.
Of course, we would have tried anything, gone anywhere when we first heard Lou’s diagnosis and the medical predictions of our future. But if I’d known then what I know now, I would have encouraged Lou to make a different decision.
Regretting Endless Tests and Treatments
There are cancers that can be targeted. Cancer with unknown primary is not one of those. I hope anyone reading my words never faces what’s in front of us. But if you find yourself in this nightmare, here’s what I would say: Don’t spend whatever time you have going to doctors, submitting to endless tests and treatments, waiting in anonymous rooms filled with distracted, unhappy people. Sitting on uncomfortable chairs, being so vulnerable. Dealing with all-business staff that has all the time in the world, while your time is limited. And waiting. Waiting. Waiting.
If I had known then, what would I have done? I would have gone back to Paris with my husband, or we could have gone to the Broadway shows we missed.
If I had known then, what would I have done? I would have gone back to Paris with my husband, or we could have gone to the Broadway shows we missed. We would have reminded ourselves how lucky we were to be able to walk home from the theater. We could have taken in New York’s magisterial skyline from celebratory dining spots.
Now Lou is beyond tired. His legs give way and he falls, can’t get up. Sometimes I’m not strong enough, and we have to call for help. His MSK doctor says he’s fallen too many times and is not safe at home. Emotional overload. The doctor wants me to move him to an in-patient hospice. Lou knows not being home is a possibility. He is disconsolate.
No. I am not going to rush into anything. Moving furniture to make room for a hospital bed, even though Lou says he won’t use it. Never-ending efforts to schedule health aides. Medicare comes through with 15 – 20 hours a week. We now need 24/7. Trying not to think too far ahead.
Welcome to the third ring of hell. You may have read that because of COVID many health care workers died/changed careers/moved away. At the same time, more and more people need qualified help. Hours are spent trying to figure out what’s possible.
Recently my darling said, “What a terrible burden I’ve put on you.” I thought my heart would crack. “I don’t feel it as a burden,” I said, startled by my truth. What is breaking my heart is the fear that I won’t be able to help him, that I won’t know what the right thing is. Fortunately, the hospice physician and woman covering for him are knowledgable and compassionate.
So far, there is no pain. One blessing among the horrors. But he is suffering, and we are looking at a future of unknown — though not long — length.
Struggles of a Caregiver
As I’m writing this, Lou is visibly deteriorating. He can no longer turn himself easily in bed or rise to a sitting position without help. He can barely stand for a moment with assistance while he is moved from the bed to the wheelchair.
What is breaking my heart is the fear that I won’t be able to help him, that I won’t know what the right thing is.
I can’t imagine how people navigate this without a caring partner, but anyone taking on the caretaker role should know in advance: there is mighty little guidance. It’s learn-on-the-job. Case workers and nurses may or may not be thoughtful and compassionate, but you have to think of the questions to ask because too often no one volunteers information.
Are you willing to stay in because you don’t trust that the aide will keep your loved one safe? Or because the aide didn’t show up? Are you prepared to spend hours of your time trying to find coverage even though the agency assured you they would always be able to come through? Can you handle the blowback when you cancel what isn’t working? Can you deal with the additional cost? Are you prepared for the never-ending laundry? Can you function with catch-as-catch-can sleep, only a few hours each night?
My husband is dying. But he’s not gone yet. A few nights ago, he agreed to the hospital bed. He understood that if I don’t get some sleep, I won’t be able to be there for him. He hates the bed. Misses me at night. I miss him too.
Lou eats little, sleeps at odd hours, is restless at night. The aide has to wake me. Lou’s speech is now slurred. It’s hard to understand him. He is angry. He forgets. He wants the hospital bed and the strange people in the apartment gone. He wants me with him all the time. I am terrified.
Addendum: The Death of My Husband
In the daytime, he dozes, wakes, starts to read the newspaper, dozes, wakes, tries again to read. My plan was to write how I would put my arms around him, wanting him to know how much I love him. I was going to share how he would reach out to put his arms around me, wanting me to know how much he loves me.
On September 17th, Lou slept most of the day and night. He mumbled about wanting to go home. I held his hand, said he was home and I was with him. I used to call him my giant, and I told him that I would still choose him out of all the giants in the world. I said I would always be with him and he would be with me. He smiled, squeezed my hand and moved his lips to kiss me.
The next day, he woke and surprised me, wanting to brush his teeth, shave, shower. The aide helped him into the wheelchair and into the bathroom. Afterwards, I warmed some chicken soup. He reached for it and gulped down almost half a cup. Then he lay back to rest. Suddenly he was gasping for breath. And then he was gone.
I am numb. The aide gently repeats that Lou is not breathing. A convulsion of tears. I thought there were none left. Touching him. Taking his hand. Stroking his forehead. Kissing him. What do I do now? I am lost.
Call the hospice. They will send a nurse to sign the time of death. Call the funeral home. They will come. Then what? Vast emptiness. The rabbi calls and says I have to embrace life. Says that’s what Lou would want. Rationally I know he is right. Somehow, I will find a way. I just can’t imagine how.
This year, for our anniversary, June 27th, we had to cancel reservations at a restaurant with spectacular Manhattan views. Lou said it made no sense to go when he couldn’t eat much. He was devastated to disappoint me.
I said: “We’ll always have Paris.”
Complete Article ↪HERE↩!
Dying is a selfish business
Whether you are the dying person or the caregiver, living life to the fullest remains your goal, but somedays it’s just too darn hard. When you are so busy that it doesn’t seem you have time to take a breath, where does living life to the fullest fit into your day? It may just get a minute or two of your time but knowing that your life can change in a nanosecond may help you try just a little harder to fit life into your life.
