
Nearly a decade ago, David Modersbach had what he thought was a straightforward question: How many unhoused people had died that year?
The grants manager and his team at Alameda County Health Care for the Homeless knew people were dying on the streets, but they wanted more than anecdotal evidence; they wanted data that could show them the big picture and help them hone their strategies.
They queried the coroner’s bureau and were stunned by the response: only a single death had been reported.
“We realized there’s a lot of work to do,” Modersbach said.
What followed was a bootstrap campaign to fill the data gap. It took years, and the work was sometimes lonely, often tedious and consistently heartbreaking. When the team finally released its first report in 2022, detailing deaths from 2018–20, they counted 195 people in Alameda County who died while homeless in 2018, plus another 189 people with recent histories of homelessness whose housing status couldn’t be verified at their time of death.
As more Californians have fallen into homelessness — a number greater than 181,000 at last count (PDF) — more have died while unhoused, but the state’s ability to track these deaths and assess the scope of the problem hasn’t kept pace.
Spurred in part by Alameda County’s efforts, which are considered a national model for the field, the state recently began taking steps toward collecting this data. In 2022, California added a field to death records for homelessness status, and this year, a law went into effect that empowers counties to set up homeless death review committees to determine the root causes of homeless mortality.
California is among several jurisdictions across the country seeking this data. The pandemic put a spotlight on the health vulnerabilities accompanying homelessness, and that has led to growing national interest in the topic, said Barbara DiPietro, senior director of policy for the National Health Care for the Homeless Council. A recent study from researchers at the University of Pennsylvania and NYU found the death rate of people experiencing homelessness increased 238% between 2011 and 2020.
“One of the things that hopefully we took away from COVID is that homelessness is a public health issue,” she said. “Not only is living unhoused very dangerous and high risk for people experiencing homelessness, this isn’t good for communities either.”
Researchers said the data is critical in assessing whether the state’s public health interventions for people on the streets work.
“That is how we work to change things,” said Dr. Margot Kushel, director of the UCSF Benioff Housing and Homelessness Initiative. “One of the problems with not reporting it is that it makes it harder to act.”
But getting statewide — let alone national — data detailing the number of unhoused deaths requires meticulous reporting on the part of local agencies. In the case of Alameda County, it was a system Modersbach had to build from scratch.
How they count
For each homeless mortality report, Modersbach and his colleagues first scour thousands of county death records, searching for clues that suggest homelessness: words like “encampment,” “tent” and “shelter.” They then cross reference that list with a database of everyone in the county who has experienced homelessness in the past five years — itself a bespoke repository that draws on the agency’s healthcare data and records from the county’s shelter and homeless assistance programs. To capture anyone they might miss, they cull information from service providers, media accounts and a public online portal for submitting tips about deaths.
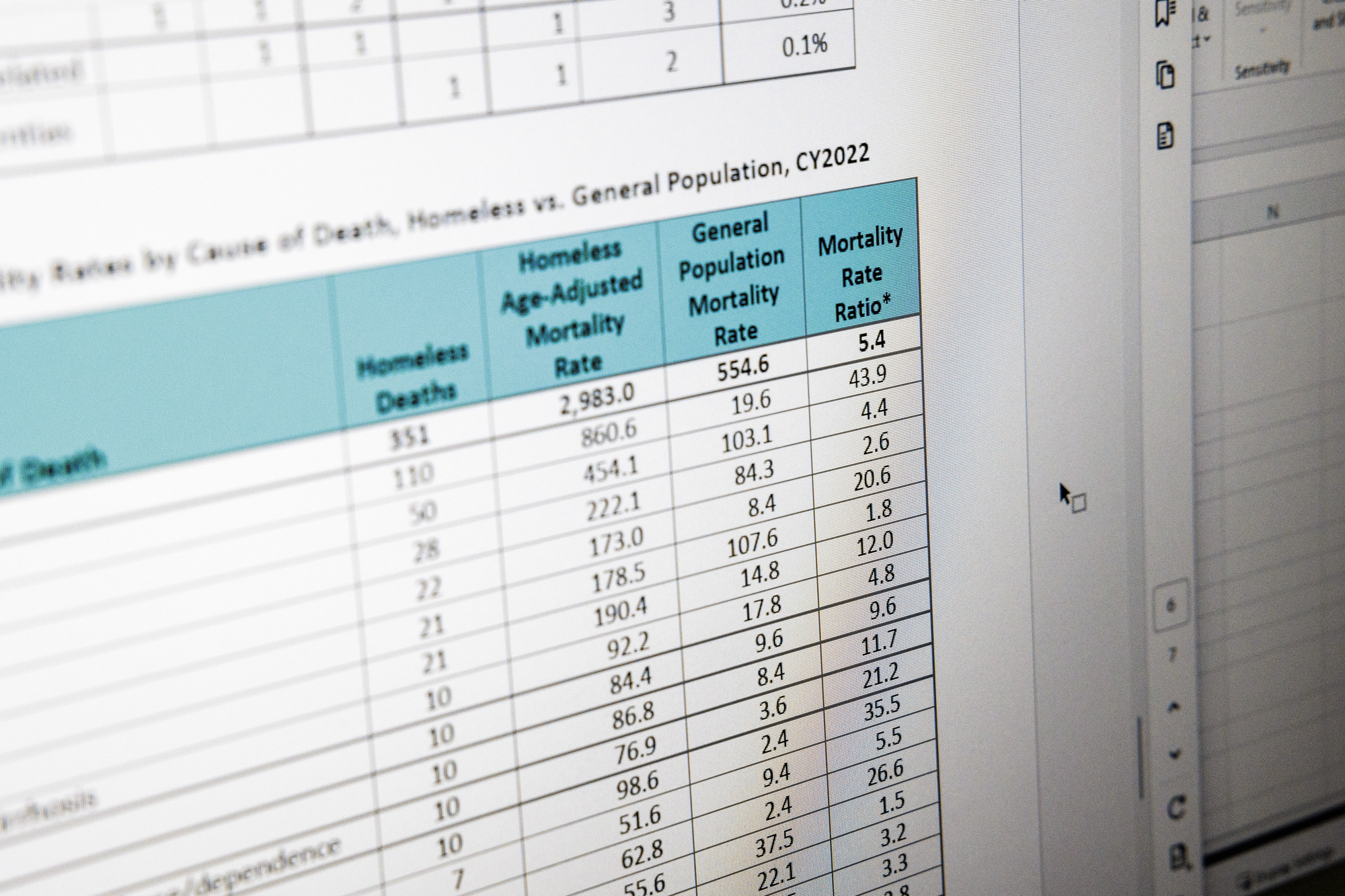
Since they began tracking homeless mortality, the team has traced an 80% increase in the number of deaths, which rose from 195 in 2018 to 351 in 2022, the most recent year for which data was reported. Over the same period, homelessness in the county jumped by nearly the same amount — or 77% — from 5,496 people to 9,747.
Behind the numbers are snapshots of how and where people are dying. A body found in a car. An overdose at an encampment. People mangled by cars or trains; others charred. Modersbach finds the tableau at once unsurprising and shocking.
“We see the same inequities in our mortality data that are reflected in homelessness,” he said. Black people are overrepresented, comprising 48% of the unhoused population and accounting for 44% of the deaths — though they represent only 19% of deaths in the county’s general population.
People who are unhoused die at five times the rate of those with housing and do so more than two decades sooner — at an average age of 52.
The data shapes decisions
Most of the deaths could be prevented, said Amy Garlin, Medical Director for Alameda County Health Care for the Homeless.
“You could say almost all of these deaths are preventable if you go far enough upstream,” Garlin said.
The largest share, 44% of the deaths among the homeless population, were caused by acute or chronic medical conditions, like heart disease, cancer, diabetes and infections. Some of those appear to have been more immediately avoidable, Garlin said. “If these people had had medical care, they may not have died this year.”
At an encampment along East 12th Street in Oakland, Angel Gonzalez, 40, remembered the friends he’d known there who had died. An asthma attack claimed one, exposure another and a third succumbed to a fever. Though Gonzalez said he didn’t know what had caused the fever, he said people are often sick, and rat bites are common.
“Health-wise here, it’s bad,” he said.
There’s frequent violence, too. Gonzalez described a drive-by shooting that killed one friend and wounded others. But what claims most people in the camp, he and others said, is overdoses.
“The fentanyl is killing mostly everybody,” Gonzalez said, explaining that people unwittingly use fentanyl-laced meth or other drugs. “It’s kind of scary.”