Hug your child longer, spend a moment with a sunrise or a sunset, say “I love you.” Listen to the last notes of your favorite music on the radio before turning off the car, get out for a walk, or just water your plants and take a walk outside. All will help you seize the moments as they arrive. They are fleeting, so you need to pay attention. Living in the moment takes hard work and practice.
There are many challenges for the dying patient. Some are substantial and overwhelming. A caring physician trained in treating the dying patient may be the source for the best care for the patient. Many physicians are not trained in coping with the dying patient, and this can lead to many miscommunications and discomfort for both the patient and the doctor.
An understanding of the dying patient’s experience should help the physician improve their care of the terminally ill. These physicians are often known as palliative care doctors. The doctors specialize in medical care for people living with a serious illness. This care is focused on providing relief from the symptoms and stress of the illness. The goal being to improve the quality of life for the patient and the family. They can assist with the following six challenges that are common to the dying patient:
1. Pain. Pain and the fear of pain often make the patient’s behavior change at the end of life. Cancer patients rank “freedom from pain” as one of their goals for care. Even though the fear of pain is there, the elderly are often unwilling to report their pain because they believe it is a normal symptom of aging and that their pain is directly associated with the worsening of their illness.
2. Depression. The presence and severity of clinical depression often correlates with the severity of physical illness and, in some, a progressive inability to get out of bed. A decreased appetite may also suggest major depression. Anxiety commonly co-exists with depression, and it may be driven by fears of helplessness, a loss of control, abandonment, or pain.
3. Coping. Patients with advanced illness face the challenge of coping with their disease daily. While some patients demonstrate optimism, practicality, resourcefulness, awareness, and flexibility, others present with a variety of defensive styles in response to their diagnosis. These defenses can be denial and non-compliance, which can lead to a delay in treatment.
4. Dignity. For dying patients, maintaining dignity is foremost in their care, broadly defined in terms of being worthy of honor, respect, and esteem. For many patients, dignity is directly related to the level of independence retained through the course of illness.
5. The need for control. For some terminally ill patients, maintaining a sense of control is a central task of the dying process. This need for control is prominent among patients who request physician-assisted suicide (PAS) in Oregon. These patients were universally described as having strong personalities; they were determined and inflexible, and they wanted to control both the timing and the manner of their deaths.
6. Other aspects of the dying process. Dying patients and their families often must deal with complicated “practical” issues, such as financial problems and legal issues. These seemingly mundane concerns can cause a great deal of distress for dying patients and their families. It’s a good idea to take care of the difficult things while the dying person can make decisions. Wills, trusts, burial requests, and choosing a grave site can be taken care of while the person is well, so the decisions are not made after the death.
While nature is selfish, you don’t need to be. You might find that your best friend is yourself. You know when you need a hug or when it’s time to rest or try to appreciate the moment you are in. You also know when you are at the end of your rope and need to walk away, so things don’t blow up and get out of proportion.
There are five regrets the dying person often have when it is too late to do anything to change them. There is still time, if you can try and make some small changes now, so your regrets are fewer in the end.
1. I wish I’d had the courage to live a life true to myself, not the life others expected of me. This seems to be a very common regret when people realize that their life is almost over and look back on it. Many dreams when unfulfilled due to choices they made or did not make. When we are healthy, it’s hard to realize that a decision now, which we may only be allowed to make once, can change our life forever. Time may run short, and the chance won’t come up again.
2. I wish I hadn’t worked so hard. This regret is more common with men than women. Or it used to be. Since men are often the primary source of income, they regret what they missed while working. Time with children and spouse being the main regret. This is changing now that women are a strong force in the workplace. The working mother who has a child and goes back to work right away may eventually regret the lost time with the child as an infant.
3. I wish I’d had the courage to express my feelings. Suppressing one’s feeling to keep peace with others may result in a mediocre existence and prevent the person from becoming the person they were truly capable of being. Illnesses can result from this, and one may never realize the cause. Mental health is as important as physical health. Bottling up emotions and thoughts is hard on one’s psyche.
4. I wish I had stayed in touch with my friends. There are many deep regrets over lost friendships. Getting caught up in one’s day-to-day life makes it easy to let friends slip away. Waiting until the end of life is way too late to try and track old friends down.
5. I wish that I had let myself be happier. Many people do not realize that happiness is a choice. We get comfortable in the way we live our lives and don’t realize that happiness is easy to come by if we just work at it a little and let it in the front door. Fear of change makes people pretend they are happy, but truly they are not. A good laugh and some silliness won’t hurt anyone.
Complete Article ↪HERE↩!
End-Of-Life Workers Are Sharing The Major Things We Get Wrong About Death

The one big thing that people have in common is that we all will die, and we likely will experience the death of someone we love, too.
And yet despite this shared future, death can be hard to talk about, because it’s not an experience that anyone can report back from to say how it went. When you or a loved one starts approaching death, the existential stakes can go from theoretical to personal, sometimes feeling emotionally, physically and spiritually fraught.
That’s why it can help to hear the insights of people who see death all the time, because understanding it now can help us better process grief about others and feel more at ease when thinking about our own mortality.
I had conversations with palliative and hospice care physicians, nurses and social workers that comforted me, surprised me and challenged my own assumptions about death. Maybe they will for you, too.
Here are some of the biggest misunderstandings they shared with me about death and what the reality actually is:
The physical process of dying doesn’t look like it does in the movies.