The mortality data compiled by Modersbach’s team reflects this, with an alarming rate of overdose deaths among unhoused residents that is 44 times the general population’s. In response, they’ve expanded their harm reduction services, focusing on naloxone distribution and installing dispensers in shelters.
At the East 12th Street camp, Gonzalez pointed out a purple dispenser on the street corner. Though Modersbach’s team had not installed it, it still proved lifesaving, Gonzalez said, when a friend recently used one of the naloxone sprays to reverse an overdose.
Alameda County Healthcare for the Homeless received a grant from the Centers for Disease Control and Prevention in 2023 to fund overdose response, a key part of their strategy to reduce mortality, and Modersbach credits their data for helping them get it.
In Minnesota, the only state with a statewide robust system for tracking homeless mortality, public health officials took a similar approach. A report on deaths between 2017 and 2021 showed unhoused people in the state were 10 times more likely than the general population to die of an overdose. Shortly after that data was released in 2023, state lawmakers passed drug overdose prevention legislation that expanded harm reduction and housing programs for people experiencing homelessness, decriminalized drug paraphernalia — a first for the U.S. — and funded “safe recovery sites” that offer clean needles, fentanyl testing and will eventually offer supervised drug consumption.
“Having the data was really useful in making the case for some of those things, both with legislators and with the public and advocates,” said Josh Leopold, senior advisor on health, homelessness and housing at the Minnesota Department of Health.
Alameda County’s latest homeless mortality report is now prompting the team to focus on how to extend palliative care services to unhoused people with terminal illnesses. Garlin estimates almost one-fifth of those who died in 2022 would likely have been eligible for hospice care.
What’s next in the ‘labor of love’
Modersbach’s team is also working to automate the most tedious aspects of compiling the county’s homeless mortality report and aims to launch a public dashboard later this year that will make information available quarterly.
“The biggest challenge is that we do not have timely data that we can act upon more quickly because of the workarounds that we have to do to get an accurate count,” Modersbach said. “We’re almost always looking backwards.”
The county’s latest tally, for 2022, was released at the beginning of 2024.
Santa Cruz, San Diego, San Mateo, Sacramento, Los Angeles and San Francisco are among the counties with varying degrees of reporting on homeless deaths. In Santa Clara County, an early champion of this work, a public dashboard tracking homeless mortality is updated nightly. A spokesperson for the Medical Examiner’s Office credited its partnership with a third-party vendor with allowing it to return results so quickly. So far this year, the dashboard listed 51 deaths.
Across the country, about two dozen jurisdictions have homeless mortality reports that are issued with some regularity, according to DiPietro of the National Healthcare for the Homeless Council, which tracks these efforts. But because the reporting isn’t standardized, it’s difficult to draw comparisons between them, she said.
In California, despite the recent efforts to improve this tracking, limited resources will likely continue to hamper the reporting of homeless deaths. Since 2022, when the state added a field on death reports to indicate a person’s housing status, Modersbach has seen some evidence people are filling it out, but he worries many unhoused deaths will continue to go uncounted around the state because the funeral directors, coroners and physicians filling out the reports don’t often have the resources to determine whether someone was housed.
“This is a lonely, costly battle to just put all this information together, not a funded mandate,” he said. “It’s kind of a labor of love.”
In counties with well-established systems for tracking these deaths, Modersbach hopes AB 271, by Assemblymember Sharon Quirk-Silva (D-La Palma), will make a difference. The new law allows counties to create homeless death review committees and access sensitive information about people who died. The data, which includes medical, mental health and criminal records, goes beyond what Modersbach and his team have so far been able to collect, giving them greater insight into the circumstances surrounding a person’s death.
Alameda County assembled its death review committee last year, bringing together officials from several county agencies, homeless service providers and formerly unhoused people with the aim of finding ways to keep more people experiencing homelessness alive.
“It’s just getting started,” Modersbach said, “but this is the future for us.”
Complete Article ↪HERE↩!
My advice for terminally ill Latinos like me
— You have options