This was a repeated theme among the experts I spoke with. Pop culture may have you thinking that death happens quietly and quickly, with eyes closing and arms crossed, but dying from natural causes often looks different in real life.
“My own dad said to the nurse, ‘I’m about ready to hang it up,’ and then he died minutes later. But that type of death is very uncommon,” said Penny Smith, a hospice quality manager and registered nurse in Washington state.
In her decadeslong career, Smith said she’s only come across a few instances in which people died quickly.
“It’s usually more of a process where they go into that unresponsive state, and there’s all kinds of things going on with their body. Their color’s changing, their breathing is changing and then they finally slip away,” she said.
Smith started posting TikTok videos about working in hospice care during the COVID-19 pandemic shutdown of 2020 and has since amassed around 640,000 followers on the platform. She uses skits and sound effects to educate people on what it’s like to be in the room with someone who is dying, covering topics like deathbed visions to the sounds that dying people make.
Common responses to her TikToks are comments of relief, acceptance and commiseration at seeing someone describe an experience that resembles how their own loved ones died.
“I, as a hospice nurse, have been with so many families where they were really disturbed by what they were seeing, or scared. And I would say: ‘That’s normal. We see that all the time.’ The relief is palpable,’” Smith said.
In one TikTok, Smith explains that when a person’s body is “shutting down,” it’s normal if they do not want water. A top comment on the video reads: “Thank you for this. My mom stopped drinking when we knew she was going to pass and I still felt like I should have tried to have her drink water more.”
Among all the physical processes of dying, Smith said the biggest misunderstanding she sees is when family members worry that their loved ones are dying of starvation because they’ve stopped wanting to eat.
“These are people who are already dying. They don’t need the food,” Smith said. “And when the family starts to try to force them or coerce them into eating just by, ‘Come on, just have a bite just to eat something,’ it just sets up so much stress between the family and the person.”
Similarly, families often worry that the use of morphine and other opiates will hasten the death of loved ones, according to Frances Eichholz-Heller, a senior social worker for the palliative care consult service at NewYork-Presbyterian/Columbia University Irving Medical Center.
“Some people will say to me, ‘Well, we had an uncle who was in the hospital dying, and then as soon as they put the morphine on, he died really quickly,’” Eichholz-Heller said. “I have to explain to them: ‘Well, he probably died really quickly because he was dying. He wasn’t dying because of the morphine, but they put him on the morphine to help.’”
Families can live with a lot of regret over what they should have done.
If you are seeking to support a loved one who is dying, be mindful of how your own fear and discomfort could impact what a dying person shares with you, said Dr. Aditi Sethi, a North Carolina-based hospice physician and end-of-life doula.
According to Sethi, some dying people try to talk about their experience with loved ones but the families dismiss it because of their own discomfort, using language like “You’re not dying, don’t worry about it.”
“So many times, loved ones have the most regret,” Sethi said. “They’re so terrified of losing their loved one that they can’t be fully present to their loved one at the time when they need them the most, really — to hold their hand and to really honor what they’re going through, and have a space to share what they’re experiencing in this epic journey they’re about to embark on.”
But if you had a strained relationship with the person before they were dying, don’t feel like you have to force a connection that is not authentic, either. “Your relationship with the dying person is personal, and if you didn’t have a good relationship, you are not obligated to go and be with that person,” Smith said.
It’s also important to provide space for people to be themselves when they are grieving, said Ladybird Morgan, a California-based registered nurse, palliative care consultant for the company Mettle Health, and co-founder of the Humane Prison Hospice Project nonprofit.
“I really ultimately believe that what happens is what needs to happen. And I see a lot of suffering for families that get left behind when they feel like they should have done something different,” Morgan said. “You grieve the way you’re going to grieve. You let go the way you’re going to let go. I tend to want to be careful about saying, ‘You should do X, Y and Z.’”
Not everyone wants silence or a somber mood when they are dying.
Health care providers and family members can make assumptions about what a dying person would find comfortable, without considering what that person truly enjoys. Some people may desire silence, but others may welcome raucous celebrations.
Smith recalled worrying about a football game party happening in the room of a dying woman until one of the patient’s adult sons reassured Smith that this was her passion.
″[The son] said: ‘Oh, my gosh, she was the queen of football parties every Sunday [with] everybody in the neighborhood. Yes, she loves this,’” Smith said. “I was new in my hospice career and making assumptions about what I thought a dying person would want. I thought they would want a quiet, dark room, and that’s not necessarily the truth.”
Not enough people plan or talk about how they want to die.
Most Americans say that given the choice, they would prefer to die at home, but about 1 in 5 deaths in the U.S. occur after admission to an intensive care unit. In the book “Extreme Measures: Finding a Better Path to the End of Life,” Dr. Jessica Zitter details what she calls the “end-of-life conveyor belt” — a type of care in which dying ICU patients receive painful treatments to be kept at alive at all costs.
“Unfortunately, by the time someone is on the conveyor belt, it’s often too late to talk to them about what they want. And then everybody is trying to play catch-up. And it’s hard to get it right when the chips are down and there’s so much emotion,” said Zitter, who specializes in palliative medicine and critical care.
“So my recommendation is to talk about these issues early on in life, maybe starting when you become an adult. Start to think about your mortality, and visualize how you would want things to go for you when you get into that stage of life, the end stage. Communicate honestly.”
“The people that I notice that have the least amount of distress are the ones … [who] have lived really fully, and that they can say to themselves, ‘I was here.’”