By Jose Alejandro Lemuz
I am dying from prostate cancer that has spread to my bones.
But it’s comforting to know that I will likely soon die gently because I plan to use a medical aid-in-dying law championed by civil rights icon Dolores Huerta.
Thanks to the California End of Life Option Act, I will soon have the option to take a medication prescribed by my doctor that will allow me to die peacefully.
While I understand why my doctor wanted me to undergo more treatments, at this point in the rapid progression of the disease, the costs outweigh the benefits for me. Doctors should consult with patients about their care, not dictate it. Only I can determine how much suffering I can endure.
Less than three percent of the Californians who used the law in 2022 were Latinos, even though we represent 40% of the state’s population, and polling shows 68% of Hispanic Californians support medical aid in dying.
I suspect this disparity is because we have unequal access to this end-of-life care option because of healthcare system bias, cultural differences, and/or language barriers. I am a low-income body shop mechanic who does not speak English. My family doesn’t even have money for my burial.
Shamefully, I had to learn about this law through YouTube videos of a young Puerto Rican man, the late medical aid-in-dying advocate Miguel Carrasquillo, and TV news stories, instead of through my own doctors.
‘No More Treatment’
In December 2023, three months after trying to start the conversation about medical aid in dying with my healthcare team and after I had already endured numerous rounds of treatment since my diagnosis in 2018, I told my doctor:
“I don’t want any more treatment, I want you to respect my decision and I want you to help me. I’m asking that you declare me at the end stage because you’re the one who knows the treatment isn’t working for me anymore.”
I repeatedly asked my oncologist to estimate how long I have to live.
She declined to give me a prognosis. I showed my doctors a web page about this end-of-life care option to prompt the conversation with them.
They responded, “No, not yet…Keep taking more chemo.”
‘I Have Options’
I kept telling my doctors: “I have options.”
Why did my doctors not advise me about my healthcare options at the end of life, including my right to decline medical treatment for this incurable illness?
Hospice
For five years, I endured treatments to try to cure the cancer so I could work to provide for my two children and enjoy life.
Not anymore.
Last week [March 10], my doctors finally placed me in hospice care that focuses on alleviating some of the pain.
I am tired. I am weak. I have had a fever and convulsions for days. My frail and thin body can no longer withstand more than just a few steps.
Suffering is like being tortured.
Cancer consumes you little by little.
Unfortunately, the hospice care I am getting does not significantly reduce my suffering, so I will soon get the medication that will relieve me of this pain so I can die in peace.
I have spoken to God and asked Him to forgive my sins throughout my life.
I have talked to my children.
They understand and they support my decision.
They know it is my time to go.
Complete Article ↪HERE↩!
New Zealand’s ‘coffin clubs’ bury taboos about death
By Ryland JAMES
It’s a task of grave importance, but there’s nothing to stop New Zealanders having a laugh as they work on DIY caskets in the country’s “coffin clubs”.
Elderly club members meet for cups of tea, a bit of banter, and to literally put the final nail in one-of-a-kind coffins that will carry them to their eternal resting place.
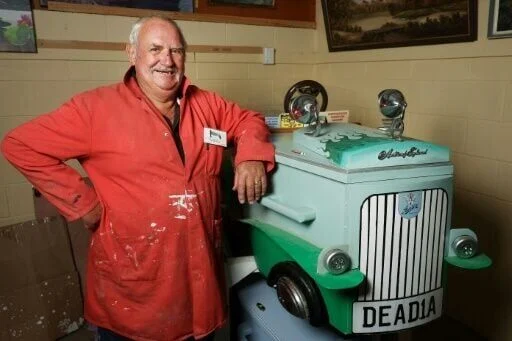
Kevin Heyward plans to be sent off in a box resembling a vintage Austin Healey.
Registration plate: DEAD1A.

“My daughter came up with the idea,” the 79-year-old car enthusiast said with a grin, brushing sawdust off his overalls.
It’s fully equipped with a mock steering wheel, windscreen, rubber wheels with metal hub caps, wooden mudguards, a bonnet, painted-on side doors, and wing mirrors.
“The trickiest part was getting the mudguards lined up because of their curve,” Heyward told AFP at the workshop of the Hawke’s Bay Coffin Club in Hastings.
The hefty casket, which can be carried with six wooden handles, even has working headlights. The batteries, naturally, are currently dead.
“It weighs quite a bit and I’m a big man,” he said.
“I have said to my six grandsons they had better start weight-training, because they will be carrying it one day,” Heyward chuckled.
“There is a bit of humour in this car.”
The club is one of four that have sprung up around New Zealand, with the first opening in 2010 in Rotorua on the country’s North Island.
Some clubs boast as many as 800 people on their books, though one admitted “not all of them are above ground”.
At the Hastings club, Jim Thorne, a spritely 75-year-old motorcycle fan, used his skills as a cabinet maker to build a casket painted with a motorbike track. It’s stored in his garage, alongside a collection of motorbikes.
Thorne said most friends “are a little aghast and say ‘why are you doing that?'” when they hear about his coffin-making hobby.
“Apart from the fact that I like the look of mine, it’s my input into my final days.”
– ‘Dying to get a coffin?’ –
“There is a certain mindset in some people that this is almost a taboo subject that they find very, very difficult to talk about,” Thorne said.
“They tend to overcome it. At the end of the day, it’s a reality of life, unfortunately.”