– Ladybird Morgan, a palliative care consultant at Mettle Health.
Filling out forms for so-called advance care planning goes a long way. But “it’s as important that you, number one, identify a person you trust — or two or three [people] — that can honor your wishes,” Sethi said, “and have the conversations ahead of time, before you’re in the state where you can’t communicate your needs and wishes.”
Some hospice workers recommended Five Wishes, an advance care planning program, as one way to get clarity on how you want things to go.
Morgan recommended playing a card game called GoWish with a friend, a partner or someone else you hope will follow your end-of-life wishes. “[The cards] have different statements on them about possibilities of what you might want or not want,” she said. “And you make stacks of the ones that you like, the ones that you know you don’t care about, and the ones that you’re not sure about.”
Someone playing the game may find it difficult to choose which cards represent their values, which is why Morgan suggests having two people play together, so that it can be a conversation starter.
Keep in mind that there is no one right way to die, and preferences may differ.
“There are people who feel that every moment of life is precious and that they value the length of life over the quality of life,” Eichholz-Heller said. “So they are willing to endure a certain amount of suffering to be able to be kept alive. Then there are other people who value quality of life over length of life. And they would rather focus on comfort, even if it means that they won’t live as long.”
There are still a lot of negative associations with hospice care, even though it can be helpful.
There’s a difference between palliative care and hospice. Palliative care workers help to make patients comfortable at any stage of their life if they’re suffering; hospice is a medical service specifically for people with a short-term life expectancy. While anyone living with a serious illness can seek palliative care, Medicare will help cover hospice care costs for people in the U.S. if their health care provider certifies that they are terminally ill and have six months or less to live.
Some people wrongfully assume that going into hospice automatically shortens the life of a patient. Smith said she has been called a murderer for working in hospice care, adding that the worst myth about hospice workers is that they kill their patients.
“People think that when you go on hospice, it’s a death sentence and that death is imminent,” Smith said. She cited former President Jimmy Carter, who entered hospice care in February and is still alive today, as one prominent example of how that is not always the case.
In fact, research shows that seeking palliative care at an early point can improve quality of life. Published in 2010, one study on advanced lung cancer patients found that offering early palliative care on an outpatient or ambulatory basis led to fewer clinically significant depressive symptoms and a longer median survival.
“When patients are suffering, they use so much of their energy just to fight the suffering that if we can make them comfortable, they sort of stabilize,” Eichholz-Heller said. “And a lot of times, it really helps them to live longer.”
Hospices can differ in their approach to care and the additional services they offer. There are resources that can help you figure out the right questions to ask to select the best hospice for you or a loved one.
We can’t control death.
There can also be a misunderstanding about the medical community’s ability to defeat death — even from health care workers themselves.
“The biggest misunderstanding that I see [among] patients, families and even health professionals around the issue of death is that we think we can control it,” said Dr. Solomon Liao, a UCI Health physician in California who specializes in palliative medicine and geriatric pain management.
“We believe that with all of our machines, technology and medications, we can determine when or even if that happens. Instead of accepting death as a natural endpoint of this life, we get depressed and even angry when it happens. We avoid planning for it or even talking about death, and then are shocked when it happens.”
The reality is that we can’t control death ― and we’ll all experience it at some point. “The people that I notice that have the least amount of distress are the ones — not so much that they’ve controlled every element, but that they have lived really fully, and that they can say to themselves, ‘I was here,’” Morgan said. “And people around them can honor that and acknowledge that like, ‘Yeah, we saw you, we felt you.’ … And that was so important for them, allowed a deep relaxing into what was coming next.”
At the same time, it’s OK not to be ready.
Morgan said many conversations around death and dying have focused on making sure someone is ready and not as much on cases in which a person loves life until the last minute and is not ready to go.
“It’s OK to miss life,” she said. She recalled talking to a client about how he knew everyone else was going to be all right after he died, and how that was heartbreaking for him.
In our conversations, hospice and palliative care providers suggested that it’s helpful to keep an open mind about death — leaving space for it to be “both and,” as Morgan told me.
Death can be devastatingly sad, but it doesn’t only have to be a somber occasion, as Smith’s TikTok skits show. Dying may be painful due to a terminal illness, but it’s not inherently so, Sethi said.
“It can be positive and hard,” Morgan said. “It can be, ‘It was exactly what needed to happen, and they had a beautiful death’ and ‘Wow, was that hard to see them go because I would’ve loved to have had them around for 10 more years.’”
Complete Article ↪HERE↩!
What Happens to Patients After Taking End of Life Drug

Many people might not like talking about end-of-life care or death until they’re faced with it themselves, but this hospice nurse wants to remove the taboo from the topic and educate people instead.
As an intensive care unit (ICU) nurse for over a decade, Julie McFadden, 40, focused on keeping patients alive, but when she made the switch to hospice care eight years ago, her attention turned towards making people feel comfortable as they neared the end.
McFadden, from California, regularly talks about the realities of hospice care, and what happens when a patient opts for medical aid while dying, on social media. She told Newsweek: “My main point is to make everyone a little less afraid of death. I want to change the way we look at death and dying.”
Medical aid in dying (also referred to as death with dignity, physician-assisted death, and aid in dying) is the prescribing of life-ending medication to terminally ill adults with less than six months to live, who are mentally and physically capable of ingesting the medication independently.
At present, only 10 states and the District of Columbia permit this process, but there is growing support elsewhere. A survey of over 1,000 people in 2023 by Susquehanna Polling and Research concluded that 79 percent of people with a disability agree that medical aid in dying should be legal for terminally ill adults who wish to die peacefully.