He breaks the ice with newcomers by asking: “Are you dying to get a coffin?”
But the club’s atmosphere is far from morbid.
Banter flows during the morning tea break as members chat over scones and hot drinks.
“We’re a bit unique, but we are happy. There are always lots of jokes,” said club secretary Helen Bromley.
Most members are seniors. The club provides a space to open up about death and dying during weekly meetups.
“I think everybody here has accepted that they are going to die, whether they’re decorating their coffin or helping others with theirs,” Bromley said.
“We’re a club that tries to empower people to plan their coffin, to plan what happens if they get sick.”
She said some members want to spare relatives the burden of meeting rising funeral costs. The club will also build and decorate coffins for grieving families.

On average, a funeral in New Zealand costs around NZ$10,000 (US$6,200), according to the national funeral directors association.
Coffin prices range from NZ$1,200 to NZ$4,000.
– ‘Remember Me’ –
For a NZ$30 membership, the Hastings club gives each new member a pressed-wood coffin in one of three designs, ready to be decorated.
The coffins come in four sizes, each costing around NZ$700, extra for paint and a cloth lining.
During a tea break, Bromley announced that a member suffering from cancer was in intensive care after a fall. Her brother had asked the club to finish her coffin as a priority.
The club also builds ash boxes, which they sell to the local crematorium, and small coffins for infants, which they give away.
“The midwives and nurses at Hastings hospital have asked us to not ever, ever stop making the little coffins for them,” Bromley said.
“We donate to whoever. If there’s a miscarriage at home and they want a coffin, we donate.”
Members help knit blankets, teddy bears, pillows and hearts to go in the infants’ coffins.
Committee member Christina Ellison, 75, lost an infant daughter in 1968 and said she was comforted to know the club helps other families grieving the loss of a child.
“The little baby coffins are so beautiful and done with so much care. The knitting that the ladies do is incredible,” she said.
Ellison is moving away soon and plans to take her coffin, which has been painted a blue-grey colour called “Remember Me”.
Complete Article ↪HERE↩!
All pets go to heaven.
— She helps them do it at home.

Veterinarian Karen Meyers pulls her black minivan into the driveway of a townhouse in Maryland’s National Harbor. The home, in a gated community, is perched on a windy bluff not far from restaurants, bars, a casino — places of revelry.
The vet carries her brown doctor’s bag inside. There, she meets her patient: Xochitl, known as Xochi, an 11-year-old boxer-Great Dane mix weighing around 80 pounds.
Xochi, recently diagnosed with cancer, is struggling. A film covers her right eye. She had been bleeding from her mouth, refusing to eat. Now she stands in the townhouse’s living room, mournfully greeting family members who have come to say goodbye.
Xochi climbs onto the living room’s leather couch and lies down. Owner Eden Gaines and her family gather around her. Meyers opens her bag.
Meyers explains the procedure. First, Xochi will be injected with a sedative to make her fall asleep. Five to 10 minutes later, Meyers will administer sodium pentobarbital, which will euthanize her. But Xochi would feel no pain, Meyers assures the family.
She asks whether anyone has any questions.
No one does.
“Here we go,” she says.

Pet adoption spiked during the pandemic, with nearly 1 in 5 American households taking animals in and spending far more on them than pet owners did decades ago. With more beasts in our lives — as companions, as emotional support animals, as the beneficiaries of pet trusts — it only makes sense that their owners want their final moments in their lives to be as peaceful and painless as possible.
That’s where Meyers comes in. Working with Lap of Love, a company that provides veterinarian referrals for at-home pet euthanasia, she travels from house to house in the D.C. region offering grieving families’ animals what the word euthanasia means: “good death.” In four years, she has euthanized 1,500 animals: cats, dogs, rabbits, rats. Some had been with their owners since childhood. Some had traveled the world with them. Some were their owner’s sole companion.
Meyers has observed death rituals that include praying, burning incense, wrapping a deceased pet’s body in a white sheet, and opening a window for a pet’s spirit to exit. She has listened to owners read poems or letters to their pets and cried along with them.
“When people hear what I do for living, it sounds sad,” Meyers says. “But it’s strangely rewarding. … You give pets a peaceful experience. It’s a final gift.”< Meyers has been surrounded by a menagerie all her life. Growing up, she usually had a dog and one or two cats; at various times, she’s also had two hamsters, two turtles, a guinea pig, a bird and four chickens. Right now, she has Wren, a 6-year-old Cavalier King Charles spaniel; Travis, a 3-year-old pug; Brinkley, a 13-year-old rat terrier Chihuahua; and Pablo, a red-belly parrot. Right before the pandemic, Meyers decided to shift to doing euthanasia full time. She had been a veterinarian for more than two decades, and pet euthanasia turned out to be less stressful than working in an office while raising two children. In-home euthanasia can be easier on animals and their owners than office appointments with other sick animals and their distressed owners crowded around.


Meyers administers the first shot in Xochi’s back. The dog, already lying down with her head on Gaines’s lap, turns to glance at Meyers as if mildly annoyed.
Then, the dog relaxes.
Minutes pass.
Using a hair clipper, Meyers shaves an inch-long strip of one of Xochi’s legs and inserts a small IV line. After confirming that the family wants to continue, Meyers administers the second shot, the one with the fatal dose.
Gaines looks at the spot on Xochi’s leg where the IV had been inserted.
“It’s amazing how gray she became,” Gaines says.
Meyers holds a stethoscope to Xochi’s chest. “Xochi has her wings,” she says.
The family cries.
So does Meyers.
She and Gaines embrace.
Meyers maneuvers Xochi onto a stretcher and covers her with a blanket. With the help of Gaines’s sons, she loads the dog into her car. Eventually Xochi will be cremated and her ashes returned to the Gaines family.
Death is a part of life, Meyers says.
“Many times, people will comment how a human family member passed, and it was so painful at the end, and this is peaceful by contrast,” she says.
They tell her, she says, that they wish they could go the same way.

Complete Article ↪HERE↩!
Asian Elephants display complex mourning rituals similar to humans

Elephants are smart animals with strong feelings and they often work together. In India’s Bengal area, scientists found that elephants buried five baby elephants, according to a study published in the Journal of Threatened Taxa.
Researchers have limited the study of elephant thanatology—the examination of death and related practices— to the burial of calves. Observers had noted this aspect of behaviour in African elephants but had not documented something similar in Asian elephants until recently, despite both species diverging 4.2 million years ago.
The researchers wanted to clear up the second question – do Asian elephants, like African elephants, mourn their dead calves? And the answer is yes, and it is loud. The vocalizations from the elephants lasted between 30 and 40 minutes, but only in places far from human settlements.
They point out that this behaviour suggests elephants distinguish human spaces from non-human spaces to avoid disagreements. They also mention that elephants limited vocalisation to the burial phase.
The increasing encroachment of human activities into natural habitats and the resulting environmental degradation are forcing elephants to venture into human-dominated areas in search of food and other ecological necessities. This interaction has led to new behaviours in these majestic creatures.
Asian Elephants’ mourning behaviour
Parveen Kaswan, an officer with the Indian Forest Service, and Akashdeep Roy, a researcher at the Indian Institute of Science Education and Research, spent 16 months reviewing literature relating to elephant burials. They found five case reports that document this behaviour.