States where it’s permitted include Colorado, California, Washington, Hawaii, Maine, Montana, Oregon, and Vermont. Legislation is also being considered in Massachusetts, New York and Pennsylvania.
How the End of Life Drug Is Administered
As a hospice nurse in California, where a bill was passed to permit death with dignity in 2015, and became effective from June 2016, McFadden has assisted many patients who wanted to die on their terms.
She believes that there is real beauty in someone being able to have full autonomy over their death and choosing when they go, but she knows it’s a polarizing issue.
“People have to remember that not everyone has the same beliefs and I think it’s a beautiful thing that someone gets to have control over,” McFadden told Newsweek. “It’s powerful to witness someone be so alert, say goodbye to their loved ones, have their loved ones watch them take this drink and then die, but still be willing to be there to support them.
“I think most people in the U.S. have no idea that this law even exists, and even when I give very descriptive explanations of what the law is, what it means, what the criteria is, there’s still people who think I’m just overdosing patients with morphine.”
In order to acquire the medication, an individual’s request must be approved by two doctors, they have to undergo a psychological evaluation to ensure they aren’t suicidal, and doctors have to confirm that the person is capable of making their own decisions. Patients with certain conditions do not qualify, including those with dementia.
If approved, the person must take the medication themselves, and they can have family, friends, and hospice staff present if they wish.
Since June 2016, in California 3,766 death with dignity prescriptions have been written, and 2,422 deaths registered. To protect the confidentiality of any individual who makes this decision, death certificates usually note an underlying illness as the cause of death.
McFadden continued: “There are a few drugs mixed in, it’s taken all at once and the initial drugs kick in very quickly, within three to seven minutes. This person who ingested this drug will fall asleep or basically go unconscious. I say fall asleep just so people can picture what it looks like, but they’re unconscious.
“Then, the body is digesting and taking in the rest of the drugs that are also in that mixture, which will eventually stop the heart. It’s a general sedative and then they take two different cardiac drugs to stop the heart.
“They have a change in skin color and changes to their breathing, in what we call the actively dying phase, which is the last phase of life.”

People Have A Lot of Misconceptions
Regardless of whether you’re in a state that permits physician-assisted death or not, dying isn’t regularly talked about in a positive way.
One of the reasons why McFadden wants to have a more open conversation about it is to remove any prior misconceptions that people might have and educate them on what really happens.
“I have not seen anyone show signs of pain, but people are always concerned about that,” she said. “In general, if you’ve done this for a long time, if you’ve been in the healthcare system and work as a nurse or by someone’s bedside, you know what a body in pain looks like, it’s very obvious.
“A person who is unconscious and can’t verbally say they’re in pain will show you with their body language. Most people that have taken this medication who I have witnessed did not show those signs. I witness it day in, day out, but it’s pretty miraculous to see how our bodies, without even trying, know how to die. They’re built to do it.
“People get really angry and think I’m trying to hurt people. I always want to educate people around this topic, because the main thing people don’t want is for their loved ones to suffer at the end of life.”
As an ICU nurse formerly, McFadden explained to Newsweek that she was trained to keep patients alive, and they “didn’t have conversations about death early enough.” Despite patients being near death, they were kept alive through machinery for weeks or months, before ultimately dying on the ward.
Many of the country’s biggest medical associations are conflicted by death with dignity, with some choosing to endorse it, and others speaking against it. The American Public Health Association, and the American Medical Student Association are among the bodies to endorse it, but it has been publicly opposed by the American Medical Association and the American College of Physicians.

Talking Openly About Death
In 2021, McFadden set up her TikTok account (@hospicenursejulie) to speak openly with her followers about death and answer any questions people might have. Many of her videos have gone viral with millions of views, and while she does get a lot of positive feedback, there is also plenty of negativity.
There are people who wholly disagree with her advocacy for death with dignity as they claim she is playing God, or that she’s promoting suicide. But by having an open conversation, the 40-year-old hopes to make people less fearful of dying.
Speaking to Newsweek, she said: “Most of my audience is general public, that’s why I don’t talk like I’m speaking to other nurses or physicians. I talk like I’m speaking to my families who I talk to in everyday life. I think death just isn’t talked about, or it’s not explained well.
“I’m seeing so many times that people who are willing to have difficult conversations about their own death, who are willing to say they’re afraid to die, those patients who were willing to ask me those things and talk to me about death, had a much more peaceful death.”
Complete Article ↪HERE↩!
Planning to die at home?
— Here are 5 things to consider first.

Many of us say that if we have to die, we’d like to die comfortably in our home. Luckily, hospice—a Medicare-covered model of gentle, holistic end-of-life care—is ready to help with that goal.
Maybe.
by Laura Kelly
At age 78, my divorced father was diagnosed with Stage 4 colon cancer. He later admitted that he’d skipped getting any colonoscopies. He was a savvy healthcare researcher and, via drug trials, controlled the spread of his cancer for four long years. Then came the day his doctor said, “There are no more treatments left, Larry. Call your kids and sign up for hospice. Today.”
If you’re hazy about what hospice is, as my family was, check out Medicare’s hospice page that details the conditions that qualify you for hospice care and what costs Medicare will cover. You might also check out a 2023 New York Times article that sheds light on how hospice functions today. The industry has traveled far from its grassroots, volunteer origins of 40 years ago.