Researchers have revealed that Asian elephants, similar to their African counterparts, engage in what we can describe as mourning rituals. Observations showed them vocalising loudly and burying their deceased calves, exhibiting a level of ritualistic behaviour that parallels human funeral rites.
The study reports a heartbreaking journey of a mother elephant. The mother elephant carried her dead calf for two days before letting it go. This extended time of grieving shows the deep attachment between mother elephants and their offspring. This could have been made stronger possibly by hormonal influences like oxytocin and the long gestation period elephants experience. This response is consistent with other studies on chacma baboons, olive baboons, African elephants and Thornicroft’s giraffes.
As per the study, the burial process is a collective effort, involving not only the mothers but also other females within the herd who act as surrogate caregivers, as well as elephants of various ages. This communal participation underscores the intricate social fabric of elephant herds and their collective mourning when faced with death. Notably, this ritualistic burial is reserved exclusively for the young. The physical impracticality of carrying the larger, heavier adults precludes them from receiving the same rite. This selective practice indicates that the elephants’ mourning and burial customs are particularly significant for the young, whose passing deeply impacts the social structure of the herd.
Compassionate behaviour
The research aimed to understand the ‘perimortem’ strategy and ‘postmortem’ behaviour of Asian elephants. The main evidence shows that someone or something transported the corpses from afar, treated with great care. They buried the corpses in preferred locations, always in a specific posture, which was an unusual lying position with legs upright.
The author said, “Our study found an interesting thing – the placement of carcasses with their paws raised in narrow irrigation drains. This strategic behaviour shows the care and affection of herd members toward the deceased animal and suggests that in a potential crush situation, pack members prioritize the head over the feet,” they highlight.”
“Elephants are social and affectionate animals and, based on an external examination of the carcasses, we also suggest that herd members gently placed the dead calves by grasping one or more legs,” the experts conclude.
The authors of the report thoroughly investigated the underlying reason for the death of the offspring through postmortem examinations. One of the conclusions is that there was no direct human intervention in any of the five deaths.

“Through direct and indirect evidence, this study highlights compassionate and helpful elephants’s behaviour during carcass burial. Asian elephants transport their deceased calves to isolated places, away from humans and carnivores, while searching for drains irrigation and depressions to bury the body,” the report states.
No infanticide among Asian elephants
Many animal groups, such as monkeys, meat-eaters, and rodents, commit infanticide or baby killing. Different reasons, such as elimination of competition, scarcity of resources, or maintaining social order within a group, contribute to this phenomenon.
However, the researchers found that there was no infanticide among the Asian elephants. They believe there are a few reasons why elephants don’t kill babies:
- Elephants, particularly females and their young, live in close family groups forming strong bonds. This closeness possibly prevents them from hurting the young, actively encouraging them to cooperate in caring for them.
- Baby elephants require long term care from their mothers and other females in the herd. This extended care and help from everyone might decrease the likelihood of someone killing a baby.

- In the breeding process, elephants reproduce without having to kill their babies to quicken the mother’s readiness for another offspring. Unlike some other animals, the mother cannot immediately have another offspring if she loses a baby. Thereby, eradicating the need for males to kill babies.
- Male elephants neither directly contribute to raising the babies nor participate in the close female groups. They prioritize finding females ready to mate rather than assuming control over a herd and eliminating other males’ babies. This social structure and breeding style decreases the likelihood of elephants killing babies.
Complete Article ↪HERE↩!
Irish committee to recommend laws for assisted dying
— Proposed legislation would allow people help with ending their lives under certain medical conditions

An all-party parliamentary committee in Ireland is to recommend that legislation be introduced to allow for assisted dying if a person has a terminal illness or has only a short time to live.
A majority on the Oireachtas committee on assisted dying supported the proposal that the law be changed to allow someone to get assistance to end their life if they have between six and 12 months to live.
The legislation would apply to people who have been diagnosed with an illness or a medical condition that is “incurable, irreversible, progressive” and at an advanced stage that will cause death within six months.
It is expected that the time limit for those with a neurodegenerative condition would be extended to 12 months.
The committee’s report is to be published on 20 March but has now been agreed by a majority of representatives from all sides of the Irish parliament. After its publication it will go to government for further consideration.
It is unclear whether the three-party coalition government led by Leo Varadkar is prepared to introduce legislation to enact the recommendation before a general election expected this autumn.
If it does, Ireland will join other countries including Switzerland, Belgium, Canada and the Netherlands in allowing assisted dying under certain circumstances.
It is understood that the proposed Irish legislation would require two doctors to sign off on a person’s incurable and life-threatening condition.
At hearings representatives of the Christian churches and a Muslim cleric voiced their opposition to the legislation, saying it was morally wrong to kill someone and was against God’s will.
Some psychiatrists also argued it could lead to “a slippery slope” with increasing numbers seeking to end their lives.
But the committee’s recommendation has been welcomed by the chair of the advocacy group End of Life Ireland.
Janie Lazar said: “We’ve been working hard to get people talking about assisted dying and about the choices that should be available to those who have no time to wait or waste.”
Constitutional law experts say they are confident that the committee’s recommendation would not require a referendum but a simple law change.
Nathan Stilwell, assisted dying campaigner for Humanists UK, welcomed the “bold move”, comparing it favourably with the debate in Britain where a report by MPs last month did not recommend a vote on the issue.
“Well done to the Irish special Oireachtas committee on assisted dying for taking an evidence-based and compassionate approach. It’s brilliant to see such a bold move after just a week ago a Westminster committee did not vote for any change in the law,” said Stilwell.
Complete Article ↪HERE↩!
Death doulas
— Helping people at the end of their life

You may have heard of a birth doula – someone who provides non-medical support and advocacy throughout pregnancy, birth and after the baby has been born. More recently, so-called death doulas – people who assist at the other end of the lifespan – have been growing in popularity.
The role of death doulas is still relatively new, so the terminology and definitions of what they are based on what they do are in flux. They are sometimes referred to as an end-of-life doula, soul midwife, death coach, dying guide, death midwife and palliative care doula. The actual term used is often down to the preference of the practitioner and how they define their work, as well as cultural norms within the country they work in.
Death doulas are known to work in Brazil, Canada, the Czech Republic, Germany, Ireland, Italy, Japan, New Zealand, Russia, the UK and the US. They tend to provide support to people with life-limiting or terminal illnesses, focusing on improving both the quality of life and the quality of death someone experiences. This can include helping with funeral plans, talking about the processes involved around death, or helping someone with their care appointments.
Sometimes, the doula’s contribution is simply about being next to the person and providing company.
The work of a death doula can extend beyond the dying person. They can provide emotional and social support to family, friends and even neighbours – typically the informal carers and social network surrounding the dying person.
Doulas help those close to the dying person with the impending loss (so-called anticipatory grief). Some also carry out errands and chores to enable them to spend time with the dying person. They may also continue to visit those people after the death to support them as they grieve. Crucially, death doulas can enhance the links between professionals and the social support around a person by helping with communications and advocacy work.
Filling the gap
With healthcare systems and informal carers typically stretched beyond capacity, death doulas can provide a means to fill the gap and provide personalised attention. Someone can access doula support either privately or, depending on the doula, through voluntary means.
My colleagues and I recently examined how end-of-life doulas can be provided by the NHS. It noted that the flexibility of the services doulas can provide was not only helpful for the dying person but also for the wider healthcare system. It helped people who may otherwise not receive support due to service gaps, strict referral criteria, or lack of social support.
Beyond supporting individuals, some death doulas see community engagement as core to their role. They are keen to share information about the dying process and grief with others. They may host workshops or death cafes. Across this work, their contributions are to normalise talking about death, dying and loss in society.
Anyone can become a death doula, and it is not currently a regulated profession. There is a wide range of doula training available internationally, including online, provided either by individual doulas or by organisations such as Living Well Dying Well.

Personal experience
In addition to their doula training, doulas bring their own professional and personal experience to the role. International research on death doulas has noted that many who have become death doulas have a background in professional healthcare, social care or education, and may already have some experience with death.
Those who have trained to be a death doula can be eligible to join a community of practice. Within the UK, End of Life Doula UK is a membership organisation for doulas, setting standards for doula practice and representing doulas. Similar organisations exist globally, including the International End of Life Doula Association.
Death doulas are not a replacement for specialist palliative care and cannot prescribe drugs. Their role is to support people in having a good death.
The growing demand for death doulas is one example of how society is questioning what a good death can be and how to make it happen. Other examples include discussions about assisted dying and improving death literacy. Rather than consider death a societal taboo, there is a growing recognition that people want to value the end of life and reshape how it is experienced.
Death doulas can play a pivotal role in supporting a dying person and those around them. Their support can be emotional and practical, often bridging the gaps in existing support or helping to signpost to relevant services. Not everyone may want a doula, but those who do may see it as someone who can guide them through a significant life process.
Complete Article ↪HERE↩!