By the time I was flying from New York to Michigan to “help out,” my busy brother David had made the executive decision to move my father from his cluttered condo to David’s larger family home across town. My brother’s wife, 9-year-old daughter and three large dogs were no doubt a bit flummoxed when David deposited my hospice-unready father into the ground-floor master bedroom. But my father and everyone else were united in wanting the proverbial “good death” in the comfort of a home, even if it wasn’t his.
What happened during that home hospice experience surprised me. After it was over, I compared notes with friends. It seems that what my family went through might not be typical. Still, it could be a portent of what’s to come as the baby boomer bulge meets the realities of understaffed hospice care. Here are five takeaways if you’re ever considering home hospice for a loved one—or yourself.
1. Research hospice options before you need them
As my father and family found out, the very end is much too late to think about hospice—both for taking advantage of hospice’s full psychosocial benefits and for finding out what you’re getting into.
The hospice provider, which had been suggested to my father by his doctor’s office, turned out to be severely overstretched. We had only four short visits from a hospice nurse—a different person each time—during the 11 fraught days of my father’s end-of-life passage. It was also impossible to get the hospice doctor on the phone to answer our ongoing questions. Even so, we could never find the time to research and switch to another organization.
Since events can overtake you at the end of life, spend an hour today learning which hospice providers operate in your area. AARP keeps an excellent updated page with facts about hospice, including questions to ask when you interview organizations. Your future self will thank you.
2. Know what equipment and services to ask for
Beyond the electric hospital bed, rolling bedside table and plastic commode that the hospice group delivered, my brother’s home was not equipped for a dying person. Side note: At the intake meeting where we met with hospice nurse No. 1 and a social worker, we all agreed that the bed was much too short for my 6’4″ father. He requested a replacement, but one never arrived. We should have kept asking.
We quickly found ourselves making daily runs to a nearby Target for more towels, more large and small pillows for propping up, more pajamas, cooling patches, ice packs, a small table fan that my father could angle, sheets, blankets, sippy cups and dry-mouth swabs, plus an intercom because my father’s voice weakened too much to call for us in another room. My credit card got a workout.
3. Be prepared to hire help
As much as we tried to make my father comfortable, it seemed impossible. He was plagued by restlessness and couldn’t sleep or be convinced to stay in bed. Someone had to be near him around the clock to prevent a fall in his weakened state.
After six sleepless nights, we called the hospice phone line yet again with questions about the situation, and a nurse on the line finally filled us in on “terminal agitation,” a not-uncommon occurrence at end of life for cancer patients, even though no one in our family had heard of it. She told us that this kind of metabolic restlessness was worse than pain because it could not be soothed by painkillers. “Call us again if you need to,” she wrapped up.
By then, we realized that our home hospice team was mostly voices on the phone, not the on-site caretakers we’d expected. A concerned long-distance relative emailed me: “Get yourself some nighttime help so you can sleep.”
I had no idea how to find good health aides at short notice, but it turned out that “good” wasn’t the issue. We just needed someone to sit near my sleepless father, so we caretakers could get some rest. I also needed time to coordinate events outside of hospice, such as lining up a funeral home to call when my father died. In the end, I pretty much handed over my credit card to three different aide services to help us patch together 24/7 coverage until the end.
Will you need expensive additional aides for home hospice? Maybe, so be prepared by getting the names of aide services and interviewing them at the beginning of the hospice process, so they’re just a phone call away if needed.
4. Someone needs to be in charge
Continuity of care was a big problem for us and my father. There was a revolving stream of new hospice personnel and eight different aides, along with a churn of visits from nearby relatives and phone calls from folks farther afield. Meanwhile, every day brought changes and challenges as the end of life approached.
It took me far too long to realize that neither my father nor the home hospice team were running the show; I was. In unfortunate timing, during these hospice days, my brother had been pulled away to manage an ongoing crisis at his company. Still, every night, David remained on call to help me or an aide. He was the only one who could support my tall father as he restlessly moved from bed to nearby chair to commode.
Needless to say, my brother was exhausted. After another of these nights, I emailed my two sisters what came to be known as “the bossy note,” telling them exactly what was needed from them beyond the occasional visits bearing baked goods. It was all-hands-on-deck time.
I suggest that upon hospice enrollment or before, everyone should agree on a point person. This coordinator would have the overview of the home hospice situation, be given the latitude to set the ground rules and make decisions, and be allowed to delegate whatever to whomever, as needed.
5. Hospice at home may mean a nonprofessional will be in charge of medications
One of the hallmarks of hospice is the comfort care provided. On the first day, as I followed the intake hospice nurse on her way out the door with my list of anxious questions, she stopped me by handing over what she called a “comfort box.”
I pried open the white cardboard box and saw a confusing array of vials, syringes and suppositories. I thrust the box back toward her. “This is all for you to use, right?”
“No, they’re for you,” she said. “If your father needs them, you can call us. Put the box in the refrigerator where you can find it fast.” Then she left.
I immediately regretted that I didn’t ask her to go over each and every medication and how to use it, recording her explanation using my cellphone.
Later on, when I hired the aide services to help us through the final days and nights, I found out the aides weren’t allowed by their companies to prepare the needed antianxiety and sedative medications, and they could only give them to the patient when directed by someone in charge, meaning me. If I wasn’t awake to direct them, my father wouldn’t get his comfort meds.
As my shaking hands prepared morphine syringes and crushed Ativan pills in the middle of the night, I thought, “I would never expect or want someone like me to do this for me.”
My advice: When you’re doing those early interviews with prospective home hospice providers, ask who will actually dispense the medications. Maybe you’ll find out the home hospice nurses will be there to do it. But in our case, they weren’t.
My father died on Oct. 25, 2015, after his 11 days of home hospice care.
Was it the good death my dad had hoped for? I’ve never shared this with my siblings, but I don’t entirely think it was. My father had always prided himself on being the problem solver, not the problem maker. While we tried to hide our distress, he couldn’t help but notice how unprepared his kids were to supervise this 24/7 medical undertaking.
One late night, as I lay awake on the king bed beside my restless father in his little hospital bed, he told me he was sorry about “all the trouble I’m causing,” as he put it.
“I didn’t imagine it would go like this,” he said quietly. “No help. No sleep. Not knowing what’s coming next. Thank you for everything you’re doing.”
I reached over and touched his hand. “Dad, I am so grateful to be here helping you through this after all you’ve done for us. Please don’t apologize. You’re no trouble at all.”
Later, I heard friends’ stories of their supported and peaceful experiences in dedicated hospice facilities. There, they could quietly share smiles and good memories, listen to music, even be served meals. A facility can perhaps more easily arrange quality-of-life options for the patient, such as expert bathing and therapeutic massages with oils. Most important, a facility would presumably be staffed with professionals who could administer the proper palliative medication. A place that’s designed and intended for end-of-life care clearly has some advantages.
If, however, you’re with the majority who would prefer using hospice in a familiar home setting, look into what’s entailed well ahead of time. Ensure that family or friends are willing and able to coordinate all the activities and decisions. Have a credit card ready for all the purchases and extra help you may need. And don’t make hopeful assumptions, as I did. Be proactive and ask the necessary questions, so you or your loved one gets the quality end-of-life care all of us deserve.
Complete Article ↪HERE↩!
Does a Person Know When They Are Dying?

Family members and friends of a dying loved one may wonder if the person knows they are dying. They may worry that if their loved one doesn’t know death is near, telling them might dash any hope and even make them die sooner. Here’s how to recognize the signs that someone is close to dying and why it is ok to acknowledge it.
The Important Tasks of Dying
It is natural to want to shield the ones we love from pain and sorrow. Trying to protect a loved one from the truth about their condition may initially seem like a good idea, but in fact withholding that information can lead to resentment and disappointment.
When a person knows they are dying, they have the opportunity to do five important things:1
- Apologize for past mistakes
- Forgive others for their mistakes
- Thank those people who matter most
- Say “I love you” to those they love
- Say goodbye
Without the opportunity to do these valuable things, your loved one could die with unfinished business.
Hope at the End of Life
It may seem like a dying person can’t possibly feel hopeful, but dying people do retain an amazing capacity to hope. While they may have stopped hoping for a cure or for a long life, they may still hope to mend relationships with loved ones and to die peacefully.
Keeping the truth about dying from the one who is nearing death could rob them of the chance to reflect on their lives and fulfill their final wishes.
Signs That Death Is Near
As someone nears the end of life, they usually experience certain specific physical and mental changes, including:2
- Fatigue or sleepiness
- Refusing food and drink
- Mental confusion or reduced alertness
- Anxiety
- Shortness of breath or slowed or abnormal breathing
- Hands, arms, feet, and legs that are cool to the touch
At the very end, the eyes may look glassy and the person may breathe noisily, making a gurgling sound known as a “death rattle.”
Awareness May Linger
It isn’t clear how long a person who is dying retains awareness of what is going on around them, but research suggests that some degree of awareness may remain even after the person slips from unconsciousness.
A 2014 study looked at 2,060 patients from 15 hospitals in the United Kingdom, the United States, and Austria who had been given CPR after going into cardiac arrest (in which the heart stops completely). Of those who survived, 140 were surveyed about their near-death experiences. Thirty-nine percent reported feeling some kind of awareness before their heart was restarted, but did not have an explicit recall of events.3
Often, people will lapse into a coma before they die—a deep state of unconsciousness and unresponsiveness. People in a coma may still hear people talking even when they can no longer respond. Because of this, the Hospice Foundation of America suggests that caregivers, family, and physicians should behave as if the dying person is aware of what is going on and is able to hear and understand voices.2
A 2020 study that investigated hearing in palliative care patients who were close to death provides evidence that some people may still be able to hear while in an unresponsive state. Electroencephalography (EEG) was used to measure the dying brain’s response to sound. The findings suggest that telling a person you love them in their final moments may register with them.4
They Know They’re Dying
Dying is a natural process that the body has to work at. Just as a woman in labor knows a baby is coming, a dying person may instinctively know death is near. Even if your loved one doesn’t discuss their death, they most likely know it is coming.
In some cases, the person comes from a culture or a family in which death is simply not discussed. Furthermore, your loved one may sense that others feel uncomfortable recognizing the dying process so they don’t want to bring it up.
Death can then become the elephant in the room. Everyone knows it’s there but no one will acknowledge it. Family discussions may be awkward and superficial and never reach an intimate level. In this case, the important work of mending and completing relationships may not happen.
Talking About Dying
Talking about death is rarely easy. Many of us feel uncomfortable even saying the words “death” or “dying.” Talking about it with a loved one who has been diagnosed with a terminal illness can be especially awkward.5
First, remember that you are talking to someone who is still living, and that talking about memories and shared experiences honors the dying person’s life. Experiencing sadness with the loved one is appropriate; that’s part of life, too.
If necessary, a therapist or hospice social worker with experience in this area can make these conversations easier.
Frequently Asked Questions
What does dying feel like?
While we can observe another person’s death and perhaps imagine what it feels like for them, there is no way to know what it actually feels like to die.
What are the signs that death is near?
Someone who is very close to death will likely refuse food and water. Their breathing and heart rates will slow and/or be abnormal and their hands, arms, feet, or legs may be cool to the touch. They may also be agitated, anxious, and confused.
What should I say to someone who is dying?
There is no right or wrong thing to say to a dying person. You may want to share memories or make sure your loved one knows you love them. A therapist or hospice social worker can help make conversations about dying easier.
What are the five stages of death and dying?
According to one widely-accepted theory, originally conceived of by psychiatrist Elisabeth Kubler-Ross in 1969, the five stages of coping with realizing you are going to die are denial, anger, bargaining, depression, and acceptance.6
Some Final Thoughts
As uncomfortable as it can be to acknowledge openly that a person you love is dying, it’s important to realize that the person is most likely aware that they are dying, so you don’t have to struggle with “breaking the news.” In fact, dying people often appreciate being able to use the time they have left to tell people they love them and mend certain relationships if necessary.
Complete Article ↪HERE↩!
When disease ravaged her body, Sara was crystal clear about what she wanted.
— Here’s what she chose to do

By Nina Rota
A man from the home care agency calls on a Monday morning. “The caregivers are complaining. It’s too hard to transport Sara, to move her from the bed to the wheelchair and onto the stairlift. You need a lift or some other assistive device.”
A rush of sadness settles into my body. The end has arrived. “Sara is leaving on Friday,” I say, “Can we hold out till then?”
“Oh,” he says, and pauses, “I’m so sorry to hear this.”
My partner, Sara Flint Greenberg, was nearing the end of her nine-month journey through amyotrophic lateral sclerosis, more commonly known as ALS or Lou Gehrig’s disease, and she would take her life on Friday.
There is nothing more we could do. Her body has been ravaged by this devastating disease and she has been crystal clear, from the beginning, that she would leave when she can no longer take care of herself.
There are steps to the end of this journey.
Later that Monday morning, Sara speaks with a doctor, answering some required questions. Does she have less than six months to live? Is she mentally capable of making the decision to end her life? Can she self-administer the medication? Luckily, the session is short. Sara spends much of her day on a machine which helps her to breathe. Too much talking leaves her gasping.
On Wednesday morning Sara speaks with a second doctor who agrees that she qualifies to receive medications that assist in dying under the requirements of the California End of Life Option Act. The medication that will allow Sara to leave will be ready on Friday.
On Wednesday afternoon we celebrate our wedding. Sara and I marry in the late November light of our living room. I am not strongly attached to marriage, but as the day of Sara’s passing drew closer, I felt an overwhelming need to express the beauty of our love in ceremony.
The temporary chuppah is held over our heads by Sara’s sons Aaron and Jacob, our friend Audrey and a caregiver. We have found an independent rabbi to marry us because I am not Jewish. The rabbi is adorable in her Converse sneakers, covered with stars, as she takes us through this bittersweet ceremony. The ceremony is short because Sara is exhausted. It is her last gift to us, her family.
On Friday morning, our friend Margaret arrives from New York, kisses Sara on the cheek and tells her she loves her. It is all anyone can do. Audrey is in the kitchen. She has been with us for days, helping us through.
Later in the morning, a rabbi from our synagogue arrives to help us say goodbye to Sara. Margaret and Audrey go downstairs to wait. They sit, mostly silent and sometimes hold hands. The room feels heavy. They can hear Sara breathing above them, but they know she will not be there for long. It is one of the most reverent acts of love: to witness in silence the death of another.
At noon, Sara takes a pill to prevent nausea and vomiting when she takes the medication that will end her life. I sit beside her on the couch, Aaron is at her feet and Jacob is across from her. The rabbi is just beyond our circle as he begins to guide us through our final words. Everything is said on the edge of tears. We listen closely to hear our soft voices.
Sara regrets, deeply, that she will never see her grandchildren. She will not see her sons grow further into their lives or settle down with partners and start families. She gathers her breath and questions them closely because this is her last chance. She wants to know what their futures looks like because she will not be there.
There are apologies because anything left to be said has to be said. Death demands it. We make promises because who would say no? Sara would do anything for her sons and I promise to do the same. We celebrate Sara’s bravery. She left a longtime marriage, late in life, and jumped into love with me. And the bravery she shows today in making this choice.
The rabbi asks Sara where we can find her after she’s gone. “Walking in these hills,” she says, of the land surrounding our home where she once walked every day. She is now struggling to breathe and is silent. We are left with silence and the presence of love. We will carry this love everywhere we go.
It is almost an hour after Sara took the anti-nausea pill. She must take the medication now or wait for another day. The hospice nurse has not yet arrived. We call our hospice provider. They tell us to mix the medication with apple juice and give Sara sorbet because the taste can burn her throat. Sara reaches for the medication with both hands. She is ready to leave.
As the medication moves through her body, she prays in Hebrew: “HaShem Sheli, HaShem Sheli, ya’azor li” (“My God, my God, help me”). She recites the Shema, a centerpiece of prayer services in Judaism. As she draws closer to leaving, her last words are “Thank you, thank you,” a beautiful sentiment and a sign, I hope, that she is at peace.
Sara slides slowly down the couch, her cheek resting against the back of my hand. I feel life in her body, but after half an hour I am not sure. The hospice nurse has arrived. I ask him if she has passed. No, she is still here. Another half hour and I ask again. He checks her pulse. She has left.
My beautiful Sara is gone.
Complete Article ↪HERE↩!
